Fig. 21.1
An intra-operative photograph of a right knee in a patient undergoing revision ACL reconstruction in association with a tibial deflexion osteotomy. Guidepins have been placed medial and lateral to the patellar tendon (PT) just proximal to the tibial tubercle (TT). The patella (Pat) is also labeled

Fig. 21.2
An intra-operative lateral fluoroscopic image of a right knee in a patient undergoing revision ACL reconstruction in association with a tibial deflexion osteotomy. Guidepins have been placed demarcating the superior and inferior cuts of the planned osteotomy. The pins converge of the posterior cortex. The tibial tunnel (arrows) for the ACL graft is visible
With retractors in place protecting the superficial MCL and patellar tendon, the lower cut of the osteotomy is made under the lower pins with an oscillating saw. Care must be taken to complete the cuts on the medial and lateral cortices while keeping the posterior cortex intact. The upper cut is then completed in the same manner and the anterior bone wedge is removed. The posterior cortex is then perforated numerous times with a 3.5 mm drill, weakening it prior to closing the osteotomy (Fig. 21.3). When the posterior hinge is sufficiently weakened, the osteotomy site will be seen to close slightly. One can then gently extend the knee, closing the osteotomy. Fixation is achieved with two large staples, one on either side of the patellar tendon (Fig. 21.4). Care must be taken to avoid placing the medial staple through the tibial tunnel. There is a tendency at this point to create a varus angulation of the tibia, which must be avoided by ensuring symmetrical closure of the osteotomy site. The impact of the osteotomy on patellar height is minimal and no adverse effects have been noted. After the osteotomy is fixed, the reamer is again passed through the tibial tunnel to smooth out any malalignment that resulted from the osteotomy. The graft is then passed and secured according to the surgeon’s preferred technique (Fig. 21.4).
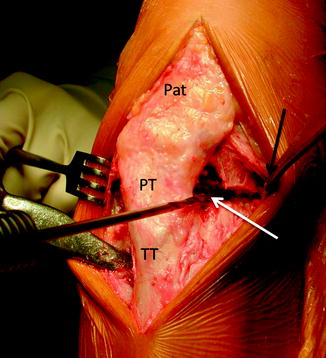
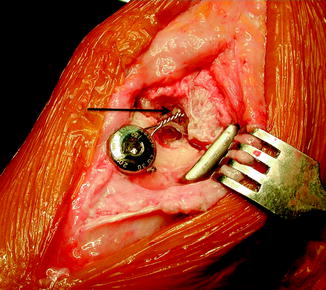
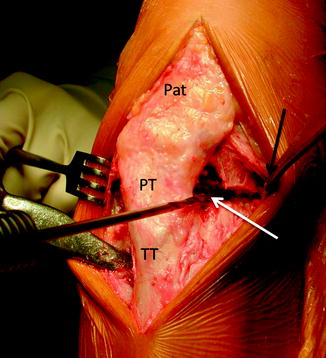
Fig. 21.3
An intra-operative photograph of a right knee in a patient undergoing revision ACL reconstruction in association with a tibial deflexion osteotomy. The osteotomy has been completed and the bone wedge removed. A 3.5 mm drill (white arrow) is being used to perforate and weaken the posterior cortex prior to osteotomy closure. The patellar (Pat), patellar tendon (PT), and tibial tubercle (TT) are labeled. The superficial medial collateral ligament is being retracted medially (black arrow) to protect is and improve visualization as during the cut
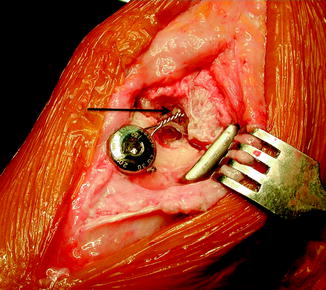
Fig. 21.4
An intra-operative photograph of a right knee in a patient following revision ACL reconstruction in association with a tibial deflexion osteotomy. The osteotomy has been fixed with two metal staples, the medial of which is visible. The ACL graft has been fixed in the tibia with an interference screw backed up with a wire tied around a post (arrow)
The change in tibial slope frequently leads to excessive recurvatum in the reconstructed knee relative to the preoperative state and the contralateral side. Because this recurvatum can lead to stretching of the graft and early failure, we prefer to perform a posteromedial capsular advancement to normalize extension. This procedure is performed through the same incision by dissection posteromedially around the knee and releasing the posteromedial capsule from its origin on the posteromedial femur just proximal to the flexion surface of the medial femoral condyle. Two suture anchors are then placed where the capsule was released and the sutures are passed through the capsule 5–10 mm distally. Tying the sutures retensions the capsule and eliminates the recurvatum.
Postoperative rehabilitation is quite different from that following a standard ACL reconstruction. The knee is placed in a brace and passive motion from 10 to 90° of flexion is initiated immediately. A continuous passive motion (CPM) machine may be useful. Full extension is avoided for 6 weeks postoperatively to protect the posteromedial capsular advancement and avoid recurvatum. Weight-bearing is allowed 8 weeks following surgery. Anti-coagulation is recommended until weight-bearing is allowed.
Potential complications include surgical site infection, deep venous thrombosis (DVT), neurovascular injury, nonunion of the osteotomy site, over- or under-correction of tibial slope, and the creation of an iatrogenic varus deformity of the tibia. Careful preoperative planning and attention to detail intra-operatively can minimize these risks.
Outcomes
There is little data available on the outcome of tibial deflexion osteotomy performed in association with ACL reconstruction. D Dejour et al. reported a series of 22 knees with chronic anterior laxity and excess tibial slope (average 16.5°) [25]. They performed deflexion osteotomy in all 22 patients and associated ACL reconstruction in 18 of the patients. They noted improved results in the patients in whom both procedures were performed and recommended the combined procedure. A good outcome has also been reported in a case of bilateral congenital absence of the ACL treated with ACL reconstruction and tibial deflexion osteotomy [26].
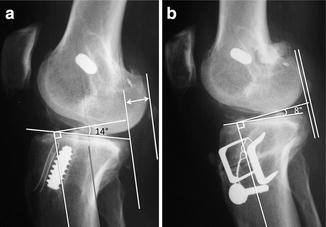
Unfortunately, there are no published studies comparing the results of revision ACL reconstruction with or without associated tibial deflexion osteotomy in patients with chronic anterior instability and increased posterior tibial slope. Our experience has been that slope correction and good control of tibial slope can be reproducibly obtained with this technique (Fig. 21.5).
Get Clinical Tree app for offline access
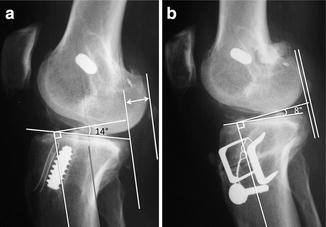
Fig. 21.5
Preoperative (a) and postoperative (b




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








