Chapter 4
SURGERY OF THE UPPER EYELID AND THE BROW
John L. Wobig and Roger A. Dailey
Throughout this book, reference will be made to the use of the CO2 laser as a useful surgical adjunct. These lasers have been employed for facial surgery since the early 1980s. They operated, however, only in a continuous wave mode, which, when used on the skin, often produced an unacceptable scar. The development of a superpulsed wavelength with a pulse duration shorter than the thermal relaxation time of skin has significantly broadened their clinical application. For facial surgery, the Nidek Unipulse Laser (Nidek, Inc., Freemont, CA) is set at 10 to 12 W in the superpulsed or Unipulse mode. Deeper dissection is accomplished with the same power setting in continuous wave mode. It is imperative to protect the patient’s eyes with sanitized stainless steel shields. A complete discussion of safety recommendations and laser skin resurfacing is beyond the scope of this book, but many excellent sources of this information are listed in the references
BLEPHAROPLASTY
The term dermatochalasis is generally used to refer to redundant skin of the eyelids. The term has been inappropriately used as a synonym for blepharochalasis, a condition characterized by multiple bouts of lid swelling resulting in ptosis, local atrophy, and scarring of eyelid and periorbital structures. Blepharoplasty is the surgical procedure used to relieve excess tissue and fullness of the eyelids. The technique is essentially the same whether surgery is performed for functional or cosmetic reasons.
CONVENTIONAL BLEPHAROPLASTY
Preoperative Preparation
The patient is seated and asked to look straight ahead. The lateral extent of excess skin is noted and marked. The incision line should generally not extend temporally beyond the beginning of the lateral orbital rim and should ideally align with an existing skin relaxation line. The lower limb of this mark should be at least 5 mm above an incision marked for skin removal in a lower lid blepharoplasty (Figs. 4-1 and 4-2).
If an excess skin fold extends beyond the lateral orbital rim, a brow lift rather than direct skin excision should be considered. The medial incision line is marked ~ 8 mm above the puncta and carried no more than 3 mm medially in a slightly superior direction, following skin relaxation lines. To avoid unsightly webbing, the incision should not extend beyond an imaginary line drawn vertically from the central aspect of the caruncle. Redundant skin in the medial canthal area may be secondary to medial eyebrow and glabelar ptosis, full correction of which may require a brow elevation. Medial W-plasty has also been described; however, direct skin excision alone will not correct all skin redundancy if the brows are ptotic. In fact, it may create unsightly visible scars and medial webbing (correction of brow position abnormalities is beyond the scope of this module; readers are encouraged to familiarize themselves with these abnormalities and methods of surgical correction). In this situation, the medial brows and glabelar skin must be elevated via an endoscopic brow lift to alleviate the redundant skin in this area.
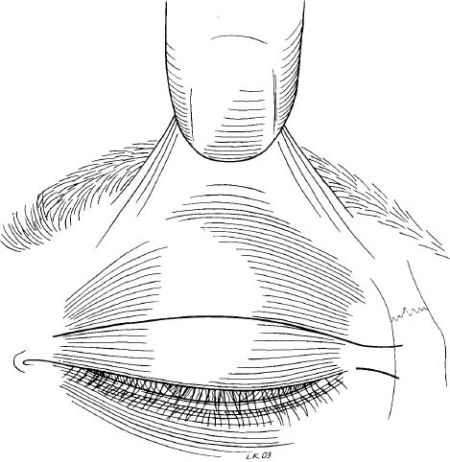
The patient is instructed to gently close his or her eyes. Using a nontoothed forceps, the central redundant tissue above and including the lower mark is grasped in a “pinch” technique so that the eyelashes are slightly everted (Fig. 4-3). The superior edge is marked no closer than 10 mm to the brow (Fig. 4-4). Because some patients pluck their eyebrow hairs, the interface of thin lid skin and thicker brow skin should be used as the superior landmark for this measurement. The experienced surgeon may modify incision placement to give the desired result. In general, 20 mm of skin should be left between the inferior brow border and the lash line. The other lid is then marked in the same fashion. Measurements from the lid margin and brow to skin resection should be the same, but modification may be required if the two eyes are asymmetrical. For symmetry, it’s what is left behind, not what is removed, that counts.
The patient is then placed in a supine, slightly reverse Trendelenburg position on the operating chair. Local anesthetic is given. The patient is then prepped and draped loosely in a sterile fashion, with the entire face exposed to minimize facial soft tissue distortion secondary to traction by adherent drapes.
Surgical Technique
Surgery of the upper eyelid is enhanced with the use of local anesthetic with epinephrine with Wydase (hyaluronidase). There is better control of bleeding, the structural planes are more easily followed, and the patient is awake and can respond to requests for movement of the eyelids. When a comfortable position has been established for the patient, anesthetic is infiltrated slowly into the upper lid using a 5/8-inch, 30-gauge needle and a mixture of 2.0% lidocaine and epinephrine 1:100,000 with hyaluronidase (Wydase) 150 μm per 20 mL. The speed with which an operation is performed is far less essential than the careful preservation of normal tissue and function. In other words, one should make “the technique conform to the anatomy” and inflict minimal trauma.
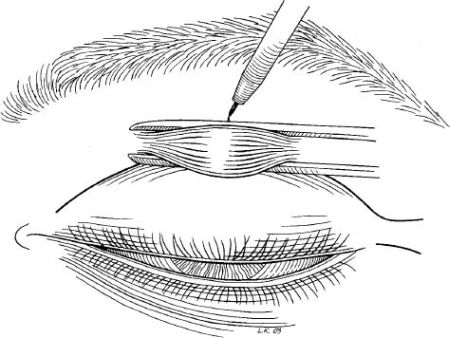
Approximately 10 minutes after the anesthetic has been administered, vasoconstriction from the epinephrine is established and surgery may commence. The skin is incised and can be resected alone or as a skin-muscle flap (Fig. 4-5). The surgeon and assistant must make every effort to stabilize the skin to avoid errant incisions and be prepared to move quickly should the patient sneeze or cough. If only skin is removed, this should be followed by removing a small strip of preseptal orbicularis. Hemostasis is then meticulously achieved with any of several types of cautery [i.e., wet-field, radiofrequency bipolar, thermal high-temperature (2200°F), or unipolar (Bovie)] (Fig. 4-6).
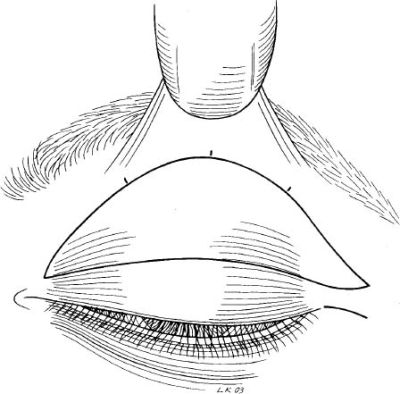
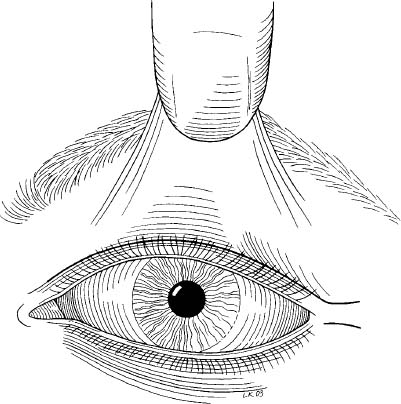
FIGURE 4-4 The superior edge is marked for incision no closer than 10 mm to the brow.
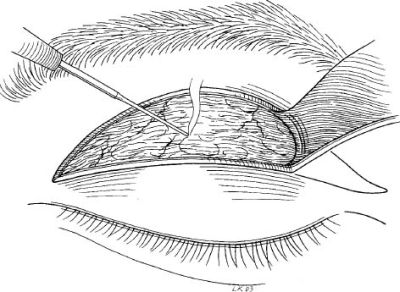
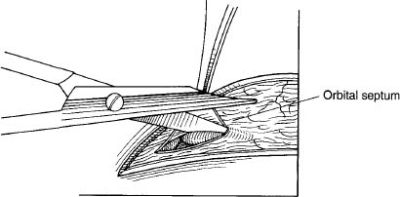
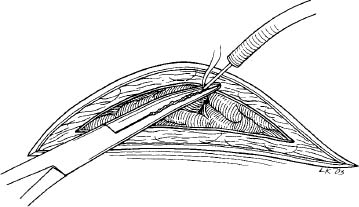
The orbital septum is identified and incised (Fig. 4-7). The preaponeurotic fat pads can be identified through septal pockets or after complete horizontal “open-sky” opening of the septum. Slight pressure applied with the surgeon’s finger to the globe through the closed eyelid will prolapse the fat pads (Fig. 4-8). If the lacrimal gland prolapses temporally, it should be repositioned (dacryopexy) at the time.
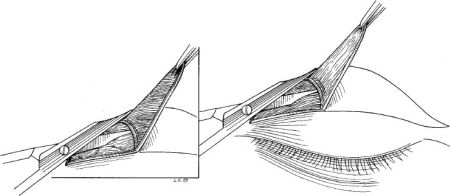
FIGURE 4-5 Incised skin shown resected as a skin-muscle flap and as a skin-only flap.
FIGURE 4-6 Cautery to achieve hemostasis.
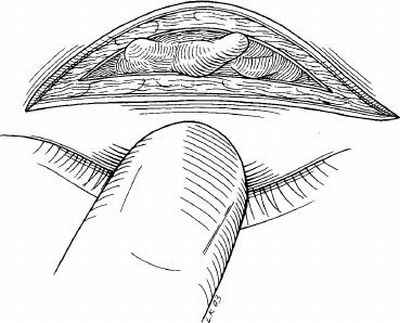
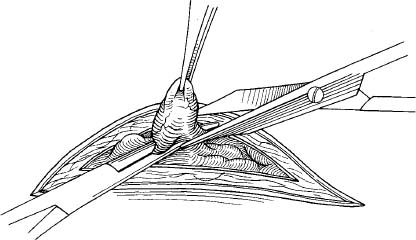
Once the fat pads are identified and dissected free of septal tissues and their own capsule, they can be debulked. Injection of a small amount of local anesthetic into the fat prior to manipulation affords the patient greater comfort. With the fat pad on gentle traction and fully visualized, a hemostat is applied at the base of visible fat and the fat is resected (Figs. 4-9 and 4-10). The cut end is cauterized prior to release of the hemostat and retraction of the fat. Alternatively, bipolar cautery can be used to “crimp” the fat prior to resection to avoid clamping. Fat may also be removed by direct incision using scissors, cutting cautery, or radiofrequency techniques. The nasal fat pad is easily overlooked or only partially resected. To avoid this, redrape the skin and have the patient abduct the eye on the operative side or apply mild manual globe pressure. If a bulge is still present nasally, further dissection and removal of that fat pad should be undertaken.
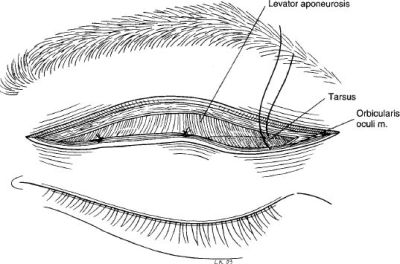
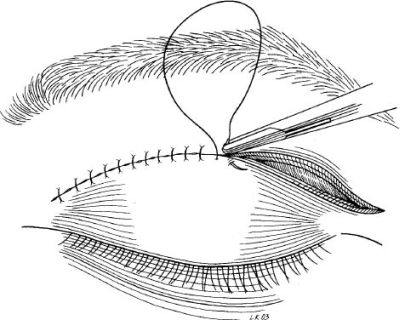
At this point, a well-defined crease or crease elevation can be achieved by performing supratarsal fixation, which involves suturing the orbicularis muscle of the inferior skin edge to the levator aponeurosis at the desired height using interrupted absorbable suture (Fig. 4-11). Alternatively, this can be accomplished by incorporating the levator at the appropriate level into the skin closure (Fig. 4-12).
Attention is then directed to the other lid, where an identical procedure is performed. When meticulous hemostasis has been obtained, the skin edges are approximated with a suture of the surgeon’s choice. The authors typically use 7-0 nylon placed in a running fashion or 6-0 Prolene placed in a subcuticular fashion. The medial 3 to 5 mm of the wound are left unsutured to avoid “bunching” of the tissue and an unsightly scar.
LASER BLEPHAROPLASTY
The continuous wave CO2 laser with a wavelength of 10,600 nanometers was first introduced by Patel in 1964. This laser works on the basis of selective photothermolysis principles. Different substances (chromophores) absorb laser energy to different degrees. It turns out that water (found in human soft tissues) absorbs CO2 laser energy very well and is thus an excellent chromophore. If the laser energy is delivered in a focused fashion, excellent ablation of tissue occurs, with some adjacent thermal devitalization. This adjacent area is referred to as the berm. Use of the continuous wave CO2 laser for blepharoplasty was reported by Dr. Sterling S. Baker in 1984. A marked increase in popularity was experience in the early 1990s with the development of superpulsed CO2 lasers that could ablate tissue efficiently with little collateral thermal damage (i.e., a narrower berm). A blepharoplasty performed with the CO2 laser is initiated and completed in much the same way as the conventional blepharoplasty described in the preceding section. Rather than review the entire procedure, just the substantive differences will be highlighted in this review.
Equipment and Safety
There are several procedural and equipment considerations that one must make before embarking on use of this laser. The laser is a powerful and in some ways dangerous tool. Operating room committees typically designate a laser safety officer to assure safety of the patient and demand that ANSII guidelines are adhered to. At a minimum, a laser sign should be on the closed door of the operating room where the laser is being used. No flammable gases or solutions should be used in this area simultaneously with the laser. Each member of the staff should be well versed in the safety considerations related to the laser. Everyone in the room should wear safety lenses specifically designed to prevent eye injury from a deflected laser beam of 10,600 nm. The patient’s eyes should be protected with sanitized or anodized stainless steel shields.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree