SURGERY OF THE CANALICULI
John L. Wobig and Roger A. Dailey
Epiphora frequently disqualifies the affected persons for employment in public positions or for enlistment in the armed forces. Industry considers that the disease makes driving hazardous and poses a risk in any job that requires constant clear vision. Epiphora patients are seldom able to wear contact lenses, and eyeglasses add to the epiphora patient’s handicap. For these and other reasons, epiphora sufferers anxiously seek relief.
The ophthalmologist who is not particularly interested in lacrimal problems, or not familiar with such diagnostic methods as the dye tests, either ignores these patients or subjects them to long, painful, and futile probings and irrigations. Overdilations with larger probes, especially those that cause bleeding, only augment the constriction. Some methods completely destroy a useful canaliculus.
DIAGNOSIS AND TREATMENT
Epiphora due to hypersecretion can be ruled out only by doing a primary dye test, as described in Chapter 10. Complete obstructions can be diagnosed by irrigations and probings and partial obstructions by the primary and secondary dye tests. Epiphora due to allergies and inflammations should have appropriate treatment. Epiphora caused by either foreign bodies or tumor will be discussed later in this chapter.
CANALICULITIS
Canaliculitis is always associated to varying degrees with acute conjunctivitis and to lesser degrees with chronic infections. Drugs used in the treatment of conjunctivitis and glaucoma, for example, Floropryl and Pilocar, may lead to obliteration of the canali culi. Actinomyces infections are largely confined to the canaliculi. The incidence of canalicular problems is high in trachomatous patients. Other viral infections and involutional changes may eventually obliterate the lumen of a duct.
It is possible to cure an everted lower punctum by wiping it “up-and-in” instead of “down-and-out.” Hypertrophic epithelium protruding from a punctum may be cauterized with silver nitrate (solution 5-10%) or some other astringent drug.
INDICATIONS FOR SURGERY
Surgery is indicated in the following cases in which canalicular failure has caused disturbing epiphora and conservative treatment has failed:
1. Phimosis of the puncta
2. Patent puncta in lacrimal hyposecretors
3. Eversion of the puncta
4. Deep lacus lacrimali with suspended puncta
5. Foreign bodies and neoplasms of the canaliculi
6. Trauma of the canaliculi
7. Idiopathic canalicular obliteration
8. Cases with patent ducts in which both the primary and secondary dye tests are negative
PHIMOSIS OF THE PUNCTA
Technically, probing a punctum is contraindicated unless both the primary and the secondary dye tests are negative. The patient with epiphora due to hypersecretion would have a positive dye test. Often one punctum is closed but the other is open and functioning.
Occasionally, a patient is born without a punctum. One can often make a stab incision with a sharp hypodermic needle or a pointed Bard-Parker blade in the area in which the punctum should be. The punctum is usually 1 to 2 mm medial to the most medial orifice of the meibomian glands.
The punctum dilator should have a tapered tip and a shaft no larger than a No. 1 or No. 2 Bowman probe. Dilators with a continuing enlargement of the shaft, such as the Ziegler punctum dilator, will tear the punctum if too much force is used.
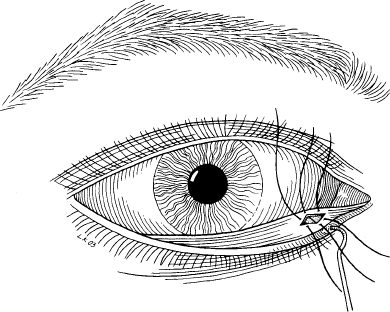
If, after three or four dilations, the phimosis recurs, a “one-snip” procedure should be used. The punctum is dilated enough to admit a No. 1 or No. 2 Bowman probe. Cocaine hydrochloride (5%) with adrenalin (1:1,000) on a cotton-tipped applicator is applied to the punctum for 2 minutes. One blade of an iris scissors is inserted to the floor of the ampulla with the other blade on the conjunctival side of the eyelid. If the scissors are closed quickly, the patient will have little or no discomfort (Fig. 12-1A).
If the punctum has a tendency to close, it should be dilated with a Ziegler punctum dilator two or three times at 2-day intervals. When the one-snip procedure fails, the two-snip method is used. The vertical snip is repeated and a second horizontal snip is made 2 or 3 mm long at the base of the vertical snip at the level of the floor of the ampulla (Fig. 12-1B). The advantage of the two-snip technique over the conventional three-snip procedure is that it leaves a triangular flap that maintains much of the function of the ampulla. The three-snip procedure removes a triangle of punctal tissue and is not recommended.
PATENT PUNCTA IN LACRIMAL HYPOSECRETORS
When the Schirmer No. 1 test repeatedly shows < 5 mm of wetting, the Schirmer No. 2 test shows < 10 mm, and the primary dye test is positive, the patient is always uncomfortable. Closing both puncta by electrocauterization or collagen plugs may be of great benefit (see Chapter 10). This will prevent artificial tears and medication from escaping from the conjunctival sac.
The first cauterization should just barely close the puncta so that they will reopen in a few weeks. If the patient gets definite relief from the closure, one can then close the ducts permanently. When the primary dye test is negative, the ducts do not need to be cauterized.
EVERSION OF THE PUNCTA
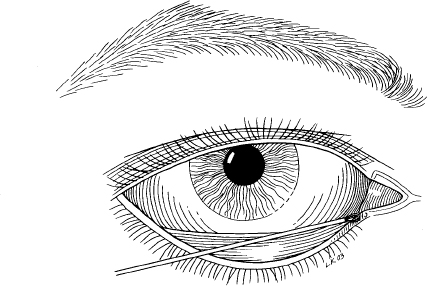
In patients in whom only the lower punctum is everted, one should remove a diamond-shaped piece of conjunctiva and subconjunctival fascia (Fig. 12-2). The part resected should measure ~ 5 mm in width and 10 mm in length. Resection should begin ~ 4 mm inferior to the punctum and the cut should be extended both ways, keeping the long axis horizontal. Insertion of a lacrimal probe in the lower duct while operating will protect the canaliculus. One must be careful not to injure the ampulla, which lies along the anterior medial margin of the dissection, nor to remove any of the deep head of the inferior pretarsal muscle with the conjunctiva. Three interrupted sutures (Vicryl 6-0) draw the anterior and posterior margins of the wound together.
If the eversion of the lower punctum is more extensive or if both puncta are involved, it is advisable to perform the Lee operation. Essentially, this technique consists of making an intermarginal adhesion between the entire lacrimal part of the eyelid margins.
If the punctum is absent and cannot be found by a vertical stab incision in the papilla lacrimalis, the anterior margin of the tear sac can be opened and a Bowman lacrimal probe passed back through the canaliculus to the punctal region. In this way, one can slit the punctum or the canaliculus along the conjunctival side of the eyelid with much less trauma and the functional results will be better than with an unguided exploratory search. In a high percentage of such patients no canaliculus will be found.
DEEP LACUS LACRIMALS WITH SUSPENDED PUNCTA
Occasionally, in patients with a deep lacus and a wide palpebral fissure, both puncta will be suspended anterior to the marginal tear strip and lacus, and the tears will spill out over the commissure. Such cases are usually bilateral and the primary dye test is negative. One patient was cured by a conjunctivodacryocystorhinostomy, with insertion of a Pyrex tube. It is probable that intermarginal closure of the lacrimal part of the eyelid margins would restore the puncta to the marginal tear strip; however, the cosmetic result might be less satisfactory.
FOREIGN BODIES AND NEOPLASMS OF THE CANALICULI
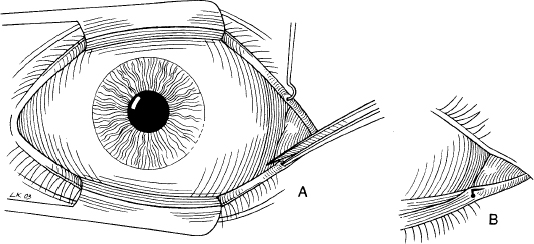
When foreign bodies are present, such as in Streptothrix infections, one or both canaliculi on one side usually become so dilated that the concretions may be removed with a tiny ear curette or be “milked” out with a glass rod by stroking the canaliculus from the commissure toward the punctum (Fig. 12-3). When no more granules appear, the canaliculus should be irrigated with normal saline or an antifungal solution. The treatment should be repeated at weekly intervals until there is no sign of more granules or infection. Both canaliculi should be examined and the common canaliculus probed if the fluid does not flush freely into the nose. Occasionally, a Streptothrix granule will plug the common canaliculus, but if dislodged, will usually wash through into the nose or remain in the tear sac. When the foreign body is not friable, the canaliculus should be opened along the lacrimal part of the eyelid margin, sparing the punctum by beginning the incision ~ 3 mm medial to the punctum and extending it as far medially as necessary (Fig. 12-4). The margins should be held open by two or more traction sutures (silk 6-0). The incision can be closed by a continuous suture through the skin alone.
This is also the method of choice when neoplasms are present or when the base of a protruding polyp is medial to the punctum. In such a case the base can be destroyed by cautery. In malignancies, the canaliculus can seldom be salvaged.
FIGURE 12-3 Removal of the foreign body from the canaliculus with a small-ring ear curette.
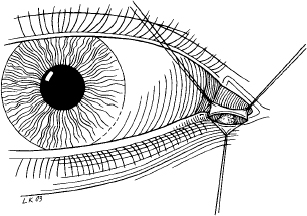
FIGURE 12-4 Opening the canaliculus sparing the punctum.
TRAUMA OF THE CANALICULI
In many hospitals, severed canaliculi are repaired in emergency surgery. This can be performed where the trauma is minimal. Deeper injuries at or in the tear sac with extensive trauma and bleeding should not be repaired for 12 or more hours, and only after thorough evaluation. It takes several hours to complete such surgery, necessitating using the operating microscope and special instruments and fine sutures. In some patients a dacryocystorhinostomy also will have to be performed. Certainly no surgeon without a thorough knowledge of the anatomy of this area should attempt to repair such injuries without skilled assistance.
A dye test should always be performed at the time of an injury that does not involve both canaliculi. If the test is positive, or if probing or irrigation proves that one of the passages is intact, one should inform the patient of the following:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree