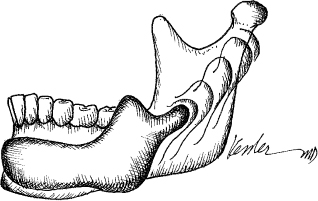
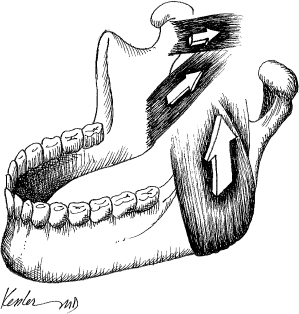
9 The majority of diseases affecting the upper and lower jaws of children are benign.1 Consequently, the surgical resection of such diseases requires only narrow margins and, in turn, commonly necessitates minimal reconstruction. In some cases, however, larger resections resulting in a significant deformity may be necessary to obtain appropriate disease-free tissue margins. In cases that result in a significant bony defect, the options for reconstructing the jaw include nonvascularized bone grafts and vascularized composite flaps. For select defects, nonvascularized bone grafts may provide a simple method of bony reconstruction, assuming the surrounding tissue bed is well vascularized and the patient has a good nutritional status. Occasionally, however, the patient has been previously exposed to chemotherapy or radiation, or has sustained a significant bony defect, requiring a vascularized bone flap. A variety of childhood diseases may affect the mandible or maxilla; however, sarcomas are the most common form of malignancy.2 Although surgical resection plays an important role in the treatment of this disease, most often these patients have been previously treated with chemotherapy, radiation, or combination therapy. As a result, the recipient bed is often compromised with regard to healing,3,4 thus limiting the application of adjacent tissue transfer or nonvascularized bone grafts. Although strategies to minimize the effect of chemotherapy and radiation on the healing of soft tissue and growth of the craniofacial skeleton have been investigated,3 under these circumstances free vascularized tissue remains the most reliable source of bone and soft tissue. When a surgical resection of the pediatric patient is indicated, prompt reconstruction is essential to both long-term psychological well-being5,6 and normal craniofacial development.3,4 Over the last decade, there has been a trend to embark on early surgical reconstruction of children with craniofacial disorders, which has resulted in a series of reports investigating the role of surgical reconstruction on psychological development.5,7 Many of these studies were prompted by a common anecdotal experience among reconstructive surgeons that children who underwent early reconstruction of craniofacial deformities seemed to socialize postoperatively with their peers and their parents in a more positive way than did their unreconstructed counterparts. Early studies by Pertschuk and Whitaker8 supported these experiences, demonstrating an increase in self-esteem and peer acceptance following surgery. Examination of the long-term effects of facial disfigurement on social development has demonstrated convincing evidence that attractiveness plays a definitive role in normal socialization patterns, and that children with unreconstructed craniofacial deformities are more prone to an inhibited personality style, low self-esteem, and impaired peer relationships.9 It has been postulated that these children harbor a poor self-image at an early age, resulting in the development of antisocial behavior in adolescence.9 Similarly, it has been suggested that adults have lower expectations of disfigured school-age children, leading to underachievement, social withdrawal, and occasionally depression.10 When early surgical intervention occurs, however, these children tend to psychosocially adjust in a rather short period of time. Commonly, both peer and family interactions occur more naturally as these children resolve their avoidance disorders.5,6,8 In addition to a healthy psychological development, a normal physical development is important in the lives of these patients. Although mandibular and maxillary reconstruction in children is uncommon, when faced with this challenge it is essential that special consideration be given to issues related to the growing child, so that the goal is to achieve optimal restoration of mastication, deglutition, and cosmesis. Similar to reconstruction of the adult mandible, bone stock, soft tissue, and skin paddle design are important factors in addressing the specific reconstructive requirements of the patient. In contrast to the adult patient, however, the pediatric patient is growing. Because of this characteristic unique to this population, surgical reconstruction of the upper and lower jaws requires an understanding of the changes in bone and soft tissue architecture at both the donor site and the mandibulofacial complex as a result of growth and development. The commonly used donor sites, including fibula, iliac, and scapula, all possess growth centers, areas of the bone that monitor and regulate growth and development. Disruption of the growth center as a result of bone flap harvest can lead to abnormal development and long-term functional consequences. Understanding the anatomic location of these growth centers and their role in normal development is essential to preventing long-term functional deficits. In the adult patient, the selection of a donor site is based on factors such as the requirements of the defect and the patient’s comorbidities.11 The pediatric patient, however, is usually healthy and in good nutritional status. Although issues related to tissue requirements for restoration of the defect are important in choosing a donor site, there is an additional parameter that is of critical importance: the longterm development at the reconstructed site as well as the donor site. Normal craniofacial development, including growth of the mandible and maxilla, results from a series of complex mechanisms that have been the focus of intense debate among investigators and clinicians. Facial growth is a dynamic process that Enlow12 refers to as the “ongoing equilibrium” that exists among the skull base, muscle stress, and occlusal relationships. After birth, the pediatric craniofacial skeleton grows through two distinct mechanisms: epiphyseal proliferation and bone remodeling. Epiphyseal proliferation is largely responsible for increases in bone length and projection (Fig. 9.1), a process that is dominant during the first 18 years of life. After age 18 the epiphyseal plate of the mandible, which is located in the proximal zone of the conical subcondylar ridge, fuses. Consequently, the majority of the longitudinal growth in this region is complete. Prior to fusion, however, the epiphysis exists as a three-dimensional structure responding to the influence of the surrounding soft tissues, traction forces of the muscles of mastication, and the condylar relationship with the cranial base. During the course of facial skeletal development, the mandibular epiphysis adapts the intercondylar distance to the widening cartilaginous synchondrosis of the cranial base, highlighting the ever-important relationship between normal mandibular growth and normal basicranial development. A disruption of the epiphysis, the muscles of mastication, or the temporomandibular joint prior to the fusion of the epiphyseal plate, can result in abnormal mandibular projection and malocclusion.13 The role of epiphyseal growth, particularly in the prepubescent pediatric patient, cannot be overemphasized; however, a second mechanism of bone growth called remodeling, plays an equally important part in mandibular contour and symmetry. In contrast to epiphyseal growth, remodeling is a process that occurs both during the prepubescent period and throughout adulthood. Adjustments in the downward and forward projection of the mandible occur through deposition of bone at the posterior margin of the ramus along with corresponding resorption at the anterior margin.12 Likewise, mandibular contour and increased width occur as a function of buccal bone deposition and concomitant lingual resorption. The two simultaneous processes of epiphyseal growth and bone remodeling occur in different areas within the same bone simultaneously, and there is no histologic difference in new bone created by either process. Although epiphyseal fusion occurs in early adolescence as part of a genetically preprogrammed process, remodeling continues throughout adult life largely in response to the mechanical stress applied by the muscles of mastication (Fig. 9.2).14–16 Understanding these principles is important in surgical reconstruction because disruption of the mandible prior to epiphyseal fusion may result in a different long-term developmental abnormality from a similar surgical disruption after epiphyseal fusion. Furthermore, it is important to recognize that girls reach mature mandibular height and depth at a mean age of 13, on average, which is 2 to 5 years earlier than do boys. The maxilla serves as the infrastructure of the midface; however, it also plays an important role during facial development by providing an occlusal surface for the mandible. This occlusal relationship functions as a feedback loop that helps to guide both midface and mandibular development. The ultimate form of the midface is a result of two separate but related processes. The first is referred to as primary displacement, or growth of the maxilla bone itself, and the second is secondary displacement, or movement of the maxilla as a result of growth of the surrounding articulating skeleton.12 Primary displacement results from the genetic propensity for the maxillary bone to enlarge as a child ages, therefore contributing to vertical maxillary growth. During this process, periosteal resorption occurs on the nasal side of the palate, whereas periosteal deposition occurs on the oral side of the palate. This leads to a downward projection of the maxilla and an enlargement of the nasal chambers. Normal maxillary width occurs as a result of bony accretion at the suture lines and resorption at the lateral nasal wall. Secondary displacement is characterized by growth of the surrounding craniofacial skeleton, namely the skull base and the mandible, which serve to further displace the maxillary complex downward and forward. Normal dental occlusion acts to guide maxillary projection and preserve both the cosmetic and functional harmony of the midface. Although primary and secondary displacement are essential to normal maxillary growth, a third mechanism is equally important in the development process. The traction forces associated with the muscles of mastication and the axial loading forces associated with mastication also contribute to the development process. A disruption in any or all of these growth mechanisms prior to skeletal maturation inevitably leads to a morphologic change in maxilla. Vertical maxillary growth is normally complete by age 14 in girls and age 16 in boys, and fusion between the palatine processes and the maturation of maxillary width occurs at 18 years of age. Much of what is known about facial development after ablative surgery is derived from experimental animal models.17 It is clear, however, that disruption of the developing maxilla or the maxillary suture lines prior to fusion will significantly affect midface development. When disruption of the pediatric midface hinders normal occlusal contacts, there may be a profound effect on both mandibular and maxillary development. Occlusal contact provides bone stress, a key component to the induction of bone growth; therefore, the occlusal interaction between the maxilla and the mandible is paramount to ensure normal craniofacial development. It is for this reason that unreconstructed defects of the pediatric maxilla can lead to significant disturbances in facial growth and aesthetic form. Although the developmental implications of performing a surgical ablation on a pediatric patient may be profound, if careful consideration is not given to the reconstruction, the morbidity associated with a donor-site harvest may be equally disturbing. Three donor sites have been applied to pediatric mandibular and maxillary reconstruction: the fibula, the scapula, and the iliac crest.18,19
Pediatric Head and Neck Reconstruction
♦ NORMAL DEVELOPMENT OF THE UPPER AND LOWER JAWS
DONOR-SITE SELECTION
The Fibular Donor Site
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree