Fig. 9.1
Typical clinical appearance of Paget’s disease with chronic eczema and nipple erosion within the nipple-areola complex
9.4 Diagnosis
Once any of the typical clinical signs and symptoms described above raises the suspicion of PD, a diagnostic work-up must suddenly be started. Physical exam, mammographic x-ray (MXR) and breast ultrasound (US) are the first line diagnostic step in order to find any possible breast lesion or mass, which together with the clinical suspicion of PD, can corroborate such a diagnosis. Physical examination can reveal a mass, which might then be seen as a nodule by MXR or US. Even if neither masses nor nodules are palpable or visible, microcalcifications could be a possible finding seen at MXR. Any dubious breast lesion will be biopsied independently of PD suspicion. Simultaneously a cytology test by nipple-areola scraping should be performed to confirm PD diagnosis. If all these tests end up to be negative a dermatology consultation and a short-time follow-up, at 2 weeks, might be a sensible option. However, even if all the tests are negative, but the epidermal lesions are very worrying, a full thickness skin biopsy must be performed. Otherwise, if any of the aforementioned tests turns out to be positive, it is of utmost importance to rule out which one of the following three conditions can occur:
A breast carcinoma without PD
A PD without any momentarily visible breast lesion
A PD with an associated breast lesion, biopsy confirmed to be a carcinoma.
In the case of a confirmed breast carcinoma, within the mammary gland, but negative cytology test for the nipple-areola eczematous lesion, if the PD suspicion remains high, a full thickness skin biopsy must be performed to rule out PD in a reliable way. In the case of a negative skin biopsy, we are facing a BC without PD, which will be investigated and treated consequently, while a positive skin biopsy, as well as a positive scraping cytology, put us in front of a mammary PD. Eventually, after the diagnostic work-up, two situations of mammary PD can occur: 1) PD with an associated BC; or 2) a PD without any identified underlying BC (Fig. 9.2).
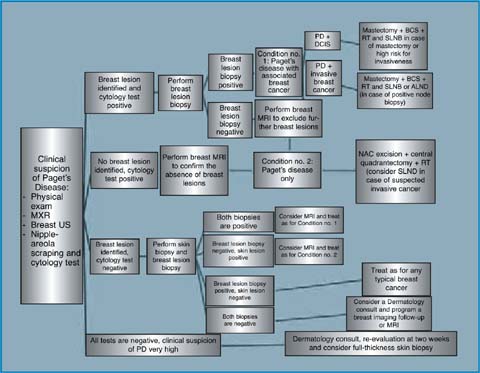
Fig. 9.2
Diagnostic and therapeutic flow-chart of mammary Paget’s disease
In both cases a breast magnetic resonance imaging (MRI) is a recommended second line investigation, especially when an underlying DCIS or invasive cancer has not been identified by first line investigations. MRI can also help in detecting multifocal/multicentric lesions and in better defining lesion topography with respect to the nipple-areola complex (NAC) [18, 19]. However, such advice is only a category 2A recommendation, because there are no randomized clinical trials to demonstrate that MRI gives any advantage in terms of survival or recurrence rate in PD.
9.5 Treatment
Mastectomy with or without axillary lymph node dissection has been the standard surgical treatment for many years [20]. Things have changed over the years but it is still not possible today to make a category 1 recommendation for PD surgical therapy. Some studies have shown that breast-conservative surgery (BCS) followed by radiation therapy (RT) is an adequate option to treat PD, achieving the same survival and local recurrence rate as after mastectomy [21–25]. This is in accordance with what has already been demonstrated for any typical in situ or invasive BC [26, 27]. A BCS treatment should always mean an NAC excision along with the underlying breast cancer, when identified. When feasible in a conservative manner, the associated cancer could be excised even as a different specimen not in continuity with NAC, also using different incisions. Otherwise, when an underlying BC has not been shown by the imaging work-up, an NAC excision alone, with a portion of breast gland tissue beneath, can be done, as long as the pathologist confirms a negative margin status. All BCS treatments must be followed by whole breast RT. Mastectomy remains the preferred option in case of very small breast volume, multicentricity, and in such conditions in which RT will not be possible. A skin-sparing mastectomy might be a valid option, either with immediate or delayed reconstruction. RT alone for PD without an underlying breast nodule or mass has been proposed as well [28–30]. However, small numbers of cases and conflicting results, make it an option to be reserved for very selected cases.
Axillary staging is not necessary for PD “per se”, being PD an in situ lesion in its nature. Nonetheless, PD is almost always acc ompanied by an underlying BC, which is why axillary staging should be considered on a case by case basis. In the case of an underlying invasive BC a sentinel lymph node biopsy (SLNB) or an axillary lymph node dissection (ALND) must be performed depending on the clinical staging of the axilla and confirmed metastasis by percutaneous US guided biopsy. Instead, when an underlying DCIS is identified by preoperative work-up, SLNB is not mandatory, unless a mastectomy is planned, since it will preclude any axillary staging in the future, or unless the DCIS lesion has very suspicious features, which may turn out to be invasive at definitive pathology response. There are two retrospective studies in the literature regarding SLNB in PD [31, 32], both demonstrating the accuracy of SLNB procedure. The more recent one [32] favors SLNB in any case of PD, since the risk of having an underlying invasive BC is as high as 27% even without any imaging finding at the preoperative work-up, and thus would avoid a second intervention (Fig. 9.2). In the case of breast-conservative surgery, as already explained, RT has to be performed after any BCS for PD, considering a radiotherapic boost on the surgical site and on the NAC area.
Adjuvant systemic therapies will be chosen based on the underlying BC parameters. For the rare cases of PD alone, as for DCIS, patients are at higher risk of developing any BC event in the future, which is why a Tamoxifen systemic therapy could be a viable option to be discussed with the patient.
References
1.
Paget J (1874) On the disease of the mammary areola preceding cancer of the mammary gland. St Bartholomews Hosp Rep 10:87–89
2.
Tavassoli FA (1999) Pathology of the breast. Appleton and Lange, Norwalk, Connecticut, pp731–760
3.
Sakorafas GH, Blanchard K, Sarr MG et al (2001) Paget’s disease of the breast. Cancer Treat Rev 27:9–18PubMed




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





