ANATOMY OF THE LACRIMAL SYSTEM
John L. Wobig and Roger A. Dailey
The lacrimal fluid is (1) secreted and (2) distributed about the conjunctival sac, and (3) its excess is excreted into the nose. It therefore can be divided into a secretory system, a distributional system, and an excretory system.
THE LACRIMAL SECRETORY SYSTEM
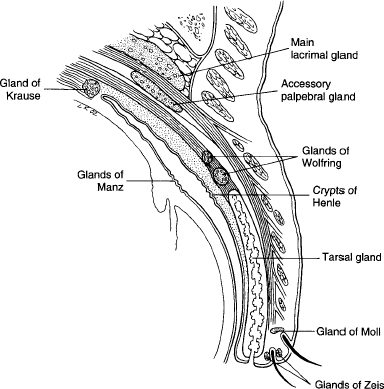
The secretory system consists of the basic secretors and the reflex secretors (Fig. 8-1).
BASIC SECRETORS
The basic secretors are glands that secrete the mucin, those that secrete lacrimal fluid, and those that secrete oil.
The mucin secretors consist of (1) the conjunctival mucin-secreting goblet cells; (2) the crypts of Henle found along the full length of the upper one-third of the conjunctival surface of the upper tarsus and, similarly, along the lower one-third of the lower tarsus; and (3) the glands of Manz, found in a circumcorneal ring of the limbal conjunctiva. The mucin secretors not only contribute most to the lubrication of the eyelids, they also form the inner or “fixed” polysaccharide layer of the precorneal film.
The lacrimal secretors are (1) accessory lacrimal glands of Krause, ~ 40 of which are in or about the upper conjunctival fornix and about six in the lower; (2) the accessory lacrimal glands of Wolfring, about three adjacent to the upper margin of the upper tarsus and one below the lower tarsus; and (3) an occasional gland in the plica and in the caruncle, and, sometimes, one may find an infraorbital gland. All of the lacrimal secretors are exocrine glands that lie in the subconjunctival tissue and form the intermediate fluid layer of the precorneal film.
The oil secretors are made up of (1) the tarsal (meibomian) glands, ~ 25 in the upper tarsus and 20 in the lower; (2) the glands of Zeis at the palpebral margin of each eyelid; and (3) the glands of Moll, found at the roots of the eyelashes. The oil secretors form the outer layer of the precorneal film, and the tarsal glands are the most important. The oily secretion prevents the escape of lacrimal fluid over the eyelid margins, and diminishes evaporation from the precorneal film.
Basic secretion is the fundamental, indispensable part of the secretory system. It alone can produce all three layers of the precorneal film. Every vertebrate that spends all or part of its life on land possesses this type of secretion, as well as the whale, which is completely aquatic. In many newborn creatures, it is the sole lacrimal supply for a few days or weeks. During sleep, it alone is present.
Many individuals go through life in fair ocular comfort with only basic lacrimal secretion. In the Schirmer No. 1 test, it accounts for the first 8 to 15 mm of wetting on the filter paper. There is no known efferent nerve supply to the basic secretors, but inflammation will increase mucin secretion. The amount of basic secretion decreases with age. It is always involved in hyposecretion but never in true hypersecretion.
REFLEX SECRETORS
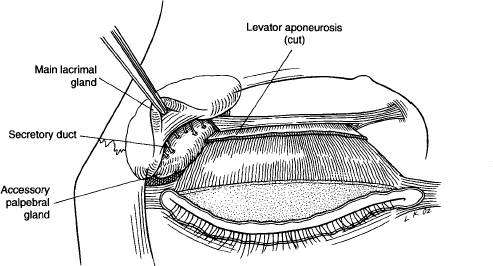
The reflex secretors include the main lacrimal gland (old terminology:orbital lobe) and the accessory palpebral gland (old terminology: palpebral lobe) (Figs. 8-2 and 8-3). They are also exocrine glands but differ from the glands of Krause and Wolfring in that they have an efferent, parasympathetic nerve supply.
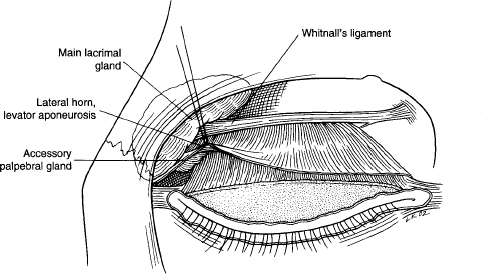
According to Whitnall, the main gland is ~ 20 x 12 x 15 mm in size and weighs ~ 0.78 g. Four sets of ligaments hold it firmly in place:
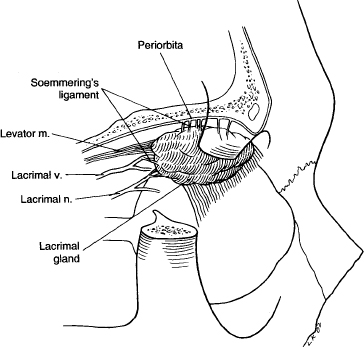
1. Superiorly and laterally by many bands of connective tissue of varying sizes, called Soemmering’s ligament (Fig. 8-4).
FIGURE 8-3 The accessory palpebral gland.
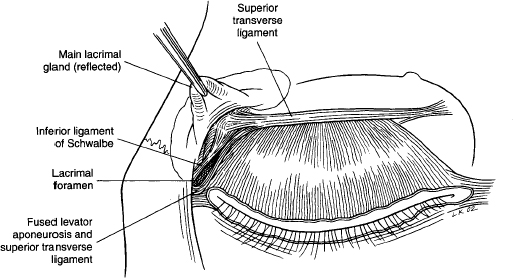
2. Posteriorly two or more bands of fascia that come from the subperiosteal tissue of the origins of the extraocular muscles and follow the lacrimal nerve and blood vessels to the gland. One of these bands, called the inferior ligament of Schwalbe, lies beneath the posterior part of the gland.
3. Medially, a broad ligament that is part of the superior transverse ligament, inferior to which is a band that extends to the vessels and excretory ducts at the hilus of the gland.
4. Anteriorly the upper free border of the lateral horn of the levator aponeurosis has fused with the superior transverse ligament. This is sometimes referred to as the lateral “check” ligament of the levator. The anterior margin of the inferior ligament of Schwalbe and the free margin of the levator aponeurosis form a fascial foramen: the lacrimal foramen (Fig. 8-5). Sometimes there is a slight shallowing of the frontal bone above the gland. This is referred to as the fossa of the lacrimal gland, but should not be confused with the lacrimal fossa.
Extending downward from the hilus of the main gland through the lacrimal foramen to the accessory palpebral gland are from two to six excretory ducts together with their blood vessels, lymphatics, and nerves. The ducts continue downward for a short distance in the postaponeurotic space and then pierce the posterior lamella of the levator (superior tarsal muscle) and conjunctiva to empty into the conjunctival sac ~ 5 mm above the convex lateral margin of the upper tarsus.
The accessory palpebral gland consists of 15 to 40 loosely knit lobules, each with a secretory duct that empties into a main excretory duct from the main gland. The upper lobules can usually be seen at the level of the lacrimal foramen and, occasionally, there will be an “isthmus” of glandular tissue connecting a few of the upper lobules with the main gland. The gland can be prolapsed into view by pulling the lateral canthal part of the upper eyelid laterally and upward.
Whitnall stated that, laterally, there may be one or two additional “main” excretory ducts that do not extend to the main gland. They drain only accessory palpebral gland lobules and may empty into the conjunctival sac as low as the lateral corner of the inferior fornix.
The fifth cranial nerve is the reflex, afferent pathway for the main and accessory palpebral glands. A flow of tears follows stimulation of its trunk or any of its branches (Czermak). “Blocking the sphenopalatine ganglion will stop the flow of (reflex) tears” (Ruskin). Other areas that may initiate a response are the retina, the frontal cerebral cortex, the basal ganglia, the thalamus, the hypothalamus, and the cervical sympathetic ganglia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree