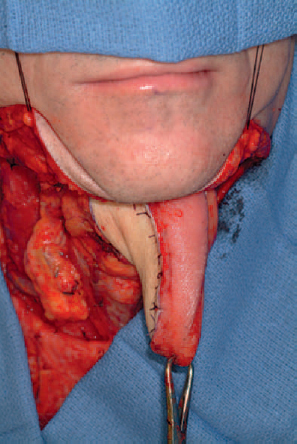
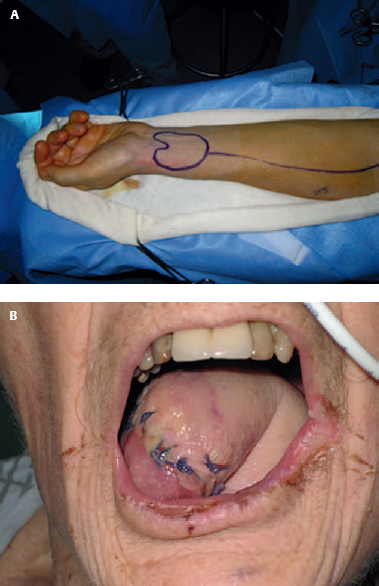
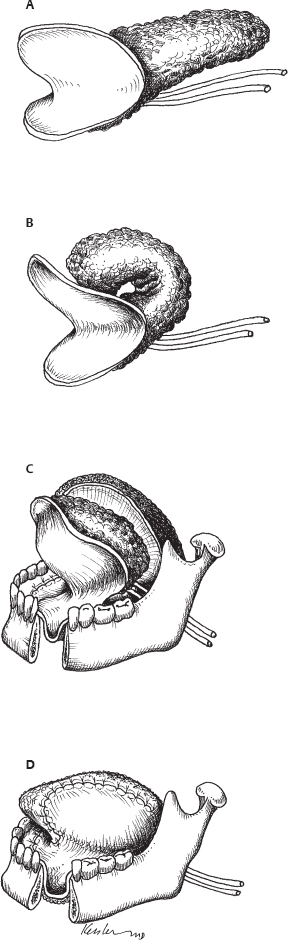
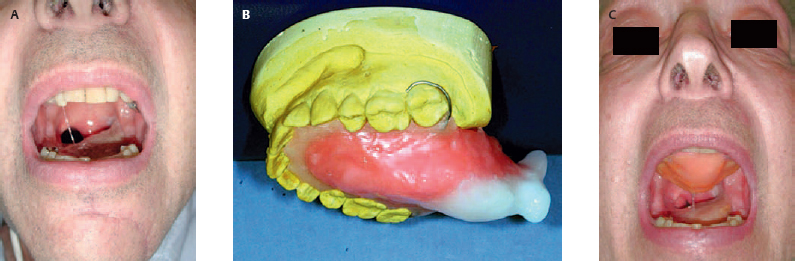
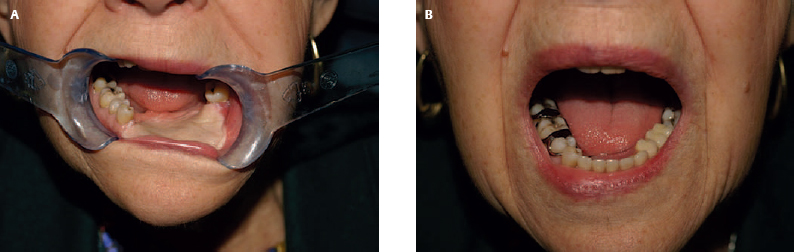
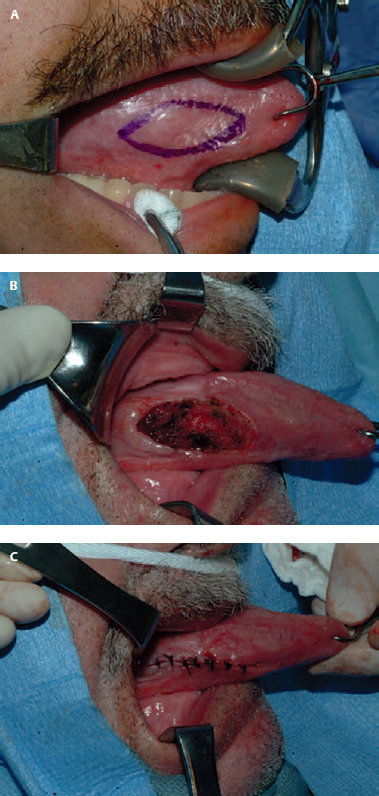
1 In most situations, surgery is the first-line management of oral cavity carcinoma. Thus it is vitally important to consider the impact of surgery and reconstruction on articulation and swallowing. Although the oral tongue is important in the articulation of speech and the oral phase of swallowing, the base of the tongue is important in airway protection and the pharyngeal phase of swallowing. Surgery of the oral cavity often compromises sensation and dynamic motion of the tongue, so reconstructive techniques that result in tethering of the oral tongue nearly always lead to impaired function. Such impairment was common in the 1970s, when tongue flaps and skin grafts were the mainstay of oral cavity reconstruction. In the 1980s, pedicled regional flaps such as the pectoralis and latissimus myocutaneous flaps were introduced. Although these flaps provided an excellent source of tissue for head and neck reconstruction, the pedicled nature of these flaps often resulted in pulling and tethering during the course of healing. This led to impaired movement of the remaining muscular tongue, which in turn translated into poor functional outcomes. The major advantage of free tissue transfer for oral cavity reconstruction is the ability to use pliable soft tissue that contours to the complex anatomy of the oral cavity and moves with the residual muscular tongue. Donor sites such as the radial forearm and anterolateral thigh provide the unique potential for sensory reinnervation.1,2 Although sensory reinnervation has been cited as an advantage for oral cavity reconstruction, the data are less convincing. Restoring the complex anatomy and function of the oral cavity following tumor ablation is a challenge. A thoughtful approach to flap design and an appreciation of the neuromuscular and sensory anatomy are vital to ensure a successful final result. The complexity of speech and swallowing is reflected in the complex neurosensory and neuromuscular anatomy of the oral cavity. The oral cavity is defined as the region extending from the lips to the junction of the hard and soft palate above and to the line of the circumvallate papillae below. The area includes the lips, the buccal mucosa, the upper and lower alveolar ridges, the retromolar trigone, the anterior two thirds of the tongue (oral tongue), the floor of the mouth, and the hard palate. The complex anatomy of the oral cavity includes muscle, nerve, salivary glands, and mucosa. Sensation of the buccal mucosa is provided by the second and third branches of the trigeminal nerve. The buccinator muscle is innervated by the facial nerve. The anterior aspect of the oral tongue is part of the oral cavity, whereas the posterior third of the tongue is part of the oropharynx. The muscles of the tongue include the hyoglossus, styloglossus, and genioglossus. Working with the extrinsic muscles of the tongue, the intrinsic tongue musculature is essential for articulation and swallowing. The styloglossus acts to draw the tongue posterior during swallowing, whereas the hyoglossus flattens the tongue by drawing it toward the hyoid. Both movements are an important aspect of speech and swallowing. The hypoglossal nerve is responsible for motor innervation of the tongue, and the lingual nerve provides sensation for the oral tongue. The floor of the mouth is the area between the mandibular alveolus and the oral tongue. It extends posterior to the anterior tonsillar pillar. The area of the floor of the mouth is composed of a sulcus of mucosa that provides the freedom of the tongue to move without restriction. There are also several important structures in the region including the submandibular duct orifice, the submandibular duct, and the lingual nerve. The goals of oral cavity reconstruction are to preserve the movement of the remaining native oral tongue, provide the appropriate bulk to optimize speech and swallowing, maintain velopharyngeal competence, and preserve sensation. As discussed earlier, the dynamic tongue motion is essential to preserve speech and swallowing. Following tumor ablation, the remaining functional tongue must be free to move untethered, to preserve articulation of speech and swallowing. Equally important is maintaining the bulk of the flap. This is important in preserving the tongue-topalate contact that is essential for articulation. Finally, velopharyngeal closure and sensation are important in both swallowing and speech. If not properly addressed, a soft palate resection can result in either velopharyngeal stenosis or velopharyngeal insufficiency. Reconstruction of the muscular velopharyngeal sphincter should be a priority when the soft palate is involved in the ablative resection. Simply relining the area with a soft tissue flap does not provide the appropriate dynamic closure that is essential for an optimal functional result. Equally important is the role of sensation in swallowing. Although the data related to flap reinnervation are equivocal, maintaining oral mucosa sensation can be very helpful in manipulation of the food bolus.2,3 There is no universally accepted classification scheme for oral cavity defects, largely because there are innumerable potential combinations of defects. Generally, defects of the oral cavity can be classified into the following schema: The ±sign means that the glossectomy defects are designated as associated or unassociated with a floor-of-mouth or mandibular defect, because when the floor of mouth or the mandible are involved, special attention should be directed to the design of the flap to prevent tethering of the oral tongue and to take into account the bony defect. The same concept holds true for buccal defects. The soft palate defects are divided into partial and total defects because in most cases the former allows for restoration of the velopharyngeal muscular sphincter whereas the latter assumes that the muscular sphincter cannot be restored. Although this classification system is simplistic, the components of the system are designed to address the important functional considerations and serve as a guide for reconstruction.4,5 Choosing the appropriate method of reconstruction of the floor of mouth can have a significant impact on oral dental rehabilitation. As discussed earlier, the most important tenet of oral cavity reconstruction is that the tongue must not be restricted or tethered. Although skin grafts, local flaps, and free flaps all represent options for reconstruction, choosing the optimal donor site depends on the extent of the defect and the location of the defect. Small to medium-sized defects of the alveolus and floor of mouth can be managed with a buccal flap, a skin graft, or a free flap. However, defects of the floor of mouth that encroach on the tongue often require free tissue transfer because skin grafts tend to contract, thereby restricting the tongue. Similarly, buccal flaps tend to pull the tongue laterally. Other factors that should be considered are the patient’s goals for oral dental rehabilitation. In those patients who desire osseointegrated implants, the soft tissue reconstruction should be low profile with as little bulk as possible. Thin low-profile tissue allows for better denture retention. Bulky flaps hinder retention of a tissueborne denture and often require revision. The split-thickness skin graft provides an excellent source of thin tissue for floor-of-mouth reconstruction. The split-thickness skin graft is best suited for small to medium-sized defects in which the soft tissue bed is well vascularized and it facilitates graft healing. Because the graft is thin, implantborne and non–implant-borne dentures can be retained quite well and often do not require revision surgery. ♦ The split-thickness skin graft should be harvested at approximately 0.17-mm thickness. The graft should be harvested only slightly larger than the defect so that there is minimal redundancy yet it can accommodate contracture. ♦ The graft should be trimmed to the size of the defect and then sutured into position with an absorbable suture. ♦ After the graft has been sutured into place, a bolster of petroleum-impregnated gauze should be constructed and sutured to secure the skin graft. Fig. 1.2 Clinical case. (A) For the alveolar and floor of mouth defect, the facial artery mucosal muscular (FAMM) flap is designed by using a Doppler to identify the arterial pedicle (arrows). (B) The flap is designed to the appropriate length to provide oral cavity lining. (C) The flap is transferred into the defect and sutured with absorbable suture. The split-thickness skin graft should be used in patients with small to medium-sized defects that do not involve the tongue or ventral surface of the tongue. These areas tend to contract and restrict the tongue motion. The grafts should be used with caution in those patients who have been previously treated with radiotherapy because the grafts have a higher rate of sloughing. Split-thickness grafts often heal well over alveolar bone if the bone is well vascularized and the periosteum is intact. In those cases where the periosteum has been removed, the cortical bone can be drilled down to expose bleeding bone. Postoperatively, we recommend the bolster be kept in place for 5 days. During that time, the patient remains on antibiotic therapy and is placed on a full liquid diet. Dentures are not fabricated for 6 weeks to allow for complete healing. The facial artery mucosal muscular (FAMM) flap is a vascularized pedicled flap based on a branch of the facial artery. The flap can be pedicled superior or inferior depending on the defect location. For most floor of mouth, alveolus, and lateral tongue defects, the inferior-based FAMM flap is appropriate.6 Because the FAMM flap is a pedicled flap, it is well vascularized and is ideal for inferior- located oral cavity defects, even in the setting of prior radiation. ♦ Once the resection is complete, the FAMM flap is designed to the specifications of the defect. Although redundancy is not necessary, it is important to design the flap with enough length to accommodate rotation of the flap without tension (Fig. 1.2A). ♦ The flap can be designed to be pedicled inferiorly for floor-of-mouth and alveolar defects. ♦ The vascular pedicle can be localized using a Doppler. ♦ The parotid duct should be cannulated prior to the flap harvest to prevent injury to the duct. ♦ The flap is then harvested and rotated into the defect. Absorbable sutures can be used to achieve the closure of the donor site and the recipient site (Fig. 1.2B). ♦ Several weeks after surgery, the healing is complete. The flap heals flush with the alveolus and floor of mouth, assuming the natural contour of the oral cavity (Fig. 1.2C). Postoperatively, the patient should be NPO (nothing by mouth) for 4 to 5 days to promote healing. Dental rehabilitation should not begin before 6 weeks following surgery. Patients with alveolar defects and minimal floor-of-mouth defects are ideal candidates for the FAMM flap. This is a reliable and well-vascularized flap that heals and adapts well to the floor-of-mouth mucosa. In some cases, the pedicle of the flap may contract, causing tension or mild trismus. This can be managed by lysis of the pedicle 6 to 8 weeks after the initial surgery. Larger defects of the floor of mouth often require free tissue transfer. The thin pliable tissue of the radial forearm free flap7 is ideal for floor-of-mouth reconstruction. The tissue contracts minimally and in most cases is thin enough to accommodate dentures with minimal revision or tissue thinning. Fig. 1.3 Clinical Case. (A) Larger defects that communicate with the neck can be managed with a radial forearm free flap. The skin paddle contours to the alveolus and floor-of-mouth anatomy. (B) The thin, low-profile skin paddle can accommodate a tissue-borne denture. ♦ The radial forearm flap can be designed to the exact dimensions of the floor-of-mouth defect (Fig. 1.3). ♦ The flap can be sutured into the floor-of-mouth defect with absorbable suture. ♦ No bolster is necessary. ♦ The vascular pedicle can be drawn through a floor-of-mouth defect to align the vascular pedicle with a donor vessel for the microvascular anastomosis. Patients with larger defects of complex wounds that have been exposed to radiotherapy are ideal candidates for the radial forearm reconstruction. Patients with defects that extend onto the ventral surface of the tongue or lateral tongue are also best suited for this reconstruction. Modifications of this flap, such as inclusion of subcutaneous adipofascial tissue in the distal part of the flap to fill dead space under the floor of mouth,8 or use of a bilobed flap for defects involving the floor of mouth and tongue,9 have been described. Postoperatively, we recommend that the patient be NPO for 5 to 7 days to facilitate healing. Dental restoration should not begin before 8 to 12 weeks when the flap has healed to the deep tissue. The partial glossectomy defect can range from a small superficial resection of the lateral tongue to a hemiglossectomy defect. Depending on the size, defects that involve the oral tongue can be managed with a variety of reconstructive options including primary closure, healing by secondary intention, a split-thickness skin graft, a local flap, or a free flap. However, when the floor of mouth is involved in addition to the oral tongue, healing by secondary intention and split-thickness skin graft techniques are less desirable because of the inevitable scar contracture that ensues. Primary closure is not usually an option, and therefore free tissue transfer is typically the primary reconstructive option. Select defects can be managed with regional flaps like the submental island flap10; however, one must consider the potential risk of transferring a submental metastasis into the donor site. In select patients, small defects of the oral tongue can be closed primarily. It is always difficult to exactly determine the threshold for when a defect is best managed with primary closure versus a skin graft versus a free flap. The decision is often based on a combination of experience and instinct. Unlike a skin graft or a free flap, the primary closure technique preserves sensate mucosa, which is helpful in oral rehabilitation (Fig. 1.4). Generally, we suggest that if primary closure appears to tether the tongue from freely moving from side to side, another option should be considered. The radial forearm remains the optimal donor site for oral tongue reconstruction due to its versatility and often excellent functional results.11 The thin pliable tissue allows for contouring to the oral tongue and the floor of mouth in a way that cannot be achieved with other soft tissue donor sites. Other advantages include the ability to reinnervate the flap to provide sensation.1,12 Some clinicians have criticized this donor site because the thin tissue characteristic of the volar surface of the forearm may be inadequate to provide the bulk necessary to fill a hemiglossectomy defect; however, fat can be harvested from the forearm to adequately provide bulk to the flap. Fig. 1.4 (A) Clinical case. A superficial oral tongue cancer. (B,C) A superficial oral tongue defect without involvement of the floor of mouth is amenable to primary closure. ♦ After clear margins have been established, the design of the flap is predicated on the necessity for floor-of-mouth lining and bulk. In most cases, the oral tongue can be reconstructed transorally without the need for a midline mandibulotomy (Fig. 1.5). In some cases, a “pull-through” technique13 may facilitate the resection and the reconstruction (Fig. 1.6). ♦ If floor-of-mouth lining is required, the flap can be designed using a bilobed skin paddle to accommodate the oral tongue defect and the floor-of-mouth lining without tethering the tongue (Fig. 1.7A). ♦ If the floor of mouth is not involved, the flap can simply be designed to accommodate the oral tongue defect. The bilobed flap can be harvested with fat along the vascular pedicle to protect the vessels from thrombosis in cases where there is a high risk of salivary leak (Fig. 1.7B). ♦ When bulk is required, vascularized fat can be harvested along the proximal aspect of the flap (Fig. 1.8A). ♦ The flap can then be designed such that the vascularized fat is rolled under the skin paddle (Fig. 1.8B). ♦ This provides the increased flap volume that is important for preservation of speech (Figs. 1.8C,D and 1.9). ♦ The flap should be designed to accommodate the defect with marginal redundancy. ♦ The vascular pedicle should be drawn into the neck medial to the mandible to eliminate compression of the pedicle. ♦ After the tongue defect has been reconstructed, the microvascular anastomosis can be performed. ♦ When choosing a donor vessel, kinking should be minimized. The transverse cervical vessels provide excellent geometry for flaps with a longer vascular pedicle. Fig. 1.9 Clinical example of the radial forearm flap and vascularized fat graft used to add volume to the radial forearm skin paddle. Superficial defects of the tongue heal well either with a split-thickness skin graft or by secondary intention. More substantial defects often require free tissue transfer. In most patients, the radial forearm provides an excellent source of tissue; however, in thin patients, either a vascularized fat flap or an alternative donor site, such as the anterolateral thigh or lateral arm, may provide the bulk necessary to optimize function. In those patients who sustain sacrifice of the lingual nerve, reinnervation of the flap can be beneficial to long-term function. Establishing the appropriate bulk is important to optimize articulation. Postoperatively, patients remain NPO for 5 to 7 days depending on their nutritional status and prior radiation history. For those with poor nutritional status, or who have been treated with external beam radiotherapy, we prefer to delay oral feeding for 10 to 14 days. When the oral tongue defect extends posteriorly to involve a portion of the base of tongue, a thin anterior flap with bulk in the posterior aspect of the reconstruction may be desirable. The lateral arm flap14 has the advantage of providing minimal thickness in the distal flap and more bulk proximally. This unique characteristic provides the opportunity to restore the anterior tongue with the distal portion of the flap, and the base of tongue with the proximal aspect of the flap. ♦ Once the tumor margins have been established, the flap can be designed. The thin tissue located in the distal aspect of the flap will be oriented anteriorly, whereas the proximal, more bulky tissue will be oriented to the posterior defect, where bulk is desirable. ♦ Because the lateral arm vascular pedicle is shorter that the radial forearm flap, the vascular pedicle can be oriented to the facial or superior thyroid vessels. ♦ The lateral arm flap also has the advantage of sensory reinnervation, and, if indicated, the flap can be innervated via the lingual nerve. This donor site is ideal for defects involving the oral tongue and a portion of the base of tongue. Because the vascular pedicle is shorter than that of the anterolateral thigh and radial forearm flaps, this donor site can be a challenge in patients with a vessel-depleted neck. Postoperatively, patients remain NPO for 5 to 7 days depending on their nutritional status and prior radiation history. For those with poor nutritional status or who have been treated with external beam radiotherapy, we prefer to delay oral feeding for 10 to 14 days. The total oral glossectomy defect can be managed using a variety of donor sites, such as the anterolateral thigh flap, the radial forearm flap, or the lateral arm flap. Each has advantages and disadvantages. Other reconstructive options have been described including the submental island flap and the pectoralis flap. Regardless of the donor site choice, functional success is largely dependent on the ability to preserve base-of-tongue mobility and oral neotongue bulk. The integrity of the hypoglossal nerve and base-of-tongue innervation is essential to provide airway protection and preserve the oropharyngeal phase of swallowing. When movement of the base of tongue is compromised, the risk of aspiration rises. Similarly important is the neotongue bulk, which is essential to preserve speech and articulation. Planning the reconstruction such that the oral neotongue maintains bulk is important for long-term function. When the base-of-tongue movement is preserved and the oral tongue bulk is established, the functional results of a total oral tongue reconstruction can be exceptional. In contrast, when the reconstructed tongue is unable to contact the hard/soft palate complex, articulation and speech intelligibility can be severely compromised. In those cases where the bulk is insufficient, a “palatal drop prosthesis” can be used to improve the neotongue-palate contact (Fig. 1.10). This technique, although effective, is not well tolerated because most patients have been treated with radiotherapy, making retention of the obturator difficult. The anterolateral thigh flap has gained great popularity for head and neck reconstruction because of its reliability and diversity.15 It is also associated with minimal donor-site morbidity relative to other donor sites.16 The bulk of the anterolateral thigh flap can be variable depending on the body habitus of the patient. In thin patients, adjacent vascularized fat or de-epithelialized skin paddle can be harvested and rolled under the skin paddle to increase bulk. More commonly, this donor site may provide too much bulk, and alternative sites such as the lateral arm or radial forearm will need to be considered. In the appropriate patient, the anterolateral thigh flap can provide an excellent donor site option. ♦ After confirming negative margins, the reconstruction can be planned. In most cases, the oral tongue can be reconstructed transorally without the need for a midline mandibulotomy. ♦ If there is no connection between the floor of mouth and the neck, a tunnel should be created to pass the vascular pedicle from the oral cavity into the neck where the microvascular anastomosis will be performed. ♦ The flap can be designed in a shape that accommodates the defect. Fat can be harvested with the flap to improve the bulk, and in patients who have been previously treated with radiation, muscle can be harvested to improve healing. ♦ Once the flap is inset, the microvascular anastomosis can be completed. The most common problem with complete oral tongue reconstruction is anterior ankyloglossia. This creates difficulty with both articulation and swallowing. The oral phase of swallowing requires that the tongue force the food bolus into the posterior aspect of the oral cavity. Ankyloglossia inhibits this mechanism, and patients often complain of food being stuck in their mouth and being unable to initiate the pharyngeal phase of swallowing. The bulk of the anterolateral thigh flap may be important in achieving neotongueto-palate contact but may impede anterior neotongue mobility. In patients with bulky thigh tissue, the radial forearm with a vascularized fat flap may represent a better option. Postoperatively, the patient is kept NPO for 7 days. We initiate swallowing exercises on postoperative day 5 followed by an oral diet trial on postoperative day 7. The total oral glossectomy can be managed with the radial forearm flap if vascularized fat is harvested with the flap to achieve and maintain the bulk of the oral neotongue. The advantages of the radial forearm donor site include the ability to reinnervate the flap, and the pliability of the tissue lends itself to the complex contours of the floor of mouth. ♦ Once the ablation has been completed and the margins have been assessed, the flap can be designed. When the entire oral tongue has been resected, the flap can be designed with a wide skin paddle to accommodate the floor-of-mouth lining. The wide design also provides the architecture necessary to maintain the height of the flap within the oral cavity. ♦ The flap should be designed with a strip of vascularized fat to maintain the bulk. This will improve speech and articulation. ♦ The skin paddle can be sutured to the remaining floor of mouth mucosa with absorbable suture.
Oral Cavity Reconstruction
♦ RELEVANT ANATOMY
♦ EVALUATION OF THE ORAL CAVITY DEFECT AND BIOMECHANICAL CONSIDERATIONS
♦ CLASSIFICATION OF ORAL CAVITY DEFECTS
♦ THE ORAL CAVITY DEFECT
The Floor of Mouth
Option for Management: Split-Thickness Skin Graft
Surgical Technique and Considerations (Fig. 1.1)

Patient Selection and Perioperative Management
Option for Management: Facial Artery Mucosal Muscular Flap
Surgical Technique and Considerations
Patient Selection and Perioperative Management
Option for Management: Radial Forearm Free Flap
Surgical Technique and Considerations
Patient Selection and Perioperative Management
♦ THE PARTIAL GLOSSECTOMY DEFECT
Option for Management: Primary Closure
Option for Management: Radial Forearm Free Flap
Surgical Technique and Considerations
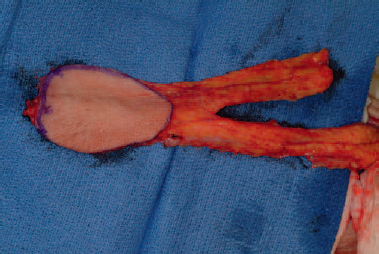
Patient Selection and Perioperative Management
Option for Management: Lateral Arm Flap
Surgical Technique and Considerations
Patient Selection and Perioperative Management
♦ THE TOTAL ORAL GLOSSECTOMY DEFECT
Option for Management: Anterolateral Thigh Free Flap
Surgical Technique and Considerations
Patient Selection and Perioperative Management
Option for Management: The Radial Forearm Free Flap
Surgical Technique and Considerations (Fig. 1.11)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree