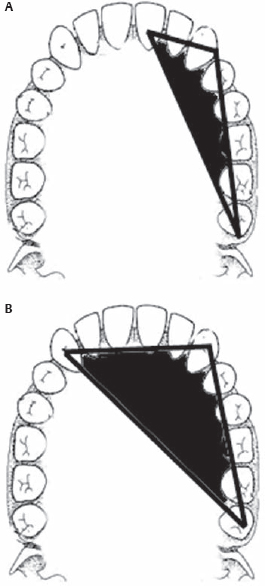
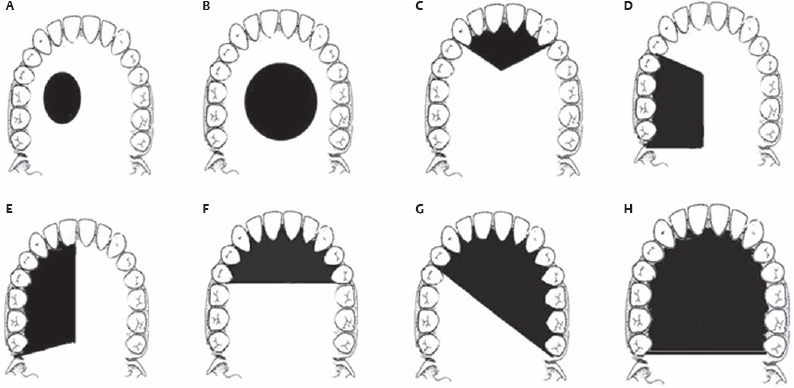
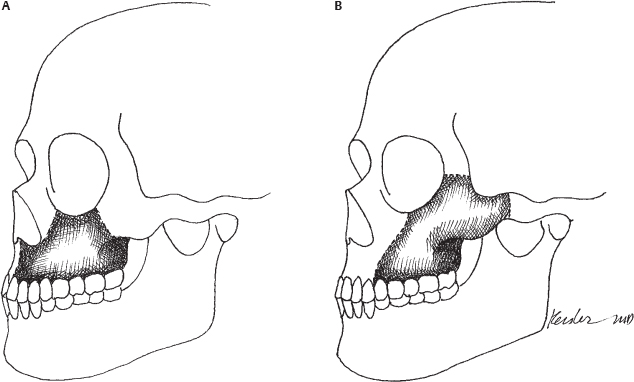
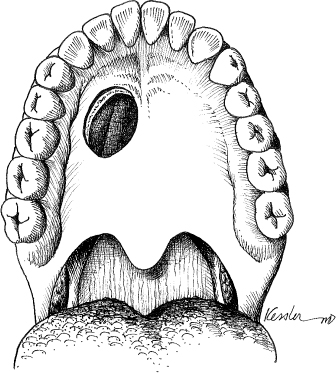
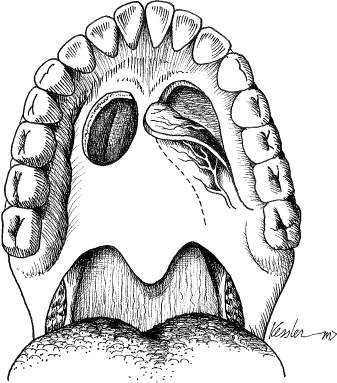
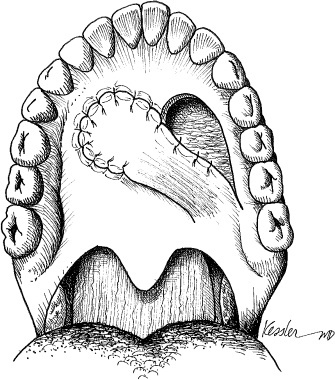
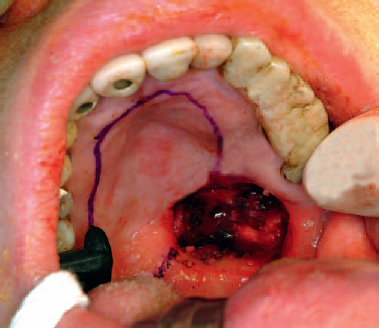
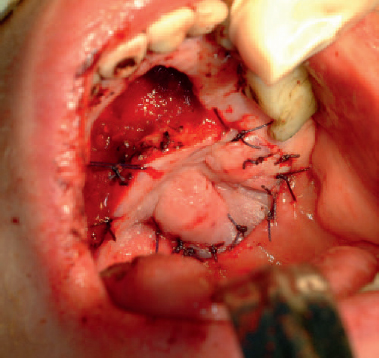
3 The unique three-dimensional infrastructure of the maxillary skeleton serves both functional and aesthetic roles. The palate provides support for the upper dentition, whereas the maxillary complex helps to support the globe and the nasal airway. As an aesthetic scaffold, the maxilla is also responsible for the projection and form of the nose, cheek, and upper lip. The relationship between form and function make postablative reconstruction of this area a formidable task for the reconstructive surgeon. Prosthetic obturation, local soft tissue flaps, free bone grafts, pedicle and free soft tissue flaps, and vascularized bone-containing free flaps, have all been used for palatomaxillary restoration. Choosing the best reconstructive modality to achieve an optimal result requires a comprehensive evaluation of the soft tissue defect, the bone defect, and the quality and quantity of the remaining dentition. Historically, tissue-borne prosthetic obturation was the only option for the orodental rehabilitation of postablative palatomaxillary defects. Although prosthetic obturation has several advantages, including immediate dental restoration without the necessity for further surgery, it is also associated with several shortcomings, most notably instability and poor retention. A breakdown in the oronasal prosthetic-tissue seal, characteristic of prosthetic instability, may lead to oronasal communication manifested by hypernasal speech and oral regurgitation. These shortcomings are accentuated in edentulous patients, irradiated patients, and those who have undergone extensive resections. Efforts to improve stability, and hence oral rehabilitation, have resulted in an improvement in prosthetic design. Surgically created scar bands and the midline palatal bony shelf are critical factors that help to retain palatomaxillary prosthesis. Lightweight prosthetic material and dental clasps were later introduced as a method of improving retention. In 1978, Aramany1 published a classification system of postsurgical maxillectomy defects and defined the biomechanics of the obturator framework for six categories of commonly occurring maxillary defects. He classified defects based on the remaining teeth and the surgical defect in an attempt to guide the design of prosthetic dentures. By anticipating the functional leverage forces associated with mastication, he advocated a design that would equally distribute and neutralize these forces to best stabilize the prosthesis. Aramany’s1 work and subsequent publications2 on this topic were instrumental in guiding the development and design of contemporary prosthetic obturator. However, achieving an optimal functional result, particularly in large palatomaxillary defects, is a significant challenge for prosthetics alone. Palatal reconstruction using pedicled palatal, pharyngeal, and nasal septal flaps has a long history with less than ideal outcomes.3 However, the limited availability of local tissue restricted the application of these flaps to the restoration of only small defects. As the biologic behavior of palatal and sinus carcinoma became better understood, the oncologic necessity for en bloc resection led to more extensive postablative defects, often involving the orbit and zygoma. Over the past several decades, a more critical appraisal of the functional results of prosthetic restoration has led reconstructive surgeons to apply a host of newly described pedicled flaps, such as the deltopectoral flap,4 temporalis flap,5 and the forehead flap,6 to palatomaxillary reconstruction. Primary surgical reconstruction of palatomaxillary defects has met with considerable opposition. Although palatal obturation permitted the close observation of the maxillectomy cavity, the most common site of recurrence, flap reconstruction prevents direct examination of the defect cavity. Until the last decade, primary reconstruction has been reserved for small, low-grade neoplasms of the palate. Furthermore, soft tissue reconstruction separates the oral and nasal cavities; however, obliteration of the maxillary cavity with bulky soft tissue may prevent the retention of a tissueborne dental prosthesis. Until the introduction of bony palatal reconstruction, the use of soft tissue alone effectively partitioned the oral and nasal cavities but precluded the retention of a denture, leaving patients unable to tolerate anything more than a pureed diet. The introduction of osseointegrated implants by Branemark et al7 in the late 1970s offered a new mechanism for the retention of prosthetic devices. Osseointegrated implants were first applied to the mandible serving as an anchor for implant-borne dental prostheses, thereby obviating the necessity for sufficient dentition for retention. The endosteal titanium fixtures are placed in the bone flap, where they are allowed to osseointegrate and not only anchor but also establish load sharing of the dental prosthesis, providing for more stable retention. The benefits of osseointegrated implants in masticatory function have been well described. Similarly, implant placement in the maxilla has been successful in achieving oral rehabilitation in palatomaxillary reconstruction.8 It is important to review briefly the three key elements to achieving successful retention and function of osseointegrated implants in the maxilla. Osseointegrated implants must be (1) anchored into sufficient bone stock, (2) vertically oriented, and (3) equally distributed across the load-bearing surface. After an extensive palatomaxillary resection, the bone stock that remains available for implant placement is often insufficient. Optimally, 7 to 10 mm of bone is required for osseointegration and long-term retention. A portion of the nasal bones, the zygoma, and, in some cases, the inferior orbital rim may remain intact after a maxillary resection. Although these bones may be sufficient for the placement of non–load-bearing prosthetic devices (i.e., nasal or ocular prostheses), they are insufficient for long-term implantborne dental retention. Vertically oriented and equally dispersed placement of the implants is essential to long-term success. Implant placement into the zygoma results in oblique torque forces counteractive to the vertical loading forces of mastication. These counteractive biomechanical forces lead to loosening and eventual implant loss. In an effort to achieve successful implant stability through osseointegration, several techniques have been employed to restore bone to the maxilla. Free iliac bone, vascularized rib with latissimus dorsi and periosteal flaps,9 and vascularized cranial bone flaps10 were used in the 1980s. Although these methods provided bone to the region, it was often insufficient for implant placement and the soft tissue was commonly too bulky to permit the retention of tissue-borne dentures. The application of microvascular reconstruction to the head and neck has greatly impacted the surgeon’s approach to both defect restoration and functional rehabilitation. Superior functional results in mandibular reconstruction using vascularized bone-containing free flaps led to the application of the osteocutaneous scapular free flap,11 followed by several publications describing fibular12,13 and iliac14 bone-containing free flaps for maxillary reconstruction. Vascularized bone-containing free flaps offer several benefits for primary maxillary reconstruction over traditional palatomaxillary obturation. This technique permits the single-stage transfer of vascularized soft tissue and bone; it facilitates restoring the separation of the oral and nasal cavities as well as providing bone adequate for the placement of osseointegrated implants. The mobility of the soft tissue paddles relative to the bone flap permits the restoration of complex three-dimensional defects of the palatomaxillary complex as well as relining the nasal and oral cavities. Probably the most significant advantage of free composite flap reconstruction is the ability to rehabilitate the extensive palatomaxillary defect. Table 3.1 The Goals of Palatomaxillary Reconstruction The biomechanical forces placed on a palatomaxillary obturator, particularly in extensive defects where the retentive surface is diminished, lead to a cascade of destabilizing forces. Reconstruction with autologous bone and soft tissue achieves the goals of palatomaxillary reconstruction (Table 3.1). It restores a permanent soft tissue seal, preserving oronasal competence, restoring nasal lining, and providing a fixed segment of bone ideal for dental rehabilitation. The maxillary bones are paired structures formed by the right and left maxillae. The body of each maxilla is hollow and shaped like a pyramid with the base situated medially, adjacent to the nasal cavity. In considering the anatomy relevant to palatomaxillary reconstruction, the maxilla should be divided into supportive buttresses and processes. The former constitute the infrastructure of the maxilla essential for mastication, and the latter are responsible for the form of the palate and midface. Ideally, reconstruction of the palatomaxillary defect should address both anatomic units. The anatomic complexity of the maxilla is related to its three-dimensional construct, which is a lattice-like structure supported by three separate paired buttresses. These buttresses, which have formed as an adaptation to the vertical forces of mastication,15 include the nasomaxillary buttress the zygomaticomaxillary buttress, and the pterygomaxillary buttress.16 The nasomaxillary buttress extends from the anterior aspect of the alveolus adjacent to the piriform aperture and nasal process of the maxilla, to the superior orbital rim and frontocranial attachment. This buttress supports vertical stresses placed on the anterior maxilla. The zygomaticomaxillary buttress is situated laterally, extending from the lateral aspect of the alveolus to the zygomatic process of the frontal bone superiorly and the zygomatic arch laterally. The pterygomaxillary buttress is situated posteriorly, extending from the maxillary tuberosity to the cranial base by the pyramidal process of the palatine bone and the medial pterygoid plate. The integrity of these buttresses is essential to providing a stable occlusal surface for the opposing dentition of the mandible. Furthermore, they allow for distribution of the masticator forces evenly across the skull base. Each buttress acts as a structural pillar providing both strength and maxillary position, which is roughly 45 degrees to the plane of the cranial base. Reconstruction of the palatomaxillary complex requires that at least two of the three buttresses be reestablished to evenly dissipate the vertical forces. Classically, there are four processes related to the maxilla: the zygomatic process, the alveolar process, the palatine process, and the frontal process. The zygomatic and alveolar processes play a key role in the form of the lateral midface. The zygomatic process is responsible for the aesthetics of the malar eminence. Reconstruction of this process requires an appreciation of the horizontal and vertical planes of the zygoma. The horizontal position of this process is parallel but slightly below the Frankfort horizontal plane.17 The horizontal arch runs from the lacrimal fossa to the zygomatic process of the temporal bone. The vertical plane extends from the zygomatic process of the frontal bone to the lateral antral wall. The combination of these two planes defines the contour of the lateral cheek. The alveolar process projects inferiorly from the infratemporal surface of the maxilla. Posteriorly, it projects beyond the third molar as the maxillary tuberosity. Both the vertical and horizontal positions of the alveolar process are important in providing the occlusal surface for the mandible. As mentioned earlier, the horizontal plane of the alveolar process is at a 45-degree angle to the skull base. The posterior projection of the maxillary tuberosity should be medial to the ascending mandibular ramus to prevent impingement on the coronoid process. The palatine process is a medial projection of bone deriving from the nasal surface of the maxilla. Its significance in maxillary reconstruction is minimal. Similarly, the frontal process of the maxilla is a thick band of bone that lies in front of the ethmoids and articulates with the frontal bone superiorly. The frontal process plays an integral role in lending strength to the nasal and lacrimal structures; however, it is of little significance with regard to midface reconstruction. Reconstruction of the maxilla requires reconstitution of the hard palate, lateral nasal wall, alveolus, the anterior face of the maxilla, and, in some cases, reconstruction of the body and the arch of the zygoma and orbital rim and floor. These structures are responsible for both the aesthetic characteristics of the midface as well as the functional properties such as a patent nasal airway and support of the globe. Reconstitution of the buttress system ensures a stable occlusal surface essential to functional mastication. To achieve stabilization and retention of a prosthetic obturator, every effort should be made to enhance the favorable biomechanical forces and de-emphasize the counterproductive torque forces placed on the obturator. Planning the design of the obturator should begin with a preoperative consultation with a prosthodontist. Similarly, thoughtful intraoperative decisions help to maximize the remaining hard and soft tissues that will later complement retention of the obturator. Surgical considerations for prosthetic rehabilitation should focus on the placement of a split-thickness skin graft within a palatomaxillary defect as well as the formation of tissue under cuts to aid in the creation of fibrous scar bands. Furthermore, the osteotomy cut adjacent to the defect should be made through an extraction site. Extraction of the adjacent tooth should be performed prior to the anterior osteotomy. This preserves the alveolar housing around a tooth, which is critical to retaining the prosthesis. The prosthetic prognosis, which refers to the functional success, is determined by (1) the size and location of the defect; (2) the quality, quantity, and location of the remaining dentition; and (3) the surface area of the remaining palate. A compromise in any of these factors impacts negatively upon the ability to effectively stabilize and retain a palatal obturator. The relationship between these factors results in a fulcrum line relative to the prosthetic framework. The position of the prosthetic fulcrum line is determined by the terminal abutment tooth closest to the maxillectomy defect. When three planes are drawn from the two terminal abutments to the opposite canine, a stable triangle is established (Fig. 3.1). The hypotenuse of the triangle represents the fulcrum line. When the defect enlarges, the area within the triangle diminishes as does the prosthetic stability. The rotation of the obturator framework along the fulcrum line occurs as a result of the differences in quality and quantity of supporting tissues on either side of the fulcrum line. The greater the rotational forces (referred to as cantilever forces), the greater the prosthetic instability. Aside from the intraoperative considerations mentioned above, there are several postoperative techniques that can be implemented in the design of the prosthesis that help to minimize the cantilever forces and thereby stabilize the prosthesis. Clasp assemblies fixed to the remaining dentition are essential to neutralizing the adverse cantilever forces. For this reason, the root form and condition of the periodontium is paramount. In particular, the condition of the tooth closest to the defect plays an essential role in determining prosthetic prognosis. This tooth is exceedingly important because it will bear the greatest stress. Hence, an adequate root form of this terminal abutment is an important factor. This is exemplified by the large discrepancy between the superior root form of the canine tooth compared with that of the lateral incisor. Defects that require resection of the canine tooth and a portion of the premaxilla result in a terminal abutment tooth with an inferior root form, the lateral incisor. Furthermore, this defect results in a shortening of the palatal arch. As the arch shortens, the ability to clasp teeth perpendicular to the fulcrum line, thereby preventing rotational forces, is diminished. The adverse forces placed upon a dental obturator include vertical dislodging force, occlusal vertical force, torque or rotational force, lateral force, and anterior-posterior force. Several publications have been devoted to techniques aimed at minimizing these forces.2,18,19 However, as the residual palate diminishes and the palatal defect enlarges, the cantilever forces become overwhelming, leading to prosthetic instability and a poor functional result. Large defects adversely affect prosthetic retention in two ways. First, they leave less dentition available to clasp. Second, they are associated with a diminished retentive surface area. The combination of these two factors results in greater cantilever forces over the defect. As a result, large defects of the palate result in a tendency for the prosthesis to tip toward the defect. The fulcrum is positioned across two stable teeth, the canine and the third molar. Each has a characteristically strong root form. Furthermore, the dentition beyond the fulcrum line may be securely clasped. Techniques to neutralize these counterproductive forces become ineffective in extensive palatal defects. Stabilizing large palatal defects requires the supplementation of bone to increase the area of the palatal arch. This can be achieved by the addition of either vascularized or nonvascularized bone into which osseointegrated implants may be placed and a stable fulcrum line may be reestablished. Since Ohngren’s20 original classification in 1933, there have been several classification schemes based on oncologic considerations that describe the anatomic boundaries of the maxillectomy defect.21–23 There are few classification systems, however, that address an algorithm for reconstruction. Past reports aimed at addressing the reconstructive options for rehabilitation of the palatomaxillary defect focused on prosthetic design, with little discussion regarding surgical reconstructive options. Spiro et al22 proposed a classification system in 1997 that was relatively straightforward; however, it focused on “low,” or infrastructure, defects, and failed to specifically address the involvement of adjacent structures such as the orbit and zygoma. The vertical dimension of the maxillectomy defect was more appropriately dealt with by McGregor and McGregor,23 yet this system incompletely addressed extensive palatal defects and the dilemma associated with prosthetic reconstruction of these defects. Realizing that the technique employed for optimal maxillary reconstruction was largely dependent on the nature and extent of the defect, Davison et al24 proposed a reconstructive algorithm based on a review of 108 cases using dental obturation, nonvascularized bone grafts, local flaps, regional flaps, and microvascular free tissue transfer. They divided patients into two broad categories of “complete” and “partial” maxillectomy defects. Although they proposed a wide range of reconstructive techniques, the failure to include a specific defect-oriented classification system outlining the remaining portion of the hard palate, dentition, orbit, and zygoma makes such a scheme difficult to apply as a reconstructive guide. In 2000, Brown et al25 reported a defect classification that is based on both the vertical and horizontal dimensions of a defect. The vertical component of the defect ranges from minor resections with no oroantral fistula, to radical maxillectomy defects with orbital exenteration. The horizontal component ranges from a small hard palate defect without involvement of dentition to a total palatectomy defect. According to Brown et al’s scheme, the classification of the horizontal dimension of the defect is based on the remaining palatal surface. Although the residual palatal surface plays an important role in determining the best form of reconstruction for the edentulous patient, the dentate patient can rely not only on the remaining palate but also on the remaining dentition for retention. Furthermore, the status of the orbital floor and zygoma, which play an important role in both the function and cosmetic results of reconstructive surgery of the midface, are not specifically addressed. Defects involving either of these areas are poorly managed by prosthetic rehabilitation, and, as a result, these patients often benefit from hard tissue reconstruction. Brown et al’s classification was the first to approach palatomaxillary defect classification with a multidisciplinary prospective, considering both surgical and prosthetic reconstruction to achieve a functional result. In an effort to define a systematic approach to palatomaxillary reconstruction, the Mount Sinai group introduced a classification system and treatment algorithm based on the biomechanical factors inherent to the remaining palate (Figs. 3.2 and 3.3).26 This approach divided palatomaxillary defects into three classes and two subclasses. The classification of each defect is dependent on the size and location of the defect in both the vertical and horizontal planes. In an effort to achieve the goals of optimal primary palatomaxillary reconstruction, each defect is classified to support a reconstructive algorithm. Defects that involve the hard palate but not the tooth-bearing alveolus were categorized as class Ia (Fig. 3.2A,B). Defects that involved any portion of the maxillary alveolus and dentition posterior to the canines or that involved the premaxilla were categorized as class Ib (Fig. 3.2C,D). Defects that involved any portion of the tooth bearing maxillary alveolus but included only one canine were categorized as class II (Fig. 3.2E,F). And defects that involved any portion of the tooth-bearing maxillary alveolus and included both canines, total palatectomy defects, and anterior transverse palatectomy that involved more than half of the palatal surface were categorized as class III (Fig. 3.2G,H). Defects that involved the inferior orbital rim were categorized as subclass “f” (Fig. 3.3A), whereas defects that involved the body of the zygoma were categorized as subclass “z” (Fig. 3.3B). The reconstructive algorithm was designed so that class I defects could be considered for soft tissue reconstruction or prosthetic obturator; class II defects could be considered for prosthetic reconstruction or vascularized bone-containing free flap reconstruction; and class III defects could be considered for vascularized bonecontaining free flap reconstruction. Isolated hard palate defects can range from a small oroantral fistula to a total hard palate defect. The approach to palatal reconstruction should be guided by the patient’s goals and the size of the defect. In general, the options include either prosthetic restoration or flap reconstruction. In many patients, prosthetic obturation offers a simple and immediate solution. In such cases, a preoperative mold can be fabricated so that a temporary prosthesis can be placed at the time of surgery. Obturators, however, have their drawbacks. Younger patients are often unhappy with the unnatural feel of an obturator. Many patients relate that obturators are socially awkward, and the need to wear a prosthesis during simple tasks such as drinking water or answering the phone is burdensome. Others find prosthetic hygiene onerous. This is particularly true for older patients, who complain of difficulty handling a prosthesis, and those with failing eyesight or debilitating arthritis. In spite of these drawbacks, prosthetic restoration provides patients with a nonsurgical single-stage option. Depending on the nature of the defect, surgical reconstruction of the hard palate can be achieved with a minimal investment in time, and the quality of life and functional outcomes are often excellent. In cases where primary reconstruction is being considered, it is essential that the surgical margins be negative. In those cases where the margins are in question, it is advisable to fabricate an obturator and consider a secondary reconstruction once the final margin analysis has been completed. Defects of the hard palate may result from a variety of etiologies including tumor extirpation, infection, and osteoradionecrosis. Isolated hard palate defects can be classified using a variety of classification systems; however, it is easiest to divide defects into those that are less than one-third the size of the palate and those that are greater than one-third the size of the hard palate. This is an effective distinction because it helps guide the options for reconstruction, as defects that are one-third the size of the hard palate or smaller lend themselves to adjacent tissue transfer techniques such as a palatal island flap or buccal flap. Larger defects often require free tissue transfer. The objectives of hard palate reconstruction are to establish a partition between the oral cavity and the nasal cavity and preserve the contour of the native hard palate. When considering the options for reconstruction, it is important to use a tissue graft that is hearty enough to maintain the partition between the oral and nasal cavities. Too often, mucosal grafts provide a satisfactory initial result, but over time they do not tolerate the mucosal stress. In contrast, tissue that is too bulky has an impact on a patient’s articulation and may preclude the retention of a denture if a denture is necessary. This is common in defects that are reconstructed with rectus or latissimus dorsi grafts. Ideally, the tissue graft should be thin and pliable but hearty enough to provide a reliable oronasal partition. Defects that are less than one-third the size of the hard palate can be easily managed with a prosthetic obturator or a local flap. An obturator usually requires a preoperative assessment. This facilitates the fabrication of a temporary obturator that can be placed at the time of the ablative surgery. As discussed, this type of restoration is simple and nonsurgical; however, in patients who require postoperative radiation, an obturator can be painful and difficult to fit. Because the tissue is inflamed and swollen during external beam radiation, it is often challenging to achieve a reliable prosthesis–tissue seal. The isolated hard palate defect that involves the non–tooth-bearing portion of the hard palate is considered a stable defect because the tipping forces associated with an obturator are minimal. Clasps applied to the remaining dentition provide support for the prosthesis, and prosthetic retention is conferred by the remaining palatal surface. In general, palatal prostheses designed for these defects are very stable. Patient dissatisfaction has led to the description of several locoregional and regional soft tissue flaps for the closure of the limited palatal defect. The mobility and accessibility of the oral tongue made this donor site a popular choice in the early 20th century. The obvious functional repercussions associated with the tongue flap have led to the use of several alternative donor sites including the temporalis flap, the buccal mucosal flap, and the palatal island flap. Most recently, free tissue transfer has been applied effectively to the rehabilitation of these defects. There are a variety of buccal mucosal and palatal flaps that have been described for the management of this defect; however, the palatal island flap represents an optimal option for isolated palatal defects (Fig. 3.4). This flap is pliable enough to comfortably rotate into the defect, thin enough to assume the contour of the native palate, and, because the palatal island flap is a mucoperiosteal flap, it provides a hearty partition that heals reliably to the adjacent palatal tissue (Fig. 3.5). In nonirradiated patients with small to moderate-sized isolated palatal defects, the palatal island mucoperiosteal flap is our primary reconstructive option. First described by Millard27,28 and later popularized by Gullane and Arena,29 donor tissue based on a single greater palatine neurovascular pedicle, can be rotated and safely transposed across the hard palate (Fig. 3.6). The mucoperiosteum associated with the flap serves as a barrier to effectively separate the oral and nasal cavities. The secondary defect, which results from harvesting a palatal island flap, remucosalizes over a 3- to 4-week period; however, patients can be started on an oral diet between 2 and 4 days postoperatively. Palatal defects that do not cross the midline can easily be repaired using this single-stage local flap. Similarly, posterior palatal defects requiring resection of the maxillary tubercle and dentition posterior to the ipsilateral canine are also amenable to reconstruction using the palatal island flap. The mucosa remains sensate, which aids in mastication and oral transport, and, more importantly, coverage of this defect using the palatal island flap does not preclude the successful retention of a tissue-borne denture. ♦ The blood supply of the palatal island flap is the greater palatine artery and vein. The neurovascular pedicle emerges from the palatine foramen before entering into the soft tissue of the palatal mucosa. ♦ The posterior aspect of the palatine foramen is composed of a thin column of bone that can be fractured with a straight osteotome to release the neurovascular pedicle from the foramen and provide greater rotation of the flap if necessary. ♦ When designing the flap, it is important to carefully template the defect (Fig. 3.7). The flap dimensions should be designed to closely match the defect to prevent redundancy. As the flap rotates into position, it will shorten the flap length by between 10 and 30%, so it is important to account for this in the design of the flap. ♦ The flap is raised in the subperiosteal plane to prevent injury of the neurovascular bundle. The flap should be raised from anterior to posterior until the palatine foramen is identified. This provides the optimal length and rotation of the flap. ♦ When rotating the flap into position, special attention should be addressed to preventing a kinking of the palatine vascular pedicle (Fig. 3.8). ♦ Once rotated into the defect, the flap can be sutured into position with 2.0 Vicryl sutures. In some cases, small drill holes can be placed through the hard palate along the leading edge to secure the medial aspect of the flap. ♦ The healing over 3 to 6 weeks provides the opportunity for the donor site to remucosalize (Fig. 3.9).
Palatomaxillary Complex Reconstruction
• Support the orbital contents
• Separation of the mouth and nose
• Reconstruct the palatal surface
• Reconstruct the lacrimal apparatus
• Provide facial symmetry
• Dental rehabilitation
♦ RELEVANT ANATOMY
♦ BIOMECHANICAL CONSIDERATIONS
♦ CLASSIFICATION OF PALATOMAXILLARY DEFECTS
♦ HARD PALATE DEFECTS
♦ THE PARTIAL HARD PALATE DEFECT
Option for Management: Restoration Using a Prosthetic Obturator
Option for Management: Palatal Island Flap
Surgical Technique and Considerations
Patient Selection and Perioperative Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree