APPENDIX 2 Evaluation of Vulvovaginal Disease
The evaluation of chronic vulvovaginal disease differs somewhat from that of skin disease appearing on other skin surfaces. An understanding of several general principles of the diagnosis and evaluation of skin disease or symptoms of vulvovaginal skin allows for better care (Table A2.1).
Table A2.1 Issues in the Evaluation of Women with Chronic Vulvovaginal Symptoms
| Normal variants can be confusing |
| Subtle abnormalities sometimes cause marked symptoms |
| Vulvovaginal symptoms are often multifactorial |
| Iatrogenic disease is common |
| Morphologic appearance of diseases tends to be nonspecific |
| Many inflammatory diseases produce scarring |
Normal variants often mimic skin disease. There is wide variation in the shape, size, and symmetry of the labia minora. Some women have very small labia minora, whereas other women have large, redundant labia minora, sometimes asymmetric, and sometimes extending well below the labia majora. The origin of the labia minora is sometimes bifid, originating both from the clitoral frenulum and the edge of the clitoral hood or the medial labium majus (Figure A2.1).

Figure A2.1 Erythema of the modified mucous membranes of the vulva is not necessarily a sign of inflammation.
Most asymptomatic premenopausal women exhibit erythema of modified mucous membranes, and redness is more marked in light-complexioned women. This normal erythema of modified mucous membranes is often misinterpreted by the patient and the examiner as inflammation (Figure A2.2).
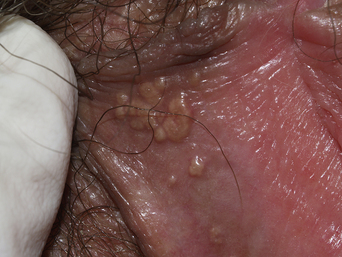
Vulvar papillomatosis is sometimes mistaken for genital warts. These tubular projections are characterized by rounded tips and symmetrical distribution. Clusters of lesions show papillae that are discrete to the base, whereas genital warts produced by papillomavirus infections are fused at the base. Vulvar papillomatosis classically occurs in the vestibule, but can be seen on any surface of the modified mucous membranes (Figures A2.3–A2.5). The ostia of the vestibular glands appear primarily just external to the hymeneal caruncles, but they are sometimes seen in other areas of the vulva (Figure A2.6). These ostia range from a few to many, and they are generally symmetrical. Fordyce spots consist of enlarged sebaceous glands manifested by lobular, hypopigmented to yellowish papules which are most often noted on the medial aspect of the labia minora, but can occur on any aspect of the modified mucous membranes of the vulva except for the vestibule (Figure A2.7). While Fordyce spots vary in size and number, these are normal findings in the premenopausal woman, and they do not cause symptoms.

Figure A2.5 Vulvar papillae are found not only in the vestibule, but sometimes on the labia minora as well.

Figure A2.6 The ostia of vestibular glands are occasionally obvious, appearing as red or skin-colored pits.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree