Fig. 22.1
Algorithm for the treatment of failed ACLR and malalignment (see text)
Occasionally, a two-stage procedure is indicated also in young active patients with tibial/femoral tunnel widening (>16–17 mm) and malalignment after failed ACLR. In this case, HTO and bone grafting of the tunnels with or without PLC reconstruction is performed first, and then ACL revision is performed after 6 months. When necessary, PLC reconstruction is performed according to the surgeon’s preferred technique.
ACL failure due to knee hyperextension certainly represents a challenge for the orthopedic surgeon. Decreasing the tibial slope can help provide stability to the knee, but may also result in increased hyperextension, mostly with closing wedge HTO. In these cases, our current approach is to decrease the slope with opening wedge HTO and, if instability persists, perform an ACL revision.
According to the single case, nonanatomic ligamentous reconstruction techniques may be considered. Between these techniques, the following should be mentioned: (1) Marcacci’s technique with proximal over the top positioning of the graft and lateral extra-articular tenodesis [9]; and (2) isolated lateral extra-articular tenodesis with fascia lata [10]. Even if not anatomic, Marcacci’s technique has numerous advantages, and these include: (1) proximal over the top position, without concerns regarding the previous femoral tunnel; (2) increased rotary stability of the knee; (3) easy proximal and distal fixation; and (4) lateral tenodesis, which provides varus stability in case of lengthened PLC structures. This technique can be performed with hamstring autograft as well as with tibialis anterior or Achilles tendon allografts. The graft should be at least 28 cm long.
Rarely, varus distal femoral osteotomy (DFO) can be indicated after failed ACLR. The indications include:
1.
Lateral compartment osteoarthritis.
2.
Symptomatic osteochondral defects of the lateral compartment (DFO + ACL revision + Cartilage repair).
3.
Chronic medial collateral ligament tear and severe valgus malalignment (DFO + ACL revision + medial collateral ligament reconstruction/retensioning).
In these cases, a medial closing DFO is performed with or without combined procedures. This technique allows for a quick healing and a single surgical approach on the medial side of the knee if ACL revision, cartilage repair, or medial collateral ligament reconstruction/retensioning is associated. Lateral opening wedge DFO can also be considered.
Treatment
Preoperative Planning
The HTO is described by Dugdale et al. [11] with a slight valgus overcorrection (3–5°) in knees with medial arthritis. In this scenario, the mechanical axis should pass through a point located at 62.5 % of the width of the tibial plateau, right lateral to the tip of the lateral tibial spine. In young, active patients a correction to neutral alignment (50 % of the tibial plateau) is planned [12]. Opening wedge HTO is planned drawing a line from this point (62.5 or 50 %) to the femoral head center, and another line from this point and ankle joint center (Fig. 22.2a). The angle obtained represents the angle of correction (α) [alpha]. The osteotomy line (ab) is defined from medial (≅4 cm below the joint line) to lateral (tip of the articular fibular head). This measurement is transferred to both rays of the α angle from the vertex (aibi and aic). In this manner, two identical segments, which are equal to the osteotomy length, define the α [alpha] angle. Next, the segments are connected by another line (bic) which is used as the base of an isosceles triangle and corresponds to the opening wedge that should be obtained medially at the osteotomy site (Fig. 22.2a).
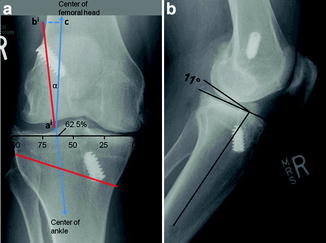
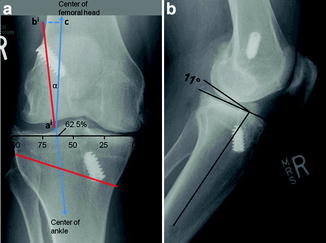
Fig. 22.2
Patient with failed ACLR, varus malalignment, and knee arthritis. (a) Planning for opening wedge HTO in the coronal plane (AP view), with a slight valgus overcorrection, considering the medial arthritis (see text). (b) Evaluation of the posterior tibial slope on the lateral view
The tibial slope is assessed on lateral view radiographs (Fig. 22.2b). The slope normally varies from 0 to 18° [13]. The amount of tibial slope correction depends on the starting value. Minimal correction is required when the slope is less than 8°, while a larger correction is needed when the slope exceeds 10°.
The planning for closing wedge is similar to opening wedge HTO. However, the osteotomy is different and entails two cuts, but the α [alpha] angle is calculated as previously described. The proximal cut is usually horizontal and is placed 2–2.5 cm below the joint line. The proximal and distal osteotomy should define the angle of correction (α) [alpha]. The tibial slope is usually decreased after a closing wedge HTO. However, it is more difficult to accurately modify or correct the tibial slope using this procedure.
Surgical Technique
According to surgeons’ preference, either opening wedge or closing wedge HTO can be performed. The ACL graft and the reconstruction surgical technique is also a matter of the surgeon’s preference.
Opening Wedge HTO
The surgery is performed with the patient on a radiolucent operating table [14, 15]. A lateral post is positioned at the level of the thigh, to allow the foot to be dropped out of the table and to achieve at least 120° of knee flexion. Intravenous antibiotic prophylaxis is administered. A tourniquet is placed around the proximal thigh. A skin marker is used to identify the medial joint line, the tibial tubercle and patellar tendon, and the posteromedial border of the tibia. The leg is elevated and the pneumatic tourniquet inflated. A 5–8 cm incision is created from 1 cm below the medial joint line midway between the medial border of the tibial tubercle and posteromedial aspect of the tibia [5, 14, 15]. The incision can be performed more lateral and extended proximally in case of concurrent ACL revision with patellar tendon autograft. If hamstring autograft is preferred, harvesting of the graft is performed at this point, in order to avoid damage to the tendons during the exposure of the anteromedial (AM) tibia. The sartorius fascia is exposed by a sharp dissection and the pes anserinus is then retracted distally with a blunt retractor, exposing the superficial medial collateral ligament (sMCL). A Cobb elevator is used to partially detach the distal sMCL insertion. A blunt Homann retractor is passed deep to the MCL to protect posterior neurovascular structures. Next the medial border of the patellar tendon is identified and protected throughout the whole procedure with a second blunt lever. A guidewire is drilled through the proximal tibia from medial to lateral under fluoroscopic control. The starting point of the wire is the anteromedial tibia at the level of the superior border of the tibial tubercle (about 4 cm distal from the joint line). The wire must be inserted aiming the tip of the fibular head (1 cm below the lateral articular surface) [5, 14, 15]. The tibial osteotomy is performed immediately distal to the guide pin to protect against proximal migration of the osteotomy into the joint (Fig. 22.3). The direction of the osteotomy in the sagittal plane is critical and should be parallel to the proximal tibial joint slope. The tendency to make the osteotomy perpendicular to the long axis of the tibia should be avoided because this will create a very thin bony fragment posteriorly because of the physiological posterior tibial slope [13, 14]. The anterior and medial cortices are cut with a small oscillating saw under direct vision. Then the osteotomy is deepened within 1 cm of the lateral tibial cortex using thin, flexible osteotomes (Fig. 22.3). The osteotomy should be taken to within 1 cm of the lateral tibial cortex, using intermittent fluoroscopy and graduated osteotomies [16]. The mobility of the osteotomy is checked by gentle manipulation of the leg with a valgus force and encouraged, if needed, piling up two or three osteotomes [5, 14, 15]. Graduated wedges are then engaged into the osteotomy and advanced slowly, until the desired opening is achieved. An intact lateral hinge is mandatory to improve the stability of the osteotomy. Intraoperative alignment is checked intermittently under fluoroscopy and, once the desired correction is achieved, with an alignment rod centered on the hip and ankle joints. According to the preoperative planning, the rod should lie at 62.5 or 50 % of the tibial width, as measured from medial to lateral. The sagittal plane correction should also be assessed by fluoroscopy and by looking carefully at the amount of osteotomy opening. Considering the triangular shape of the tibia, if the opening at the level of the anteromedial tibia is half of the opening at the level of the posteromedial tibia, the preexisting slope is maintained. The slope can be adjusted according to the correction planned on the sagittal plane by moving the wedges (and the plate) anterior or posterior. Once the desired correction has been achieved and plate positioning determined, the osteotomy is fixed with a plate and the wedges are removed. Various plates are available for fixation of the opening wedge osteotomy: conventional, locking, butterfly, long or short plates, with or without a spacer [17]. In order to further decrease the tibial slope, one distal screw is positioned and then the knee is kept in full extension while inserting the first proximal screw. In this fashion, the osteotomy gap closes anteriorly and the slope decreases. Fluoroscopic control is necessary to assess proximal and distal positioning of the screws. If a conventional Puddu plate is used, attention should be paid to position the proximal screws more posteriorly than usual, in order to have enough bone for the tibial tunnel, if ACL revision is concurrently performed. For the same reason, when using a long locking T plate (Fig. 22.3), the most anterior screw should not be inserted proximally [17]. Alternatively, all proximal screws are positioned and, if the tibial tunnel is interfering with one of them, this is removed and repositioned. The osseus gap can be filled using the preferred bone graft (autograft, allograft, or substitutes) [17–22]. Corticocancellous autograft or allograft is recommended for an opening measuring >10 mm. Conversely, bone grafting is optional for smaller corrections.


Fig. 22.3
Intra-operative pictures. (a) After positioning the guide wire and cutting the cortex with an oscillating saw, the osteotomy is performed with graduated osteotomes under fluoroscopic control, making sure to leave intact the lateral hinge (1 cm from the lateral cortex). (b) When the bone cut has been completed anteriorly and posteriorly and some degrees of opening are noted with valgus stress, the osteotomy site can be distracted. (c) Plating is performed next
Closing Wedge HTO
Many variations of lateral closing wedge osteotomy have been described in the literature, but all are based on the principle to correct the alignment achieved by removing a laterally based wedge of bone and closing the resultant defect [11, 23–25




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








