Aesthetic and functional surgery of the nose presents a variety of complex challenges. These challenges are even more profound in revision rhinoplasty when the surgeon is attempting to correct deformities in which loss of tissue, scar contracture, and lack of autogenous grafting material make optimal results more difficult. Over the years, we have used multiple techniques to address specific situations that arise during both primary and revision rhino-plasty. It is important to learn from others and remain up to date with techniques described in the literature. Understanding these techniques, modifying them to meet your needs, and perhaps, most importantly, knowing when to use them, must be a continual process to improve outcomes. We have chosen to discuss cases performed within the last 6 months (except Case 5) to provide an overview of our current rhinoplasty practice and the latest techniques we use to address difficult problems in revision rhinoplasty.
The first step in evaluating a patient considering rhinoplasty is nasal analysis. Nasal analysis in revision cases should include palpation of the nose to assess the tissues remaining such as septal cartilage, bony pyramid, thickness of the overlying subcutaneous tissue, bossae formation and other tip asymmetries, and middle vault contour. Also important is intranasal examination for synechiae, turbinate hypertrophy, persistent septal deviation or perforation, and evidence of valve collapse. Because these patients have not had satisfactory initial results, they can be more demanding. Realistic expectations and goals should be discussed with the patient beforehand. Depending on the anatomic problem, an appropriate incidence of further revisions is provided to the patient. For all but minor revisions, we estimate a 1:15 rate for further revisions. Photographic documentation is critical.
In some cases, overresection of tissue or scar contracture severely limits the ability to address cosmetic concerns and thus functional improvement should be considered the primary goal; however, both can often be achieved with careful planning and execution. Camouflage grafts can help improve cosmetic appearance when rearrangement of the primary structures is not possible. Generally, for small contour deformities, cartilage grafts are placed in precise pockets endonasally. More major revision of the tip and middle vault are usually performed through an external approach. Timing of surgery is important as well; major revisions should be approached when an adequate amount of time has allowed for scar maturation, whereas minor revisions may be approached with some flexibility.
We describe techniques we routinely use in revision rhinoplasty cases to address specific problems in the middle vault and tip. These are discussed in a case format for graphical clarity. All but Case 5 were performed in the last 6 months to give a true “snapshot” of our current preferences. This, of course, limits our ability to provide long-term follow-up and photographs for this group of patients. Selected cases involved middle vault and tip deformities, but many revisions involve the bony pyramid. Minor irregularities of the dorsum are treated with a rasp or camouflage with autogenous cartilage—frequently lightly morselized cartilage. Osteotomies are usually performed with a perforating technique: external to move the nasal bones medially and internal to move them laterally.
 Revision Rhinoplasty Techniques for Complication Correction
Revision Rhinoplasty Techniques for Complication Correction
Unilateral Spreader Graft
Spreader grafts were initially described by Sheen.1 These grafts were used for correction of internal valve collapse. Internal valve collapse can result from resection of the cartilaginous nasal dorsum without correction of the prolapsed upper lateral cartilage. This is a frequent problem encountered in revision rhinoplasty. In addition to nasal obstruction, subluxation of the upper cartilage can result in an inverted-V deformity, resulting in a pinched middle vault and giving the nose an unnatural appearance. This deformity also may be associated with mucosal scarring if mucosal injury occurred during dorsal hump reduction. Correction of this problem with a unilateral (or bilateral as needed) spreader graft when there is an asymmetric middle third of the nose provides not only an enhanced aesthetic appearance but also improved function. This has the advantage over camouflage onlay cartilage grafts in that a spreader graft will provide an optimal functional and cosmetic result and is less susceptible to absorption and movement. We use the unilateral spreader graft primarily for cases of internal valve collapse with asymmetry of the middle third, resulting from a prolapsed upper lateral cartilage.
Case Example 1
The patient presented with nasal deviation and nasal obstruction after trauma and unsuccessful reduction. Clinical examination revealed a significant external nasal deformity and prominent dorsum in the upper third of the nose. The middle third also demonstrated a prominent dorsum and deviation to the left. The lower third demonstrated mild tip asymmetry and poor tip support (Fig. 21–1).
The patient underwent an endonasal approach with septoplasty, lowering of the bony and cartilaginous dorsum with lateral osteotomies to address the upper two thirds of the nose. The asymmetry of the middle third was addressed with a unilateral spreader graft on the right. A cartilaginous strut was placed endonasally to address tip ptosis and help correct minor tip asymmetry (Figs. 21–2, 21–3).
Three-dimensional imaging allows complete visualization at any angle of a digitally captured image. This technique also allows measurement of surface distance, area, and volume measurements within 1-mm accuracy. Three-dimensional imaging provides another interesting tool to critically analyze rhinoplasty results and enhance surgical education2 (Fig. 21–4).
Case Example 2
A 43-year-old female presented after a previous rhinoplasty with breathing problems as well as dissatisfaction with the appearance of her nose. On clinical exam in the upper third she had irregularities of the nasal dorsum. The middle third demonstrated external asymmetry and collapse of both internal nasal valves. The lower third demonstrated bulbosity of the nasal tip and subtle irregularities of the lateral crura. She also exhibited microgenia (Fig. 21–5). An open septorhinoplasty with smoothing of the dorsum and osteotomies was used to address the upper third. The internal nasal valve was repaired by reapproximation of the left upper lateral cartilage to the septum and placement of a spreader graft on the right. For the lower third, a cephalic excision was used to reduce the lower lateral cartilages, irregularities of the lateral crura were shaved, and the domes reconstituted. An alar batten graft was placed on the right and a strut in the columella. She also had a medium Gore-Tex (Flagstaff, AZ) chin implant placed (see Figs. 21–6, 21–7).
This case illustrates the usefulness of unilateral spreader grafts to address internal valve collapse as well as asymmetry of the middle third. This graft provides both a functional and aesthetic improvement. Reconstitution of the upper cartilages to the septum can be adequate to address internal valve collapse, but more often spreader grafts are required. Spreader graft shape and thickness are individually fashioned according to the degree of asymmetry. Care must be taken with these grafts not to inadvertently widen the middle third of the nose or injure the underlying mucoperichondrium.
Tongue-in-Groove Technique
The tongue-in-groove technique described by Kridel et al.3 addresses specific problems such as excessive columellar show. It can be used to control nasal tip rotation and projection without excising tissue.3 This technique consists of manipulating the position of the medial crura of the lower lateral cartilages in relation to the caudal septum to reduce columellar show and provide additional tip support and rotation, depending on where on the caudal septum the medial crura are attached. It may require some excision of membranous septum, depending on how far back the crura are set on the septum. However, it is an excellent method to address caudal septal excess, tip projection, and rotation. A final attribute to this technique is the opportunity to reduce columellar width by excising soft tissue between the medial crura.

Figure 21–1 (A–D) Preoperative deviated nose.
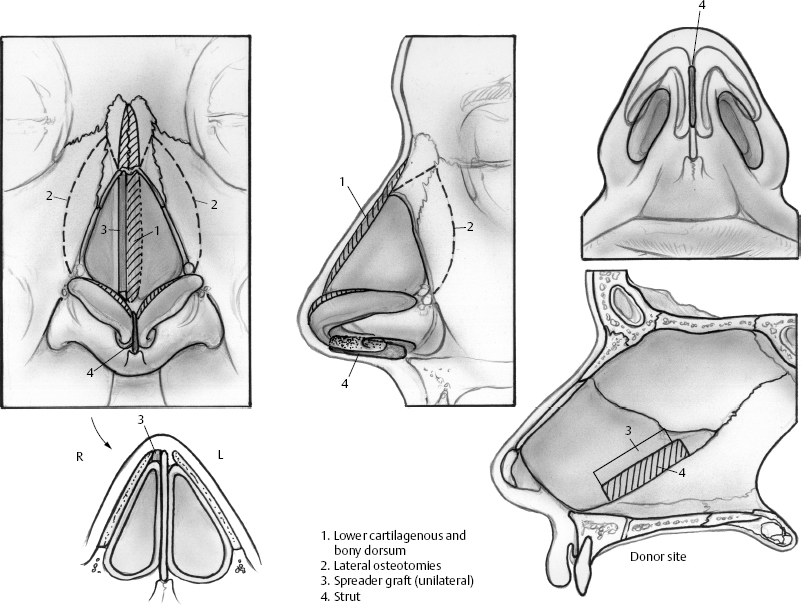
Figure 21–2 Reconstruction with unilateral spreader graft.
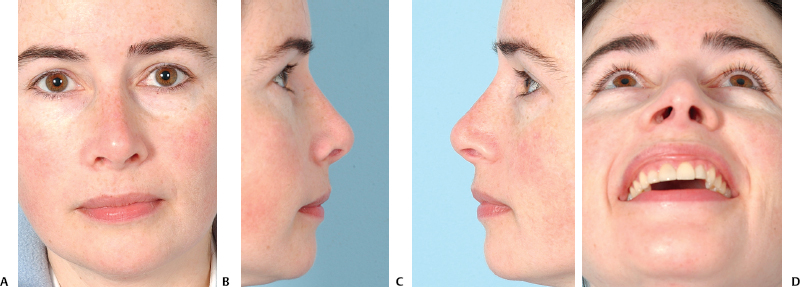
Figure 21–3 (A–D) Postoperative photographs.
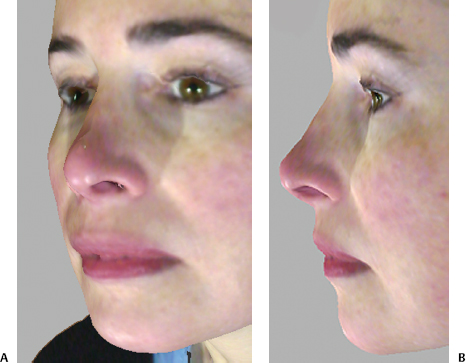
Figure 21–4 Three-dimensional photographs (A)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


