Chapter 33 Parasitic infestations
1. Where and how does one acquire cutaneous parasitic diseases?
Parasitic skin diseases may arise from systemic spread or direct penetration of the skin. Cutaneous parasitic infestations are a major source of morbidity, affecting millions worldwide. Tropical climates, crowding, poor nutrition, sanitation problems, and limited medical resources are all associated with increased variety and severity of parasitoses. Ecologically temperate climates and industrialized societies are also afflicted by significant parasitic infestations because of local vectors, distant vacations, and widespread travel to and from areas of endemic infection for business, political, humanitarian, or military purposes. Immunosuppression due to drugs or disease leads to cutaneous manifestations of parasitic diseases that may be caused by unusual organisms.
2. What is “creeping eruption”?
Properly known as cutaneous larva migrans, and popularly known as “sandworms,” creeping eruption occurs when the larva of dog and cat hookworms (Ancylostoma caninum and A. braziliense, respectively) penetrate intact, exposed skin and begin migrating through the epidermis. The most common location for the eruption is the sole of the foot, although other sites such as the buttocks, back, and thighs, which may have rested on contaminated sand, are susceptible. Lacking the enzymes necessary to penetrate and survive in the deeper dermis, the larvae wander a serpiginous route at a speed up to 3 cm/day. Clinically, the primary lesion is a pruritic, erythematous, serpiginous burrow (Fig. 33-1). Although the larvae usually die in 2 to 8 weeks, survival up to 22 months has been reported. Several cases of cutaneous larva migrans–related erythema multiforme have been reported.


Figure 33-1. Creeping eruption. Cutaneous larva migrans due to canine hookworm.
(Courtesy of the Fitzsimons Army Medical Center teaching files.)
3. How do you treat creeping eruption?
An older method was to freeze the leading point of the burrow. This sometimes produced significant tissue destruction and often missed the larva, which may be up to 2 cm ahead of the visible burrow. A classic treatment is 10% topical thiabendazole suspension applied four times a day for at least 2 days after the last sign of burrow activity; however, this medication is not always readily available. This regimen has a high cure rate and minimal toxicity. Rare cases may require oral thiabendazole. Oral ivermectin, indicated for the treatment of larval currens, may have a role in the treatment of this disease as an off-label use.
4. What is different about larva currens?
Larva currens, or “racing larva,” is caused by Strongyloides stercoralis, a nematode with a normal life cycle similar to the hookworm. Strongyloides, however, is unique in that it can complete its life cycle within the human host and bypass the obligate soil phase of the hookworms. Autoinfection may occur to a point of overwhelming infestation and host death, especially in immunocompromised victims. The serpentine eruption of larva currens appears much the same as creeping eruption but is more likely to occur on the thighs, buttocks, or perineum due to larval penetration from the nearby colon. The eruption is more fleeting and lasts no more than a few days, during which the larva’s migratory speed through the dermis may be clocked at up to 10 cm/hr (Fig. 33-2). A nonspecific rash or hives may also occur because of hypersensitivity to the parasite.
5. Are there other nematode infestations that cause skin disease?
Enterobius vermicularis (pinworms) may cause a noisome perianal itch, but secondary complications including dermatitis, bacterial infections, and local abscesses can develop. Treatment is a single dose of mebendazole. Trichinella spiralis, which is acquired by eating undercooked pork, may cause a diffuse rash, nail bed splinter hemorrhages, and a subtle but persistent periorbital edema (trichinosis).
7. Where is onchocerciasis most prevalent? How is it transmitted?
Onchocerciasis, a disease produced by the tissue nematode Onchocerca volvulus, affects millions of people in Africa and Central and South America. The infective larval forms are transmitted to humans through the bite of the black fly (Simulium) (Fig. 33-3). The common term for onchocerciasis, river blindness, takes its name from its feared complication and the fast-flowing rivers where the parasite and vectors are found.
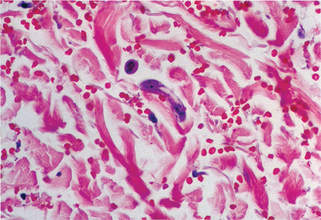
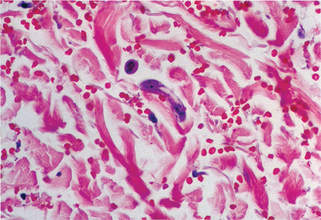
Figure 33-2. Larva currens. Biopsy demonstrates migrating larva of Strongyloides stercoralis in the dermis.
(Courtesy of the Fitzsimons Army Medical Center teaching files.)
Table 33-1. Parasitic Infestations of the Skin
| PARASITIC INFESTATION | VECTOR OR MODE OF TRANSMISSION |
|---|---|
| Filariasis | Mosquito |
| Onchocerciasis | Black fly |
| Creeping eruption | Soil contact and larval penetration |
| African trypanosomiasis | Tsetse fly |
| American trypanosomiasis | Kissing bug |
| Leishmaniasis | Sand fly |
| Schistosomiasis | Water contact and cercarial penetration |
| Dracunculiasis, sparganosis | Ingestion of larva |
| Echinococcosis, cysticercosis | Ingestion of cysts |
| Amebiasis | Direct contact or ingestion of cysts |
| Loiasis | Horse and deer flies |
| Demodex | Person-to-person contact in childhood |
8. Does river blindness cause cutaneous manifestations?
As the larval forms of Onchocerca develop into adult worms at the site of the bite, they produce subcutaneous nodules called onchocercomas, where numerous microfilariae are produced. They migrate into the skin, inducing a secondary dermatitis, skin pigmentation changes, skin thickening, frank elephantiasis, and an often disabling itching. The microfilariae also may migrate into the tissue of the eye and produce blindness due to severe uveal and corneal inflammation.
9. What are some of the problems with onchocerciasis treatment?
Diethylcarbamazine is effective treatment for the microfilarial stage, but a hypersensitivity reaction to large numbers of dying parasites in the anterior chamber of the eye may cause irreversible blindness and, in some cases, death. A safer course, in otherwise asymptomatic victims, is periodic “nodulectomy,” which removes the adult worms and significantly lowers the morbidity of onchocerciasis.
10. What is loiasis?
Loiasis, an infection endemic in the jungles of west and central Africa, is produced by the adult form of the tissue nematode, Loa loa, which is transmitted through the bite of various flies including deer flies (Chrysops




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









