Chapter 6
SURGERY OF THE LOWER EYELID
Robert A. Goldberg, Jonathan Wano Kim, Norman Shorr, Richard Tenzel, John L. Wobig, and Roger A. Dailey
BLEPHAROPLASTY
Several procedures are designed for lower lid surgery; this chapter will not cover the entire field. The anatomy of the lower eyelid has been previously covered, and the importance of the surgical anatomy for lower eyelid procedures cannot be overempha-sized. Remember, of the four rectus muscles, only the inferior rectus remains a composite muscle given that it not only rotates the globe downward but at the same time retracts the lower eyelid.
TRANSCUTANEOUS LOWER LID BLEPHAROPLASTY
The principal goal of lower eyelid blepharoplasty is to rejuvenate the appearance of the lower lids while preserving or improving their shape, position, and function. To accomplish this, the surgeon should critically evaluate the contour of the lower eyelid and midface region, realizing that the lower eyelid is a continuum from the inferior lid margin down to the cheek. In the past, the goal of blepharoplasty was simply to remove “excess” skin, muscle, and fat from the lower eyelid. Today, there are a variety of techniques that can be tailored to each patient to achieve a smooth youthful contour to the lower eyelid and midface region. The preoperative assessment should identify and separate the sources of concern, such as fat herniation, dermatochalasis, and fine rhytids. The surgical technique can then be individualized to improve the appearance in each of these areas, maximizing patient and surgeon satisfaction and avoiding complications.
Patients requesting lower eyelid blepharoplasty most commonly complain of lower lid fullness. Herniation of the lower orbital fat through an attenuated septum can produce these “bags” under the eyes, which are associated with a fatigued or tired look. For patients who possess isolated fat herniation, transconjunctival blepharoplasty is an excellent operation for diminishing fullness while maintaining lower eyelid position and contour. The preoperative evaluation should identify and localize areas of prominence due to fat herniation, which is most common in the medial two-thirds of the lower eyelid. It is also critical to evaluate the relationship of the lower eyelid to the midface region, including the position of the suborbicularis oculi fat (SOOF), the cheek fat pad, and the bony support of the maxilla. This will be discussed in Chapter 7 in association with midface surgical procedures.
Historically, two surgical approaches for lower eyelid blepharoplasty are available: the anterior transcutaneous approach and the posterior transconjunctival approach. In the traditional transcutaneous technique, excess skin, muscle, and orbital fat are removed through an infraciliary skin incision.
As with the upper eyelids (see Chapter 4), the CO2 laser is a helpful tool in lower lid blepharoplasty. The skin is incised with the superpulsed mode and subcutaneous dissection is performed in the continuous mode. The handpiece is defocused in this mode when hemostatis is necessary.
Surgical Technique
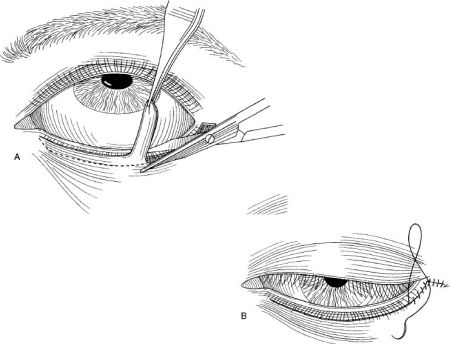
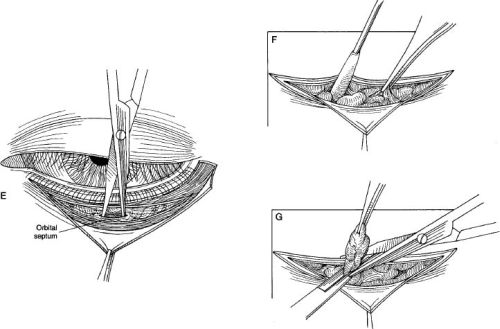
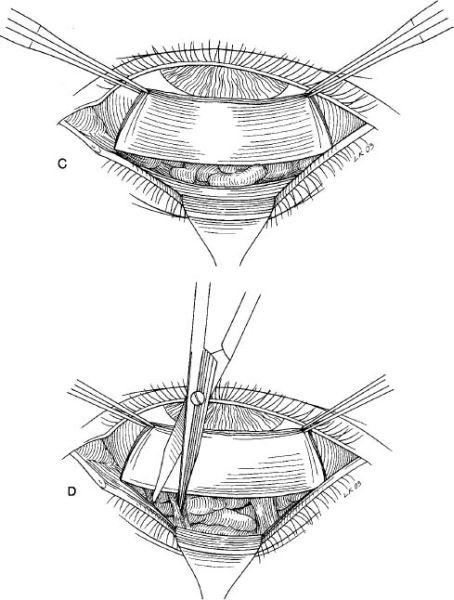
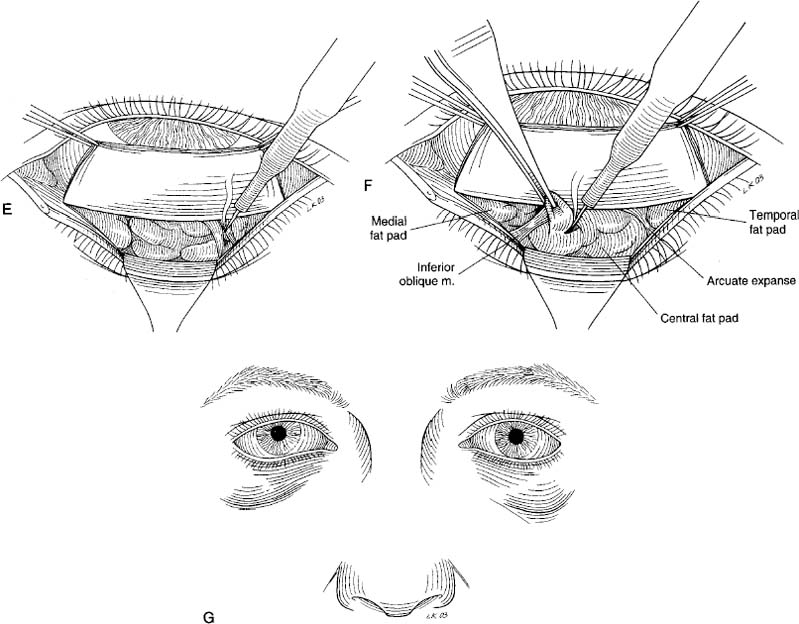
This procedure can be performed with the patient under oral, intravenous, or general anesthesia. A surgical marking pen is used to mark the incisions on the skin at this time, prior to distortion of the tissues by local infiltration. The transcutaneous incision should be 2 to 3 mm below the lash line. At the lateral commissure the mark extends out-ward, ending ~ 5 to 15 mm laterally following a lateral canthal rhytid whenever possible (Fig. 6-1A). Local infiltration consists of 1.5 to 2 mL of 2% lidocaine with epinephrine 1:100,000 with hyaluronidase (at least 5 units per mL), mixed 50:50 with 0.5% Marcaine. After approximately 10 minutes, the incision is made beneath the lower lid margin. The skin is dissected from the palpebral part of the orbicularis oculi muscle by blunt dissection with a Stevens scissors (Fig. 6-1B). Because the pretarsal orbicular muscle is the sole protractor in the lower eyelid, it should be preserved whenever possible. A useful technique is a “step-cut” procedure that employs an infralash incision but preserves the pretarsal orbicularis muscle. The surgeon should always remember that skin excision and dissection of a large myocutaneous flap carry an increased risk for postoperative lower eyelid retraction. If the skin is held “taut,” it is easier to follow the line of cleavage between it and the muscle by using Stevens scissors. The dissection is carried downward in a submuscular plane 10 mm or more. Reflect the skin downward and cut a small strip of preseptal muscle from lateral to medial (Fig. 6-1C). Pressure on the globe will push the orbital fat forward (Fig. 6-1D). Cut the capsule of the fat pad (Fig. 6-1E) and tease the fat from each capsule using a forceps and cotton-tipped applicator (Fig. 6-1F). Clamp the fat at its base with a hemostat, cut above the hemostat with a scissors, and cauterize with a thermal cautery (Fig. 6-1G).
As an alternative, the septum can be cut at the arcus marginalia and the fat teased out from underneath it and reduced or mobilized into an area of relative depression such as the lachrymal tear trough. The fat should be fixed in place with suture to the SOOF or through the skin, being careful not to restrict the septum inferiorly and potentially causing lid retraction.
There is no need to close the septum with either approach to the fat resection and it should be avoided. The amount of skin to be excised can be determined by laying the flap of skin over the lower eyelid margin (Fig. 6-2A). As the patient looks up, with the mouth wide open, the excess skin can be cut at the level of the original incision. Closure can be made with a running or interrupted suture (Fig. 6-2B).
PINCH SKIN EXCISION (ANTERIOR LAMELLAR EXCISION)
As already described, dermatochalasis of the lower eyelid can be treated by a transcutaneous approach, which involves dissection of a skin-muscle flap and violation of the orbital septum. Another alternative for patients with both dermatochalasis and fat herniation is orbital fat excision or repositioning via a transconjunctival approach (discussed following here) and removal of the excess lower eyelid skin by a “pinch” skin excision. This combined approach is a safer way to accomplish skin resection because the underlying orbicularis and orbital septum are left intact and the risk of postoperative eyelid malposition is markedly diminished.
For patients possessing large amounts of anterior lamellar redundancy, such as patients with orbicularis festoons, dissection of a skin-muscle flap may be necessary. Even in these patients, a large skin-muscle flap can be elevated and the redundant anterior lamella excised while keeping the orbital septum intact, the so-called SLAP (simultaneous lateral, anterior, and posterior) technique for lower eyelid blepharoplasty. Therefore, the skin-muscle flap should be suspended with a suture to the lateral canthal periosteum, and a horizontal tightening procedure is recommended if the patient possesses lower eyelid laxity. In many patients with orbicularis festoons, laser resurfacing combined with a transconjunctival blepharoplasty can lead to a significant improvement, obviating the need to perform transcutaneous surgery with dissection of a skin-muscle flap.
Surgical Technique
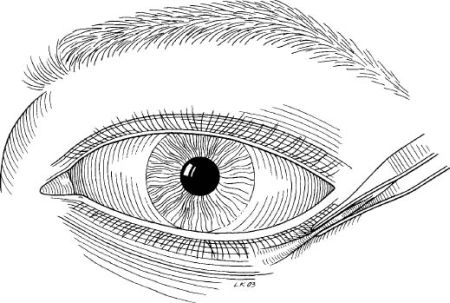
Following subcutaneous infiltration of the lower eyelid with local anesthetic (2% lidocaine with 1:100,000 epinephrine and Wydase), the lower eyelid skin is pinched 1 to 2 mm below the lashes at the lateral canthus with a small Brown-Adson forceps (Fig. 6-3). A ridge of skin is formed, extending medially and parallel to the lid margin. The appropriate amount of skin pinched is determined by the degree of dermatochalasis and the laxity of the lower eyelid. If the eyelashes are everted or the position of the lower eyelid is altered, pinching is repeated until no change results. Skin excision should always be conservative: younger patients rarely need skin removal and attempts to eradicate fine wrinkling in older patients will predispose to lower-eyelid retraction. The ridge of skin is excised with straight scissors, and care is used to remove only a minimal amount in the nasal angle to avoid webbing. If the patient has a hypertrophic orbicularis muscle, a small strip may be judiciously excised along the flap prior to skin closure. After complete hemostasis has been achieved, the skin is closed with a running 6-0 suture or with tissue glue (e.g., Histocryl).
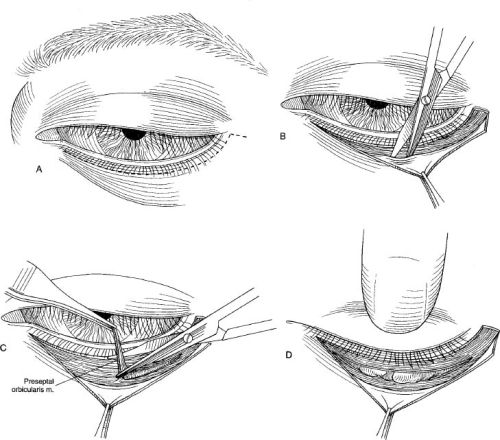
For patients that require dissection of a skin-muscle flap, an infralash incision is created below the lashes and parallel to the lid margin. Beyond the lateral canthus, the incision is continued straight laterally or within a preexisting laugh line. It is preferable that this lateral incision not be directed inferiorly because postoperative downward contracture can result in a conspicuous scar. A skin flap is elevated in the pretarsal area, preserving the pretarsal orbicularis. The Stevens scissors is used to tunnel a suborbicularis plane inferior to the tarsus, and the flap is converted into a skin-muscle flap by incising through the orbicularis along the horizontal length of the eyelid. Inferior dissection of the skin-muscle flap is performed while keeping the orbital septum intact (Fig. 6-4).
The skin-muscle flap is draped superiorly and laterally over the lid margin. The patient is asked to look up and open the mouth, mimicking the pull of gravity and placing the eyelid in its maximally extended position. The redundant skin above the lid margin with the patient’s mouth open may be excised. Removal of skin from below the lateral canthus is avoided. After removal of excess anterior lamella, the lateral edge of the excised orbicularis is pulled superotemporally and suspended with a 5-0 nonabsorbable suture to the periosteum at the lateral canthus.
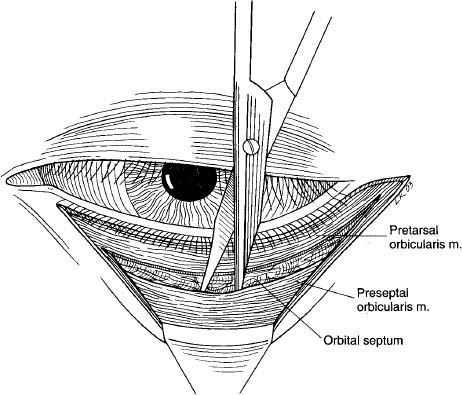
FIGURE 6-4 Create a skin-muscle flap preserving the septum.
TRANSCONJUNCTIVAL LOWER EYELID BLEPHAROPLASTY
The transconjunctival approach utilizes an incision through the conjunctiva beneath the tarsus, which permits rapid and direct entry into the orbital fat without disruption of the skin, orbicularis, or orbital septum.
Surgical Technique
Local anesthesia with intravenous sedation is re-commended for the vast majority of patients. Local injection is given through the conjunctiva because the sensory nerves of the conjunctiva and orbital fat originate in the orbit. First, a drop of topical proparacaine 0.5% is used to anesthetize the conjunctiva. Two percent lidocaine with epinephrine 1:100,000 and hyaluronidase (Wydase) is injected with a 27- or 30-gauge needle through the conjunctival fornix under direct visualization into each fat pocket. Gentle pressure is applied to the lids and a few minutes are allowed for hemostasis to occur while the surgeon scrubs and sterile preparation with open-face draping of the patient is performed.
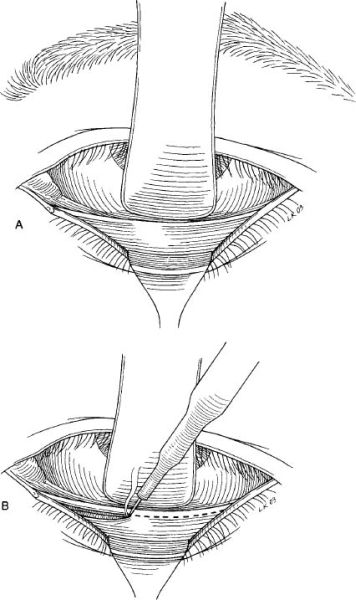
An assistant retracts the lower lid downward with a small Desmarres retractor to expose the cul-de-sac and to retract the skin away from the incision site (Fig. 6-5A
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree