(1)
Department of Dermatology, Drexel University, Philadelphia, Pennsylvania, USA
Abstract
Pathologic specimens of flexural, facial-extensor, and nummular eczema are represented here. Also represented are the mycotic form of eczema, seborrheic eczema, dyshidrotic eczema, granular parakeratotic eczema, and Doucas Kapetanakis disease.
Keywords
Congo redDoucas Kapetanakis diseaseDyshidrotic eczemaFacial-extensor eczemaFlexural eczemaGranular parakeratotic eczemaHematoxylin and eosinMycotic eczemaNummular eczemaPathologyPeriodic acid–SchiffSeborrheic eczemaThe clinical photographs in this chapter representing sites from which the biopsies were taken are similar to the sites from which the microbiological cultures were taken (Chap. 2). Hence, flexural, facial-extensor, and nummular eczema are well represented. Also represented are the foot in the mycotic form of eczema (Fig. 3.1), the face in seborrheic eczema (Fig. 3.2), and the distal extremities in dyshidrotic eczema (Fig. 3.3). The axilla was biopsied in cases of granular parakeratotic eczema (Fig. 3.4), and the leg in Doucas Kapetanakis disease (Fig. 3.5).

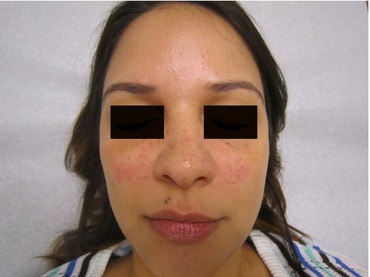




Fig. 3.1
Mycotic form of eczema. Hyperkeratosis and maceration are present in the fourth interdigital toeweb space. Diffuse xerosis and nail changes are also present
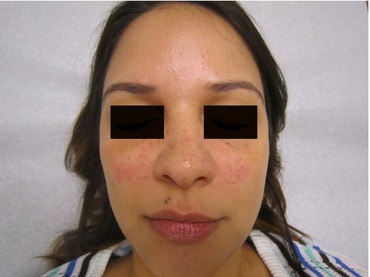
Fig. 3.2
Seborrheic eczema. Pink patches/plaques are present on the bilateral cheeks. Mild scaling is present in the eyebrows and along the lateral hairline (not visible). Small closed comedones (of acne) are also present

Fig. 3.3
Dyshidrotic eczema. On the fingers and wrist, there are lichenified, hyperpigmented plaques. Small vesicles are seen on the index finger and thumb

Fig. 3.4
Granular parakeratotic eczema. In the axilla, there is a mildly scaling, hyperpigmented plaque. Small hyperpigmented papules are present along the borders of the larger plaque

Fig. 3.5
Doucas Kapetanakis eczema. On the mid and lower shin is a red-brown, scaling plaque. “Cayenne pepper” macules are present around the plaque
In patients in whom the diagnosis was in doubt clinically, causing us to question, “Is this psoriasis or eczema?” (Fig. 3.6), cases diagnosed as eczema on pathology tended to be “nummular” clinically, inasmuch as the flexural and facial-extensor forms were generally much more readily recognized clinically.


Fig. 3.6
On the leg, there is a scaling pink plaque. Xerosis is present also. The clinical differential diagnosis includes psoriasis and nummular eczema among others
The microscopic pathology in eczema has changed little in many decades and has never had specific features to make the diagnosis with certainty. In fact, many pathologists would label a slide acute, subacute, or chronic dermatitis as a final diagnosis, and these renderings could potentially be interpreted as any inflammation of the skin ranging from contact dermatitis to seborrheic dermatitis.
The features noted in eczema have included parakeratosis, irregular acanthosis, spongiosis, intraepidermal micro- and macrovesicles, exocytosis, perivascular and adventitial lymphocytes, and eosinophils (Fig. 3.7) [1]. All these would be found to varying degrees and rarely would be present together. Spongiosis, however, was (and is) the hallmark feature of eczema and its presence was most important. Spongiosis itself is characterized by fluid in the epidermis leading to separation of the cells. When greater amounts of fluid are present, vesicles are noted. Even in the most chronic forms of the disease, where there is marked epidermal thickening, focal spongiosis can be noted.
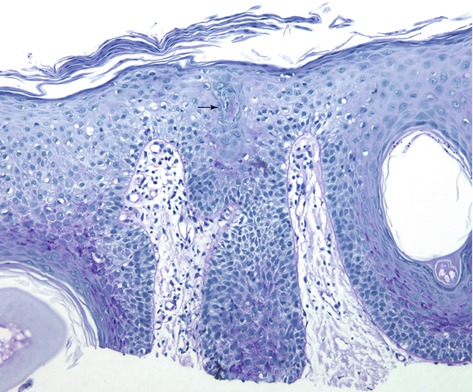
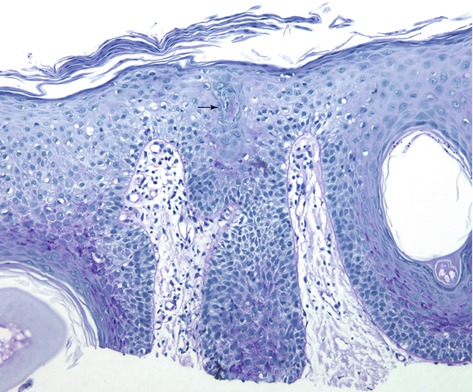
Fig. 3.7
Skin specimen stained with periodic acid–Schiff, showing separation of the epidermal cells (spongiosis). There is also a periodic acid Schiff–positive occlusion of the sweat duct (arrow)
We recently added a newly recognized form of eczema, lichen planus–like eczema, to the differential list of spongiotic diseases [2]. This list included atopic dermatitis, contact dermatitis (both irritant and allergic), seborrheic dermatitis, and others. The emphasis of our work was to tie the pathology to this variant of eczema and to exclude lichen planus (which it resembled clinically) and other histologically dense infiltrates in the upper dermis. Consequently, the spongiosis in a clinicopathologic correlation added considerably to the fact that this disorder was a variation of eczema similar to the major variations classified as flexural, facial-extensor, and nummular. Further, there was no dense upper dermal infiltrate noted (this excluded “true” lichen planus).
Spongiosis, however, is not specific even though it may help exclude other disorders with differing pathologies. Until now, occlusion of eccrine sweat ducts has been specific only for miliaria. Even in miliaria, the sweat-duct blockage may not be apparent if the pathology specimen is secured late in the life of the lesion (when inflammation obscures it) [3]. Hölzle and Kligman [4




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








