Chapter 7
SURGERY OF THE MIDFACE, LOWER FACE, AND NECK
John L. Wobig and Roger A. Dailey
MIDFACE LIFT
The preoperative exam of the patient presenting for lower eyelid blepharoplasty should include evaluation of the relationship of the lower eyelid to the midface region, including the position of the suborbicularis oculi fat (SOOF), cheek pad, and bony support of the maxilla. Patients possessing prominent globes and an inadequate inferior orbital rim projection are prone to developing postoperative lower eyelid retraction, particularly following transcutaneous procedures. The midface can be approached through either an eyelid incision (infraciliary or transconjunctival) or a combined gingival buccal incision and temporal endoscopic approach.
Midface elevation or augmentation can improve not only functional results but cosmetic outcomes as well. These techniques are essential to master for surgeons operating on the lower eyelids.
SUBORBICULARIS OCULI FAT LlFT
For the subset of patients requesting lower-eyelid blepharoplasty who possess the “double-convexity” deformity, performing a SOOF lift in conjunction with a transconjunctival blepharoplasty can achieve a single smooth contour to the lower eyelid and midface region. The lower convexity is corrected by lifting and securing the SOOF to its original position at the infraorbital rim, whereas the superior convexity can be improved by the judicious removal of orbital fat. If the SOOF descent is not addressed in such patients, the malar convexity may become more conspicuous when an adjacent lid concavity is created by orbital fat removal, leaving the patient with a concavity-convexity deformity. Raising the SOOF can reposition the midfacial tissues and creates a youthful anterior projection to the midface, often obviating the need to remove as much if any orbital fat. This safe, “deep-plane” midface-lifting can be an adjunct to facial rhytidectomy as well as numerous reconstructive procedures in the lower eyelid when there is a vertical inadequacy of anterior lamella.
A related category of patients that may achieve a functional benefit from SOOF lifting are those patients who present with preexisting scleral show, prominent globes, and hypoplastic malar regions. These patients possess an inadequate bony projection of the inferior orbital rim and subrim maxillary bone. In this setting, midfacial descent typically occurs at an earlier age, and there can be functional lower eyelid problems such as corneal exposure or frank ectropion. Such patients are also at high risk for developing postoperative lower eyelid retraction, and horizontal tightening procedures by themselves will not provide enough elevation or support to the lower eyelid. In fact, tightening the lower eyelid in patients with prominent globes may result in further descent of the eyelid underneath the globe. Conversely, performing a SOOF lift suspends and supports the lower eyelid and achieves a vertical augmentation of the anterior lamella. Combining the placement of a subperiosteal alloplastic implant (Flower’s tear trough implant) with a SOOF lift can give a dramatic and long-lasting result in such patients because both the structural and the soft tissue deficits are corrected.
PREPERIOSTEAL APPROACH
SOOF lifts can be accomplished in the preperiosteal or subperiosteal plane. In cases that require only a few millimeters of cheek elevation, a preperiosteal dissection can be performed. This area can be approached through either a transconjunctival or a subciliary incision.
Surgical Technique
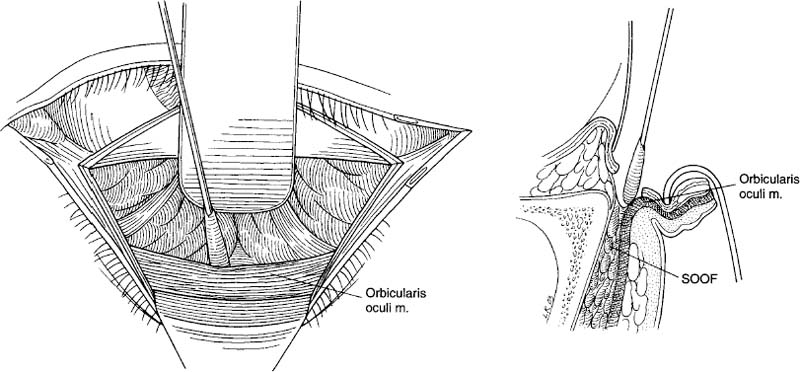
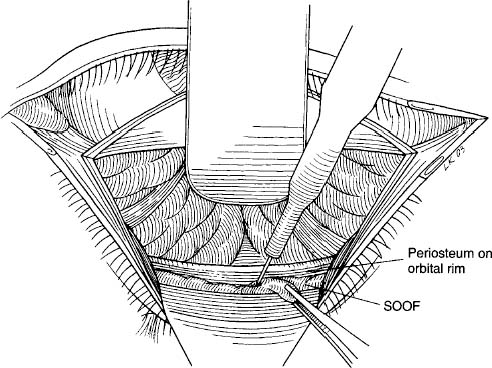
The lower eyelid and cheek are infiltrated with a solution of 1% lidocaine with epinephrine and hyaluronidase (Wydase) mixed 50:50 with 0.5% Marcaine (bupivacaine hydrochloride). Infraorbital and zygomaticofacial nerve blocks can also be given. An 8 mm horizontal line extending laterally from the lateral canthus is drawn with a marking pen and the skin-muscle incision is made with a surgical blade or laser. A lateral canthotomy and cantholysis are then performed. The lower lid can now be retracted with a Desmarres retractor and a transconjunctival incision is made approximately halfway between the fornix and the inferior border of the tarsus. The retractors are also severed with this incision. A 4-0 silk suture can be placed through the cut edge of the retractors and used to provide superior retraction of the retractors (Fig. 7-1). The orbital fat is retracted superiorly as well with a broad ribbon retractor. A cotton-tipped applicator is then used to follow the orbicularis oculi to the orbital rim. Inferior to the rim and arcus marginalis, a fat layer will be visible posterior to the orbicularis oculi. This represents the SOOF (Fig. 7-2). This fat differs from orbital fat in that it is inferior to the orbital rim and overlies the maxillary bone. It is slightly more yellow in color and tougher in consistency.
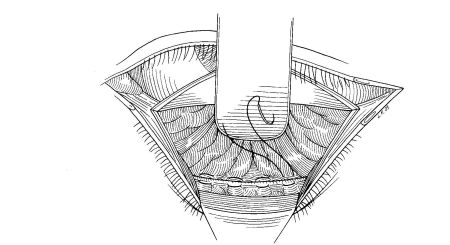
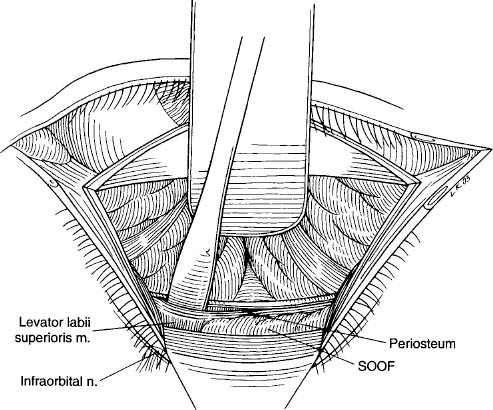
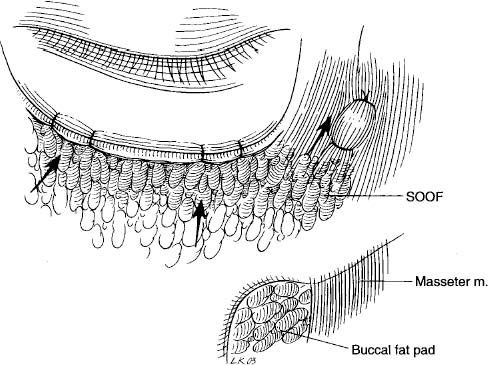
An incision is made between the periosteum and the SOOF from the medial to the lateral position. The dissection is continued interiorly, parallel to the face of the maxilla, in the preperiosteal plane. Care is taken to avoid the infraorbital neurovascular bundle (Fig. 7-3). A Brown-Adson forceps is used to grasp the SOOF in multiple locations, and it is elevated while the surgeon checks to see that this produces the desired elevation of the cheek. If not, further dissection is performed until elevation is correct. Once the cheek has been adequately mobilized, four to five 5-0 Vicryl sutures are placed in a horizontal mattress fashion to suspend the SOOF from the arcus marginalis along the entire length of the rim (Fig. 7-4). It is important that the suture passing through the SOOF not be placed too anteriorly because this will cause dimpling of the skin. Once the cheek tissues are elevated, the lateral canthal region can be reformed as previously described. The transconjunctival wound can be left open or closed with a single 5-0 Fast Absorbing Plain Gut suture.
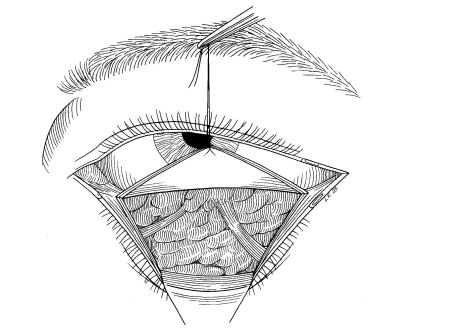
FIGURE 7-1 A 4-0 silk suture is used to provide superior retraction.
SUBPERIOSTEAL APPROACH (PERIOCULAR INCISION)
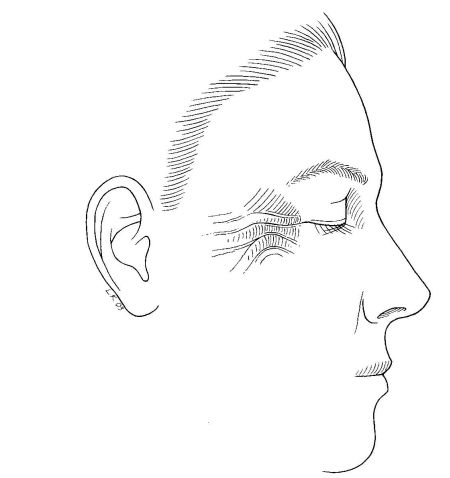
This procedure can be performed through a transconjunctival or transcutaneous, subciliary incision. The subperiosteal midface lift can also be performed through a completely endoscopic approach from a temporalis scalp incision or in combination with an intraoral incision. The endoscopic approach will be discussed later. The periocular approach is somewhat limited by the amount of elevation needed. If significant elevation is needed and the patient has a fair amount of redundant forehead and midfacial skin, a “standing wave” deformity will be created laterally unless a temporal brow lift is performed at the same time (Fig. 7-5).
Surgical Technique
Once the orbital rim has been identified in the same fashion as previously described for the preperiosteal approach, the periosteum can be incised 3 to 4 mm inferior to the orbital rim. This leaves a rim of periosteum from which the cheek will be suspended. A periosteal elevator is then used to lift the periosteum off the face of the maxilla and zygoma. As the dissection proceeds inferiorly, one encounters the infraorbital neurovascular bundle. Because fibers of the levator labii muscle are in close proximity to the nerve, it is useful to dissect the muscle fibers medial and lateral to the nerve, disinserting the muscle and allowing the nerve to become visible (Fig. 7-6). Four separate branches of the nerve may be seen coming through the infraorbital foramen. It is important that as the dissection proceeds laterally, it be maintained in a subperiosteal plane. As the surgeon approaches the masseter muscle, there is a dense adhesion between the periosteum and the insertion of the muscle. This attachment, the zygomatic and masseteric ligaments, is similar to the “conjoined fascia” seen in the temporalis region. This attachment over the medial one-third of the zygoma and at the origin of the masseter should be released completely. One must be careful dissecting along the fibers of the anterior masseter muscle more inferiorly, so as not to damage branches of the facial nerve that travel along the surface of the muscle.
The entire midfacial periosteum is now elevated, but only partial mobilization of the cheek is possible because the periosteum has not been released. With cutting cautery or digital blunt dissection, the periosteum is released and stretched. Separation of the periosteum inferiorly will reveal a soft yellow fat pad, which is the inferomedial buccal fat pad. The entire cheek is now mobile and suspended from the arcus marginalis with several 5-0 Vicryl mattress sutures and the intermediate temporalis fascia with a 4-0 Prolene suture (Fig. 7-7).
The vector of pull is extremely important and varies somewhat depending on the contour of the midface. Medial to the pupil, the SOOF is pulled superomedially. Lateral to the pupil, the vector of pull is superior. Lateral to the lateral canthus, the vector of pull is superolateral to the intermediate temporalis fascia. This multivectoral lift helps to correct the infraorbital depression secondary to SOOF descent and softens the nasolabial fold. Closure is as already described for preperiosteal lift.
ENDOSCOPIC MIDFACE LIFT
Use of the endoscope for midface lift is indicated or desirable in the following situations: (1) the patient is undergoing endoscopic brow lift and requires significant midface elevation; (2) the patient doesn’t require concomitant lower lid canthoplasty and its attendant scar; (3) the patient refuses any surgery that would leave a visible facial scar; or (4) the patient is undergoing midface elevation in conjunction with lower lid or full face CO2 laser resurfacing or both.
Important anatomical structures to consider are the frontal branch of the facial nerve and the infraorbital neurovascular bundle. The important planes include the dissection along the deep temporalis fascia and the subperiosteal midface dissection, as described above.
Surgical Technique
The surgical technique is divided into three major steps: (1) the endoscopic creation of a temporal pocket, (2) mobilization of the midface by subperiosteal dissection by either a gingival or a transconjunctival approach or both, and (3) elevation and suspension of the mobilized midface to the deep temporalis fascia and occasionally the arcus marginalis at the inferior orbital rim.
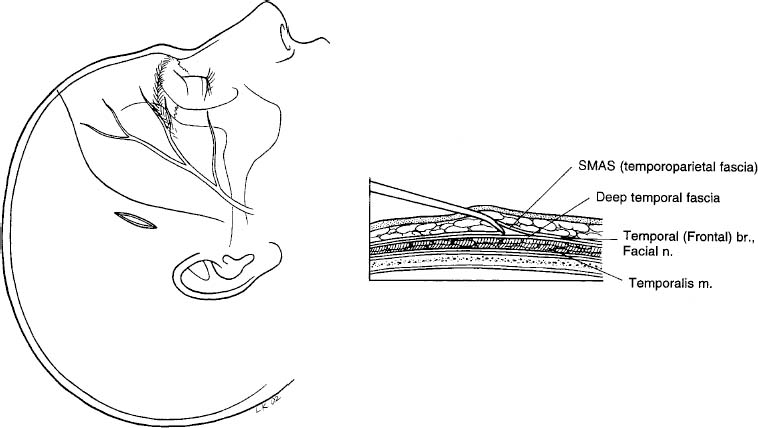
Creation of the temporal pocket begins by excising an ellipse from the temporal scalp and exposing the deep temporalis fascia. The incision is located ~ 1 cm posterior to the hairline in a line formed by the superior extent of the nasolabial fold and the lateral canthus (Fig. 7-8). A small incision in the deep temporalis fascia revealing underlying temporalis muscle verifies the proper plane. The temporal pocket dissection is started with an elevator under direct visualization along the deep temporalis fascia, which has a glistening white, immobile appearance. As the pocket is enlarged, the endoscope is introduced for visualization allowing the surgeon to avoid the temporal branch of the seventh nerve contained in the overlying temporal parietal fascia, which is an extension of the superficial musculoaponeurotic system (SMAS) found in the lower face (Fig. 7-9). Dissection is performed inferiorly and medially toward the lateral canthal region. The zygomatico-temporal “sentinel” vein is identified and cauterized if necessary. The inferior dissection extends to within ~ 1 cm of the zygomatic arch. Blunt dissection is performed in the lateral canthal region to enlarge the pocket, which provides a path for suspension sutures. The subperiosteal pocket dissection should not extend more laterally than the junction between the medial and middle one-third of the zygoma to avoid seventh nerve damage.
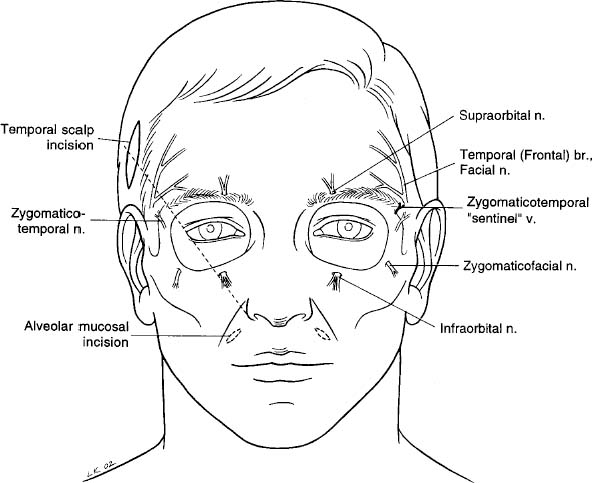
Mobilization of the midface is performed through a conjunctival or gingival incision or both. The transconjunctival incision may require a lateral canthotomy and cantholysis. The conjunctival incision is made 1 to 2 mm inferior to the inferior tarsal border down to just below the inferior orbital rim. The orbit is not entered unless the orbital fat is to be removed or redraped as part of a lower lid blepharoplasty. If used, the superior gingival sulcus incision is centered superiorly over the canine tooth, leaving a generous cuff of mucosa to allow for closure. The subperiosteal dissection is performed with a periosteal elevator. The infraorbital nerve is carefully identified and spared. The zygomaticofacial nerve is often sacrificed to allow full mobilization of the midface laterally and is usually of minimal clinical significance. The dissection is extended to the piriform aperture medially, the gingival sulcus inferiorly, and the anterior border of the masseter muscle laterally (Fig. 7-10). The endpoint is a well-mobilized midface.
The final step involves suspension of the mobilized midface to the deep temporalis fascia through the previously created temporal pocket. A 1-inch, 27-gauge guide needle is placed through the cheek at the point of desired elevation. In our experience, this is usually 5.0 to 5.5 cm from the midline at the level of the lateral alar portion of the nose (Fig. 7-11). Two 3-0 Monocryl (poliglecaprone 25) sutures (Ethicon, Inc., Somerville, NJ) are then placed in the periosteum medial and lateral to the guide needle. The guide needle is then removed. The Monocryl sutures are used to elevate the composite midface flap (the cheek). These sutures are pulled through the temporal pocket with a needle passer or long endoscopic needle holder (Karl Storz, Tuttlingen, Germany), crossed and secured to the deep temporalis fascia to create appropriate superior and lateral vectors of force (Fig. 7-12).
The temporal scalp incision is closed by securing the temporoparietal fascia (SMAS) from the anterior edge of the incision to the deep temporalis fascia posteriorly. The skin is closed with staples. The conjunctival incision is not closed unless a spacer graft is inserted, which is secured with 5-0 plain gut suture. The lateral canthus is closed in a standard fashion. The gingival incision, if used, is closed with a 4-0 chromic gut suture. A 4-0 polypropylene Frost suture is placed securing the lower lid to the upper lid and brow for upward traction in most cases (Fig. 7-13A,B
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree