CHAPTER 26 Osteotomy of the Tibia and Fibula
INDICATIONS
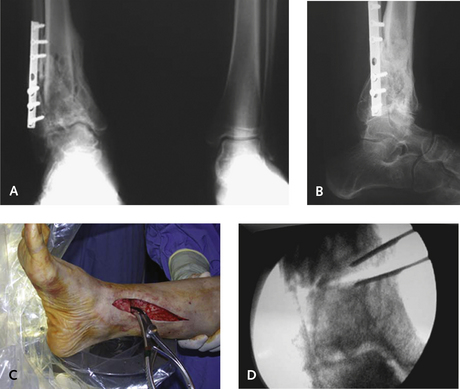
Indications for the supramalleolar osteotomy are numerous and include correction of deformity, joint preservation, and as a staged procedure that leads up to other operations, including total ankle replacement. Osteotomy is performed for correction of a malunion of a distal tibia fracture, with or without ankle joint arthritis, to redistribute or beneficially alter the contact pressures on the degenerated cartilage with mechanical realignment. Osteotomy can be used for preservation of limb alignment as a prelude to a total ankle replacement. One of the prerequisites for a successful total ankle replacement is a balanced mechanical axis of the foot with respect to the lower leg, and a supramalleolar osteotomy works well as a staged procedure for the appropriate patient (Figure 26-1).
PREOPERATIVE PLANNING
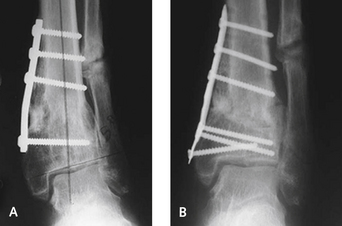
Measuring the center of rotation of angulation (CORA) of the deformity is important. The CORA is located at the intersection of two lines representing the mechanical axes of the proximal and distal segments of the deformity. A closing or opening wedge osteotomy at the level of the CORA leads to complete realignment of the foot and ankle. If the osteotomy is made proximal or distal to the CORA, the center of the ankle translates relative to the mechanical axis of the tibia and creates an unnecessary shift of loads and a clinically obvious zigzag deformity (Figure 26-2).
The osteotomy line should be translated and angulated so that a secondary translational deformity is not created when the osteotomy is intentionally made at a different level from that of the CORA (Figure 26-3), as with correction of an equinus malunion of an ankle arthrodesis. In this deformity, the position of the forefoot is fixed relative to the axis of the tibia. The simplest method of correction is to remove an anteriorly based wedge from the distal tibia and then close the osteotomy while maintaining the posterior cortex intact in a greenstick-type maneuver. The problem with this type of correction is that the foot is translated anteriorly relative to the tibia, and then the mechanical limb axis is no longer aligned or efficient for ambulation.
SURGICAL TECHNIQUE
Correction of Varus Deformity
For the correction of a varus deformity, I use either a medial opening wedge osteotomy or a lateral closing wedge osteotomy. For the medial opening wedge osteotomy, I use an anteromedial and a small lateral incision (for the fibular osteotomy). Which cut is made first is a matter of preference, but leaving the fibula intact provides some stability while the tibial cut is completed. When the deformity is minimal, then a greenstick cut of the tibia is made, in the hope that a fibular osteotomy may not need to be performed. This greenstick cut markedly increases the stability of the osteotomy, and the tibia can be opened with a laminar spreader to the desired amount. The advantage of this sequence is that the tibia does not move around after the cut is made, and movement may compromise stability. Another alternative is to apply a three-hole plate to the lateral aspect of the distal tibia at the level where the osteotomy exits. With this technique, the osteotomy cut does not open, and the correct tension on the osteotomy can be applied until the ankle is plantigrade. The plate is applied just before the osteotomy cut exits the lateral tibial cortex.
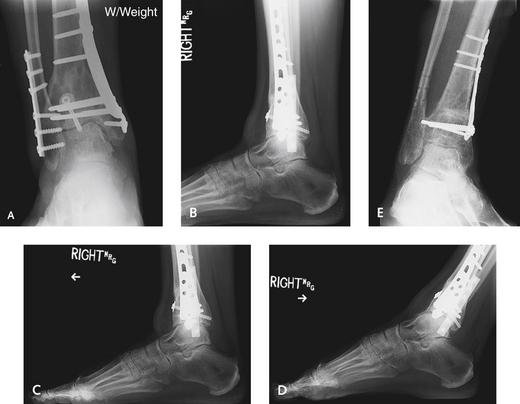
The opening wedge osteotomy is performed 4 cm proximal to the medial malleolar tip in metaphyseal bone (Figures 26-4 and 26-5). Once the skin incision is made, minimal periosteal stripping that is sufficient only to complete the osteotomy is performed. The cut is planned in the metaphysis. I apply the selected plate on the surface of the tibia before the osteotomy is made, ensuring that sufficient space is maintained to obtain fixation with three screws distally, mark the osteotomy, and complete it. I keep periosteal stripping to a minimum when the bone cut is made perpendicular to the tibia with a broad oscillating saw, and I preserve the opposite cortex and periosteal sleeve to act as a fulcrum for the opening wedge and to enhance stability. If nothing more than uniplanar angulation is required, then a small plate over the lateral tibia is useful to prevent overcorrection. If translation and rotation also are necessary, then the opposite cortex must be cut to allow the distal segment to move. The fibular osteotomy is performed with the lateral incision at the same level as that for the tibial osteotomy, although this location is not critical. A wedge osteotomy of the fibula can be performed if marked angular deformity is present and when a closing lateral wedge osteotomy of the tibia is performed. I prefer to use a structural allograft from a femoral head to fill the defect. Once the osteotomy has been performed, a laminar spreader is inserted to gradually distract the osteotomy to the desired level. This is checked fluoroscopically. The structural bone graft provides immediate mechanical support, with little likelihood of collapse even after resorption, which occurs during revascularization. Some structural integrity remains during the process of bone graft incorporation, to allow the graft to withstand loads. After the deformity has been corrected, the osteotomy is provisionally secured with Kirschner wires (K-wires), and the plate is applied to the tibia at this time. The alignment is assessed with fluoroscopy.