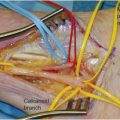
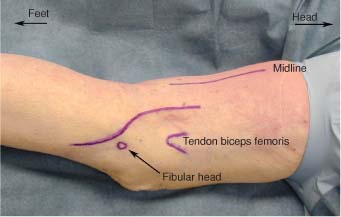
12 The common peroneal nerve originates as the smaller, lateral, terminal branch of the sciatic nerve. Its fibers are derived from the dorsal divisions of the ventral rami of the fourth and fifth lumbar nerves and the first and second sacral spinal nerves. Most commonly dividing from the sciatic at the distal third of the thigh, it then moves obliquely across the distal thigh to travel on the lateral aspect of the popliteal fossa. There it is overlapped by the medial margin of the biceps femoris muscle. Close to its origin one or more branches of the peroneal nerve leave to contribute to the formation of the sural nerve. The tibial nerve also contributes to the formation of the sural nerve. Moving distally, the nerve then crosses the lateral head of the gastrocnemius muscle to reach the area just posterior to the fibular head. After it curves over the posterior rim of the fibular head, it enters a tunnel formed by the two heads of the peroneus longus muscle and the fibular neck. The superficial head of the peroneus longus muscle arises from the tibial plateau, and as it crosses the fibular head it has a fibrous border that forms the superficial portion of the tunnel through which the common peroneal nerve passes. The fibrous origin of the deep head of the peroneus longus and the fibular neck form the deep portion of this tunnel. In this area, not only is the nerve tethered by this fibrous tunnel, it also increases its number of fascicles by twofold.1 This combination of increased structure in an area of anatomic narrowing makes the nerve especially vulnerable to entrapment and compression injuries at this location. Just before dividing, the common peroneal gives off three articular filaments to the knee and helps to supply the superior and inferior lateral genicular and anterior tibial recurrent arteries. It also gives off the lateral sural cutaneous nerve, which supplies sensation to the skin and fascia on the lateral surfaces of the leg. The common peroneal nerve, just beyond the fibular neck and underneath the peroneus longus, divides into superficial and deep branches. At this point its fibers are at risk for compression from the fibrous arch of the origin of the extensor digitorum longus muscle. The superficial portion of the nerve takes a relatively straight course to innervate the peroneus longus muscle and continues descending distally to innervate the peroneus brevis muscle. These muscles control foot eversion. In the distal third of the lower leg it becomes more superficial and lies between the peroneal tendons and the lateral edge of the gastrocnemius muscle. Near the lower border of the inferior extensor retinaculum (just superior to the ankle) the nerve splits into two dorsal digital nerves, which supply sensation to the medial and dorsal aspects of the dorsum of the foot and the great toe. The deep peroneal nerve supplies a branch to the tibiofibular joint. Once past the neck of the fibula and after passing beneath the fibrous lateral edge of the peroneus longus, the nerve gives off geniculate branches and branches to the tibialis anterior. The tibialis anterior muscle is responsible for foot dorsiflexion. These branches also contribute to further tethering of the deep peroneal nerve. The nerve descends in the anterior compartment of the leg lateral to the tibialis anterior and at first is medial to the extensor digitorum longus and the extensor hallucis longus and also innervates both of these muscles. In its downward course the nerve first lies lateral to the anterior tibial vessels, then anterior to them, and finally lateral to them again in front of the lower end of the tibia and ankle. In the very distal leg the nerve divides into medial and lateral terminal branches. In the leg the nerve sends branches to the tibialis anterior, extensor digitorum longus, extensor hallucis longus, and peroneus tertius muscles, an articular branch to the ankle, and filaments to the anterior tibial vessels. The medial terminal branch gives rise to a dorsal digital nerve, which splits to supply sensation to the contiguous sides of the first and second toes. The lateral terminal branch curves outward beneath the extensor digitorum brevis and supplies this muscle, the adjacent tarsal and tarsometatarsal joints, and the dorsal interossei muscles of the foot. The nerve also supplies sensation to a small portion of skin over the first dorsal web space of the foot. After intubation and induction of general endotracheal anesthesia on a stretcher, the patient is placed on the operating table in the prone position on abdominal bolsters. The arms may be either tucked to the side or brought forward on an arm board. A small bolster is placed beneath the ipsilateral hip to turn the lateral surface of the leg into a more visible position. Alternatively, some have advocated operating with the patient in the supine position with the knee flexed; I find this positioning awkward and less amenable to gaining proximal exposure of the nerve, should it be required. The peroneal nerve may also be operated on in the lateral position. The midline of the popliteal fossa and just superior to it should be marked. The biceps femoris tendon can usually be palpated in the lateral aspect of the popliteal fossa, and this should also be marked. Lastly, the fibular head, on the lateral aspect of the leg, should be palpated and marked. The skin incision is laid out so that the proximal end is just superior to the popliteal fossa. In the mediallateral direction it lies midway between the biceps femoris tendon and the midline of the fossa. Some would advocate moving the incision more laterally, closer to the tendon of the biceps femoris. However, by placing the incision midway between the tendon and the midline, a more proximal exposure of the lower portion of the sciatic nerve may be accomplished more easily, if required. If there is difficulty locating the common peroneal nerve due to scaring or anatomic disruption, the incision may be extended to the midline and the sciatic nerve located. The sciatic can then be traced distally into its common peroneal/tibial bifurcation. The incision should then move distally in a gentle curve to cross the lateral aspect of the fossa obliquely and posteroinferior to the fibular head. The incision purposefully crosses the joint space obliquely so as to avoid adhesions or contractures that occur in scars that cross a joint space in a straight line. Finally, the incision should curve toward the anterior compartment of the leg where it may be extended as needed to facilitate distal exposure of the nerve (Fig. 12-1). The skin is infiltrated with a 1% lidocaine with epinephrine 1:100,000 solution and then incised. Care should be taken in making the skin incision, particularly around the fibular head, because the nerve is surprisingly superficial. Once the skin incision is complete, skin flaps are developed to either side of the incision (Fig. 12-2). Care should be taken if possible to avoid injuring the terminal branches of the posterior cutaneous nerve of the thigh, which may be encountered in some patients at this level (Fig. 12-3). Once the skin is open and the skin flaps developed, a layer of fat is then visualized just medial to the biceps tendon. The nerve should then be found embedded in the fat just deep to this layer (Fig. 12-4). Attention should be given to unequivocally identify the nerve because it may occasionally be mistaken for the biceps femoris tendon. Once located, the nerve should be dissected free circumferentially with a right-angle clamp and then encircled with a narrow Penrose drain or a wide vessel loop (Fig. 12-5). The nerve may then be followed along its course, releasing any fibrous tissue attachments. As the nerve is followed distally beyond the popliteal fossa, a thick fascial covering is encountered that is contiguous with the fibrous lateral edge of the peroneus longus muscle. This edge should be incised to reveal a portion of the muscle (Fig. 12-6). This muscle may also be incised to further expose the nerve distally (Fig. 12-7). Dissection should continue to fully expose and identify both the superficial and deep branches of the nerve (Fig. 12-8). The deep branch must be traced around the neck of the fibula and freed (Fig. 12-9). When operating in the vicinity of the fibular neck some advocate removing the posterior portion of the proximal part of the fibula with a rongeur so that the course of the nerve from posterior thigh to anterior compartment is left less angulated and relatively more relaxed than in its preoperative state.2 When identified the head of the fibula may be removed with a rongeur (Fig. 12-10). Fine neural branches going to the knee joint may also be sacrificed to gain length and greater relaxation along the course of the deep branches. The superficial branch travels on distally in a more straight line and may be traced along its path. The deep branch may be traced as far as the intermuscular septum (anterior crural septum) where it crosses over into the anterior compartment and then travels distally in the leg (Fig. 12-11).
PERONEAL NERVE
ANATOMY
POSITIONING AND SURGICAL EXPOSURE
In Leg
Peroneal Nerve
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree