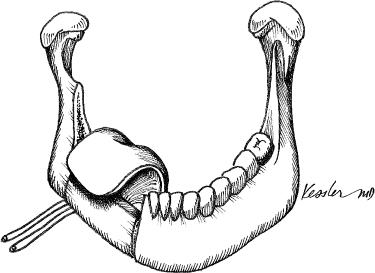
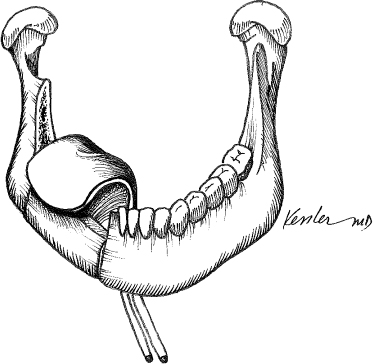
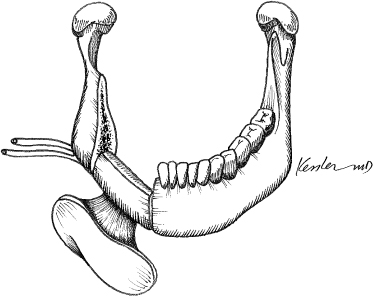
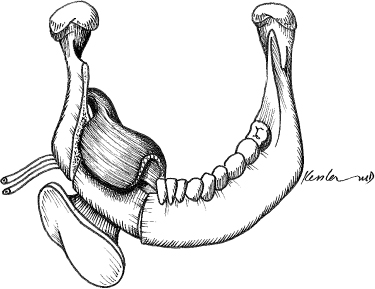
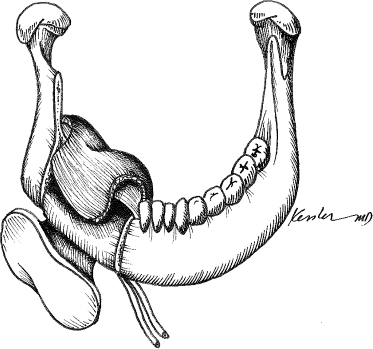
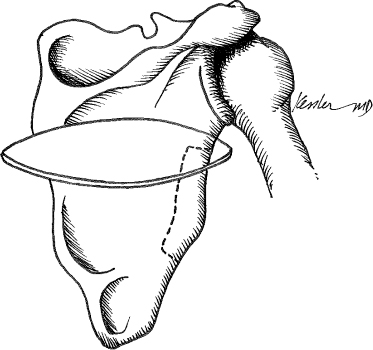
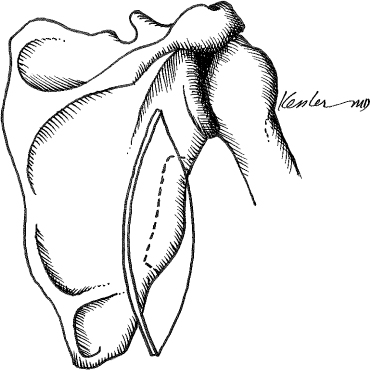
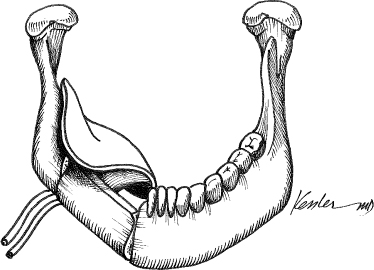
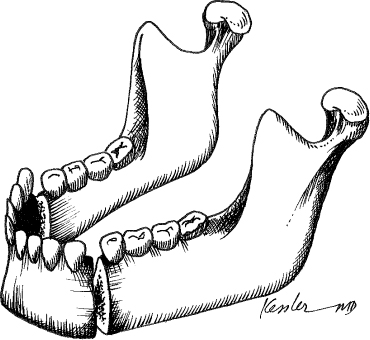
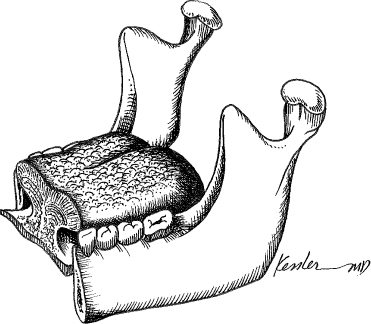
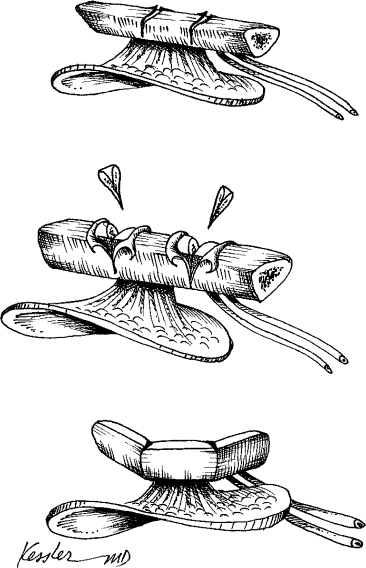
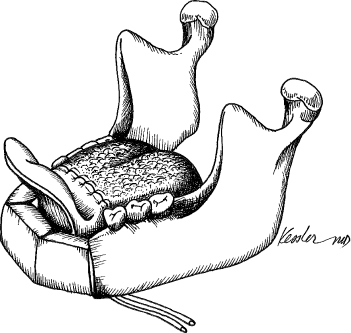
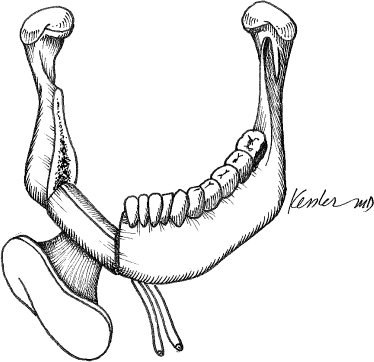
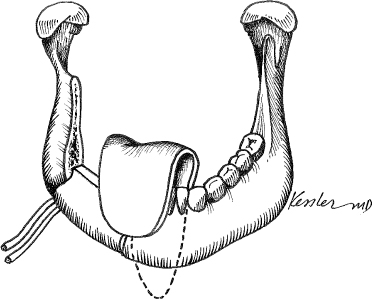
2 The oromandibular complex plays an essential role in mastication, articulation, and cosmetic form. The mandible provides the support and foundation for tongue position and elevation of the larynx during swallowing. Similarly, the tongue and the adjacent buccal anatomy are responsible for articulation of speech and mastication. Oromandibular defects that result from trauma, congenital deformity, or tumor extirpation often have an impact on both form and function. The defect can range from a simple isolated bony defect to a complex defect involving the mandible, tongue, and soft tissue. As a result, the site of the defect and the associated soft tissue defect are the two most important factors in determining the impact of an oromandibular defect on a patient’s function and aesthetics. These factors are also important in determining the most appropriate method of reconstruction. Prior to the introduction of microvascular free tissue transfer, techniques such as free bone grafts, vascularized rib, and alloplasts were commonly employed to restore mandible defects; however, the results were often suboptimal. Many of the techniques were initially developed during the First World War when external fixation and free bone grafts were commonly used as part of a staged reconstruction. Because these techniques were used prior to the advent of antibiotics and rigid fixation, free bone grafts frequently resorbed or became infected.1,2 This was particularly common when defects communicated with the oral cavity because the salivary contamination often infected the bone graft before vascular ingrowth could occur. This contributed to the development of a sequestrum and a persistent fistula. Larger grafts and vascularized rib commonly suffered a similar fate, resorbing over time. The advances in oromandibular reconstruction that followed the Second World War were largely a result of the introduction of both antibiotics and wire fixation. Although reconstructive surgeons were still dependent on free grafts, graft survival improved. In the 1960s and 1970s, prosthetic and allograft mandible reconstruction techniques became popular. Metallic trays filled with cancellous bone and materials such as alloplastic mandibles created out of Silastic, Dacron, and Teflon were popularized; however, infection, exposure, and fracture were common, and these techniques were quickly abandoned.3–6 The introduction of the metallic reconstruction plate in the 1980s provided an improved method for stable fixation of free bone grafts7; however, because nonvascularized bone grafts were used, failure rates remained unacceptably high. Large free graft, in spite of fixation, failed to revascularize, and, as a result, they became weakened and were resorbed. In an early attempt to provide a vascularized bone graft, the pectoralis myocutaneous flap was designed with a segment of vascularized rib. Early results were promising, but longer term results were less encouraging.8 In the mid-1970s, vascularized mandibular reconstruction was introduced and has subsequently become the standard of care for patients with extensive defects of the jaw.9 Initial reports using the vascularized iliac crest were subsequently followed by descriptions of the scapular and fibular donor sites.10–12 Each donor site is distinctly unique. The iliac crest, initially described in association with the groin flap, provides a source of hearty bone stock, vascularized internal oblique muscle, and skin. The vascular supply is the deep circumflex iliac artery and vein. This donor site was especially popular in the 1980s prior to the introduction of the fibular donor site; however, it is less commonly used now because of a variety of drawbacks. Although this tripartite flap provides an excellent source of bone for osseointegration, shortcomings including a short vascular pedicle, the poor reliability of the skin paddle, and the lack of segmental perforating blood vessels, limiting the surgeon’s ability to perform boneshaping osteotomies, which has curtailed the popularity of this donor site. In 1986, the scapular donor site was introduced for mandibular and maxillary reconstruction.13 Often referred to as the subscapular system of flaps, this donor site provides a system of flaps that are ideal for complex head and neck reconstruction. The subscapular artery and vein give rise to the circumflex scapular vessels and the thoracodorsal artery and vein. Because of the rich vascular network, this donor site gives rise to two skin paddles, the parascapular (axial) and the scapular (transverse); two separate vascularized bone grafts, the lateral of the scapula and the scapular tip; and the latissimus dorsi muscle. Because of the wide variation of muscle, skin, and bone flaps, this donor site is often reserved for complex defects or when peripheral vascular disease precludes the use of the iliac or fibular donor sites. The shortcomings of this donor site are limited to the fact that it cannot be harvested using a two-team approach. In our experience, the bone stock is adequate for mandible and maxillary reconstruction. The fibular donor site, introduced in 1989, has become the most popular donor site for mandible reconstruction because of its excellent bone stock, reliable anatomy, and the ability to harvest the flap as a two-team approach.12 The flap is based on the peroneal artery and paired veins. The skin island is based on the perforating vessels, which travel within the posterior crural septum. The skin island can be positioned either intraorally or externally, and this flap can provide up to 25 cm of bone, enough to perform a total mandible reconstruction. Blood supply to the fibula is both intraosseous and segmental, allowing for multiple osteotomies. Although some suggest that the shortcoming of the fibular donor site is the unreliability of the skin island, we find that this occurs in less than 5% of cases. Understanding the anatomy of the oromandibular complex is exceptionally important in determining the optimal approach to reconstruction of this unit. It is also important to understand the relationship between the structure of the mandible and the mobility of the tongue because it is this relationship that is crucially important to form and function of the oral cavity. The mandible serves as a foundation of the oromandibular complex. Although the mandible is a single bone, it is actually composed of two fused hemi-mandibles joined by intramembranous ossification at the midline during development. The fusion of the two hemi-mandibles occurs by the first 24 months of life. The mandible is composed of a horizontal body with a posterior vertical extension termed the ramus.14 On the inner surface of the mandible are the paired superior and inferior mental spines, which represent the areas of attachment of the genioglossus and the geniohyoid muscles. Just lateral to the symphysis on the inner surface of the mandible are two paired protuberances termed the superior and inferior mental spines. The genioglossus muscle attaches to the superior mental spines, and the geniohyoid muscle attaches to the inferior mental spines. The mylohyoid line extends obliquely in a posterosuperior direction from the midline and serves as the attachment site for the mylohyoid muscle that supports the tongue and its associated structures. On the medial surface of the ramus inferior to the mandibular notch is the mandibular foramen that transmits the inferior alveolar nerve and blood vessels. The lingual lies medial to the mandibular foramen, pointing posterosuperiorly toward the condylar head. This landmark can be used to locate the inferior alveolar nerve in cases where the nerve can be preserved. The ascending ramus articulates with the skill base at the glenoid fossa. The condyle of the mandible is secured within the glenoid fossa by the ligaments of the articular capsule. The articular capsule is a loose tissue envelope attached to the superior skull base and attached below to the neck of the condyle of the mandible. The other ligaments that secure the condyle of the mandible into the fossa include the temporomandibular and sphenomandibular ligaments. The temporomandibular ligament is attached above to the lateral surface of the zygomatic arch, and below to the lateral surface of the neck of the mandible. The sphenomandibular ligament is a thin band attached above to the spina angularis of the sphenoid bone and fixed below to the lingula of the mandibular foramen. The articular disk sits in the joint space between the condyle of the mandible and the mandibular fossa. The disk acts to promote free movement of the joint during speech and mastication. The general understanding of the mandibular anatomy is important when considering reconstruction in order to preserve the biomechanics and function of the mandibular complex. Because the loading forces associated with mastication are significant, a general understanding of the mandible biomechanics is important to preserve function and form. Factors that influence the biomechanics of the mandible include the integrity of the temporomandibular joint (TMJ), the bone stock distribution, and the forces associated with scar contracture. The mobility of the TMJ is extensive. The mobility of the TMJ allows for the mandibular depression, elevation, side-to-side movement, and anterior and posterior movement. The TMJ is often referred to as a single joint, yet actually there are two joint spaces, an upper and lower. During speech, the joint movement is confined to the lower of the two joints. When the mouth is opened widely during biting, the lower joint acts as a hinge, whereas the upper joint provides a gliding character. The hinging and gliding movements take place simultaneously during mastication as the condyle rotates on the joint disk. The preservation of the joint biomechanics is ideal during reconstruction of the mandible. Because the complex movements of the TMJ are difficult to reconstruct, the integrity of the joint should be preserved whenever possible. Yet even the most meticulous joint reconstruction fails to provide the complex hingegliding movements of the native joint. The mandible itself is uniquely designed with increased bone stock along the inferior border and anterior aspect of the ascending ramus in response to the forces of mastication. When approaching a mandibular reconstruction, it is ideal to re-create these structures with the biomechanics in mind. A good example is during mandibular reconstruction where it is beneficial to reestablished the inferior border to preserve the integrity of the biomechanical forces of chewing. In addition to the distribution of the bone stock density, the form and contour of the mandible are also important. The contour of the mandible is important to facial symmetry, and the continuity of the mandible is important to oral function. The mandibular arch, for example, serves to anchor the suprahyoid muscles, whereas the mandibular body anchors the mylohyoid muscle, which supports the position of the oral tongue. When either the body or the arch of the mandible is disrupted, the ability to raise the larynx during swallowing or the position of the tongue may be greatly affected, leading to a disturbance in swallowing, speech, and articulation. Scar contracture is the most difficult biomechanical force to account for and often is the most disrupting. This is exemplified by debilitating trismus that often occurs after mandibular reconstruction and external beam radiotherapy. Because external beam radiotherapy is associated with an inflammatory phase during the treatment course and is subsequently followed by a healing phase that results in scar formation, it often causes an irreversible scar contracture of the temporalis muscle, whereas therapy may minimize the extent of the contracture that can cause trismus, shifting of the mandibular complex, and a painful and debilitating cross-bite deformity. In many cases a coronoidectomy performed at the time of the surgery is the most effective way to prevent this chain of events. Although temporalis contracture is rather easy to predict, masseter, pterygoid, and oropharyngeal contractures are more difficult to anticipate as well as more difficult to prevent and manage. Several classification systems have been proposed for the assessment of the mandibular defect15–18; however, none has gained wide acceptance. The failure of any singular system to gain acceptance highlights the complexity of the bony and associated soft tissue anatomy. The first comprehensive classification system was published in the Russian literature by Pavlov15 in 1974. He reviewed 215 cases and divided the cases into three classifications based strictly on the bony defect. Pavlov’s classification system was enlightening, as it recognized the functional and aesthetic importance of the anterior mentum and the condyle. Pavlov wrote, “The most important sign, the presence or the absence of the mental portion of the lower jaw, this largely determines the severity of the clinical picture and the functional disturbances and the complexity of the restorative operations and their results.”15 The classification system, however, was simplistic and failed to recognize the concomitant mucosal defect. The Mount Sinai Group introduced a classification system in 1991 that expanded on Pavlov’s concepts and classified defects based on bone, soft tissue, and neurologic deficits.18 The complexity of this anatomic classification system was overwhelming, offering more than 3500 possible oromandibular defects. Although thorough, this system was too complex, making the design of a reconstructive algorithm impractical. The University of Toronto group subsequently proposed a simpler classification system using upper case letters to denote the bony defect and lower case letters to convey the involvement of skin mucosa, skin, and the combination of skin and mucosa.17 But none of the published classification systems has caught on, and most reconstructive surgeons use a simple description to relate the extent of the defect. Although a classification system has the potential to provide a framework for a reconstructive algorithm, it has proven difficult to relate the functional and aesthetic complexity of a mandibular defect in a simple classification system. Optimal outcomes in oromandibular reconstruction can only be achieved with careful presurgical preparation. When assessing an oromandibular defect, it is important to consider the predicted location of the bony defect, the extent of the associated soft tissue defect, and the plan for dental rehabilitation. The soft tissue defect is typically considered the most important factor when considering reconstructive options. For many years, tongue flaps, skin grafts, and primary closures were used to manage the soft tissue component of the oromandibular defect. These techniques often led to devastating functional deficits because of tethering of the tongue and impaired swallowing and articulation. Free flap lends the unique advantage of providing vascularized bone and a skin paddle that can be used to reconstruct the floor of mouth or tongue without interfering with articulation and swallowing. This is not to say that the extent of the bony defect is not important. In fact, the size of the bony defect will also play a role in determining the options for reconstruction. Bony defects less than 3 cm may be treated with free bone grafts if there is no defect in the lining of the oral cavity. In contrast, bony defects greater than 3 cm. often require a vascularized bone containing free flap, especially if there is an oral mucosal defect. The complexity of the oromandibular complex and the wide range of potential combinations of bony and soft tissue defects make reconstruction of this area most challenging. The plan for dental rehabilitation must be carefully considered well before surgery. Although tissue-borne dentures are common because of the financial burden of osseointegrated implants, implant-borne dentures provide the optimal oraldental rehabilitation. In either case, the re-creation or preservation of a lingual-buccal sulcus is essential to establish retention of the denture. If osseointegrated implants are anticipated, a coordinated presurgical plan should be established with an oral maxillofacial surgeon and prosthodontist. This will facilitate planning of the implant placement that is essential for any stable dental restoration. Finally, mandible reconstruction can be performed either primarily, at the time of extirpation, or secondarily, at a later date. Following the introduction of microvascular free flap reconstruction of the mandible, opponents suggested that primary reconstruction may obscure surveillance and prevent the early detection of recurrence. For this reason mandible reconstruction was advocated as a secondary procedure following a 2-year disease-free interval. Since the early 1990s, advances in imaging have improved surveillance and demonstrated that when the combination of serial imaging and routine physical examination are instituted, primary mandible reconstruction does not adversely affect the early detection of recurrence. There are, however, circumstances when secondary mandible reconstruction may be considered. Specifically, in situations where the bone margins are in question, a secondary reconstruction may be considered. Other considerations include patients who are at high surgical risk because of medical comorbidities, and elderly patients who are frail. Although most surgeons prefer to perform primary mandible reconstruction because it is technically easier, secondary reconstruction may be rarely indicated. Establishing the optimal position of the vascular pedicle and the skin paddle relative to the bone graft prior to surgery requires an understanding of the flap geometry. Because the right-sided donor site provides a very different vascular pedicle and skin paddle geometry than the left-sided donor site, it is important to predict the position of the defect and the donor vessels before choosing a donor side. In general, it is best to plate the bone graft on the surface that will least disrupt the vascular pedicle or periosteal blood supply. To optimize the vascularity of the graft, the plating surface often will dictate the orientation of the skin paddle and the vascular pedicle. When managing a right-side defect, if the contralateral donor site (left) is harvested, this will position the skin paddle intraorally and the vascular pedicle posterior. This geometry is commonly used for most routine composite defects involving the floor of mouth or tongue (Fig. 2.1). In situations where it is desirable to position the vascular pedicle anteriorly, the ipsilateral donor site (right) will position the vascular pedicle anteriorly and the skin paddle intraorally. This geometry is less common but may be necessary when using donor vessels in the neck contralateral to the defect (Fig. 2.2). When it is necessary to position the skin paddle externally and the vascular pedicle posteriorly, the ipsilateral donor site is used. This is common in defects of the external skin (Fig. 2.3). Fig. 2.4 The fibular free flap donor site. When the skin paddle is positioned externally and the vascular pedicle is anteriorly, the contralateral donor site is used. When the skin paddle is positioned externally and the vascular pedicle is anterior, the contralateral donor site is used (Fig. 2.4). The tripartite design of the iliac crest–internal oblique flap lends itself to several orientations depending on whether a skin paddle is harvested with the internal oblique muscle. In general, the muscle is usually oriented intraorally because it is more reliable. When the pedicle is oriented posteriorly, the ipsilateral donor site is harvested. This is the most common orientation because the vascular pedicle is usually positioned posteriorly (Fig. 2.5). In those situations where the vascular pedicle needs to be oriented anteriorly, the contralateral donor site is harvested (Fig. 2.6). Fig. 2.8 The scapular skin paddle orientation is ideal for composite defects combined with an extensive hemiglossectomy or total glossectomy defect. The scapular donor site is the most versatile bone-containing free flap because the skin paddle has great versatility in its ability to rotate, and the skin paddle can be harvested from the scapular or parascapular sites. The scapular skin paddle results in a flap orientation where the vascular pedicle is positioned posteriorly and the skin paddle lies perpendicular to the bone graft. This orientation is ideal for composite defects combine with an extensive hemiglossectomy or total glossectomy defect (Figs. 2.7 and 2.8). The parascapular skin paddle results in a flap orientation where the vascular pedicle is positioned posteriorly and the skin paddle lies parallel to the bone graft. This orientation is ideal for composite defects involving the floor of mouth or tongue (Figs. 2.9 and 2.10). With the exception of the rare isolated bony disease, defects of the anterior mandible nearly always involve the anterior floor of the mouth and in some cases the anterior tongue (Fig. 2.11). In rare cases, they may also involve the anterior lip or chin skin. Anterior mandible defects almost always require reconstruction because of the significant cosmetic and functional impact of this defect. Resection of the anterior mandible leads to a characteristic cosmetic deformity often referred to as the “Andy Gump” deformity, named for the popular comic strip created by Sidney Smith in 1917 parodying a chinless character named Andy Gump. The characteristic chinless appearance is associated with a variety of cosmetic and functional deficits. Unlike other areas of the mandible, the anterior mandible plays an integral role in tongue position and laryngeal elevation. The genioglossus and geniohyoid muscles insert into the mandibular tubercle located on the medial aspect of the anterior mandible. When this insertion is compromised, the tongue will fall back into the pharynx, resulting in glossoptosis. When this dynamic is compromised, glossoptosis usually results in airway obstruction requiring a tracheostomy. Additionally, elevation of the hyoid and larynx that normally occurs during swallowing becomes compromised, resulting in aspiration. Consequently, patients with an Andy Gump deformity are commonly tracheostomy dependent and, in many cases, gastrostomy tube dependent. Unless the mandibular defect is exceptionally small, most anterior mandible defects require free tissue transfer. This is usually because in addition to the bony defect, there is a concomitant soft tissue defect (Fig. 2.12) Although this can be accomplished with any of the three vascularized bone containing free flaps, the fibular donor site provides the optimal source of bone because multiple osteotomies can easily be performed to achieve the curvature of the anterior mandible without compromising the vascular integrity of the graft (Fig. 2.13). The fibular graft also provides a skin paddle that can be designed and rotated to address an anterior floor of mouth–tongue defect or a complex defect eroding through the anterior chin (Fig. 2.14). The most important aspect of the reconstruction lies in anchoring the genioglossus and the infrahyoid complex to the anterior mandible with a nonabsorbable suture to secure the tongue forward and elevate the larynx (Fig. 2.15). For this reason, we advocate using a single reconstruction plate to fixate the bone graft. The reconstruction plate provides the rigidity and fixation necessary to bear the stress of the anchoring sutures without disrupting the bony segments. ♦ When possible, a reconstruction plate should be applied prior to tumor extirpation, especially in the dentate patient. This helps to maintain occlusion following the reconstruction. After fitting and securing the plate, it can be removed to perform the resection (Fig. 2.16). ♦ If a plate cannot be fitted prior to the extirpation because of a deforming lesion that precludes placement of the plate, an external fixation device can be used or the patient can be placed into internal maxillary fixation throughout the resection and fixation of the reconstruction plate. ♦
Oromandibular Complex Reconstruction
♦ RELEVANT ANATOMY
♦ BIOMECHANICAL CONSIDERATIONS
♦ CLASSIFICATION OF OROMANDIBULAR DEFECTS
♦ ASSESSING OROMANDIBULAR DEFECTS
Flap Geometry
The Fibular Donor Site
The Iliac Donor Site
The Scapular Donor Site
♦ THE ANTERIOR OROMANDIBULAR DEFECT
Option for Management: Fibular Free Flap
Surgical Technique and Considerations
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree