CHAPTER 57 Periprosthetic Hip Fractures
Periprosthetic hip fracture is a severe complication of total hip arthroplasty (THA). Surgical treatment of such fractures is a challenge, as it is often accompanied by fracture comminution, bone deficiency, and femoral component loosening. Of 1049 periprosthetic femoral fractures recorded in the Swedish National Register, 23% required reoperation and 18% developed postoperative complications.1 Periprosthetic hip fracture is associated with poor functional outcome, increased morbidity, and a high incidence of mortality, as well as with elevated economic burden.
Periprosthetic fracture is increasingly prevalent; it has been estimated to range from 0.1% to 3.2% for primary uncemented total hip arthroplasties and from 3% to 12% for revisions performed with or without cement. Factors associated with this increase include a broadening of THA indications, a growing population of hip joint replacement recipients, increased use of uncemented implants, and an increasing population of revision recipients. Roughly 5% of revisions performed are for periprosthetic fracture, making it the third most frequent reason for revision of primary total hip replacements. Periprosthetic fracture as a reason for revision is currently less common than either aseptic loosening or sepsis and has the same frequency as dislocation.2
RISK FACTORS
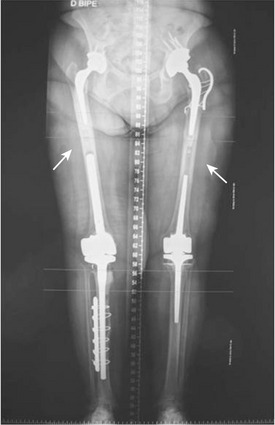
Patients at risk for intraoperative fracture include those with osteoporosis, osteopenia (as in rheumatoid arthritis), altered bone morphology or deformity (as seen in Paget disease), developmental dysplastic hip, and old proximal femoral fractures.3 Local risk factors include cementless stems (especially in revised settings), impaction bone grafting in revision procedures, minimally invasive techniques, under-reaming of the femoral cortex, use of large-diameter femoral stems, and a low ratio of femoral cortex diameter to canal diameter.4 Risk factors for postoperative periprosthetic fracture include osteoporosis, osteolysis, cortical perforation, loose femoral implants, and ipsilateral hip and knee revision arthroplasty that produces two stress risers in the isthmus of the femoral diaphysis (Fig. 57-1).5
CLASSIFICATION OF FEMORAL FRACTURES
Many classifications of periprosthetic fractures are reported in the literature. Classifications provide information about the site of the fracture; they are also of value in determining treatment strategy. The Vancouver Intraoperative and Postoperative Classification, proposed by Duncan and Masri,6 is the most widely used system. The system is simple, reproducible, and validated, as well as being useful in formulating treatment strategies. It takes into account the site of the fracture, the stability of the implant, and the condition of surrounding bone stock: the most important factors for making the decision regarding the optimum course of treatment. The Vancouver Intraoperative Classification can be used to guide management of intraoperative fractures, although its reliability and validity in such situations have not been as widely documented.
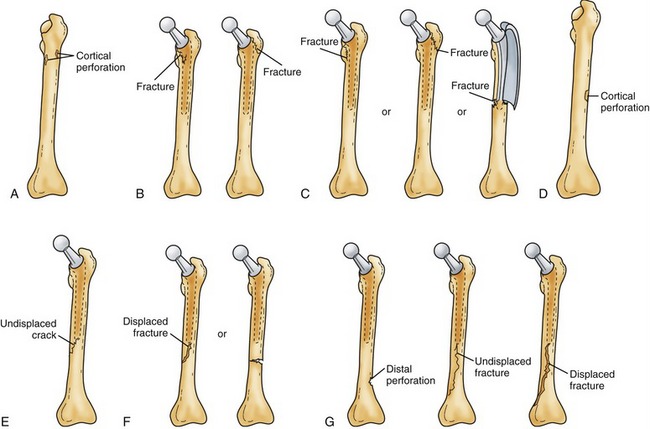
Vancouver Intraoperative Fracture Classification
The Vancouver system takes into account fracture location, pattern, and stability, dividing fractures into three types. Type A involves the proximal metaphysis (trochanteric area); Type B is diaphyseal (tip of the stem); Type C is distal to the stem tip and not amenable to insertion of the long revision stems. Each type is further subclassified as either subtype 1 (in which there is only cortical perforation), subtype 2 (nondisplaced crack), and subtype 3, with a displaced and unstable fracture pattern (Fig. 57-2).4
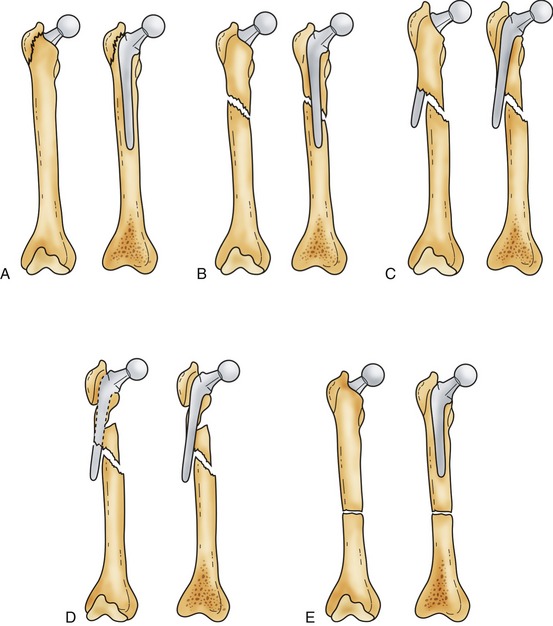
Vancouver Postoperative Fracture Classification
The site of the fracture, stability of the prosthesis, and quality of the bone stock determine fracture severity (Fig. 57-3). In type A, the greater or lower trochanter is affected. Type B fractures are those at or just distal to the stem tip. Type B has three subtypes: B1, in which the prosthesis is stable; B2, in which there is a loose prosthesis but adequate bone stock; and B3, in which the prosthesis is loose and there is marked proximal bone loss or damage to a degree that a standard revision component will not be supported. Type C fractures are well distal to the stem tip.
MANAGEMENT OPTIONS
Femoral Intraoperative Fractures
Goals of treatment include the following:
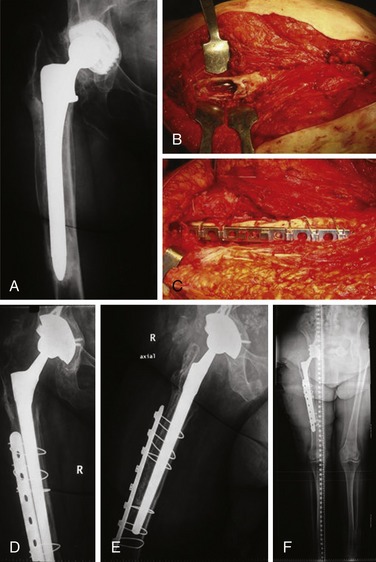
Type B1: Diaphyseal Cortical Perforation
Diaphyseal cortical perforation is most commonly caused by incautious use of cement removal devices or reamers during canal preparation.7 If a diaphyseal cortical perforation is detected, it should be bypassed by a distance of two cortical diameters, using a longer stem. Before stem insertion, consideration should be given to cerclage fixation of the bone at or below the perforation to prevent crack propagation. If the perforation is at the tip of the longest stem, it should be bypassed with a cortical strut or plate; such a perforation should also be cancellous bone grafted at the time of strut or plate insertion and fixation (Fig. 57-4).