Chapter 5
SURGERY OF PTOSIS (INCLUDING SURGERY OF PTOSIS BY FRONTALIS SUSPENSION)
Allen M. Putterman, Steven C. Dresner, Dale R. Meyer, John L. Wobig, and Roger A. Dailey
There is a difference of opinion on the proper surgical repair for ptosis. The authors’ preference for levator resection or aponeurosis repair is based on an anatomical approach. Alternative methods are discussed here so the reader can select a method that is suitable.
The conjunctival approach for levator resection was the most popular method in the past. It is now utilized most frequently in tarso-Müller’s muscle-ectomy. Caution is advised in the approach for anatomical reasons. The conjunctiva in the area used is rich in mucin-secreting goblet cells and contains 80% of the accessory lacrimal glands of Krause and Wolfring. The ducts from the reflex-secreting lacrimal glands are adjacent at the lateral end of the incision and may sever them. The conjunctival approach should be avoided in patients with traumatic ptosis, ptosis due to aponeurotic defects, and reoperations.
The cutaneous approach is important for all ptosis surgeons to know because it is a necessary approach for ptosis with reduced levator function and ptosis with greater severity. This approach will not sacrifice conjunctiva, tarsus, and the lacrimal glands. It is the accepted approach for complicated surgery, especially for traumatized eyelids and reoperations for ptosis. Greater amounts of resections are possible in cases where the levator action is poor. Finally, it gives the opportunity to remove redundant skin. The approach should always be based on what is best for the patient.
LEVATOR APONEUROSIS REPAIR
The levator aponeurosis repair was reintroduced and promoted by L.T. Jones and has been the authors’ primary procedure for acquired myogenic ptosis. This procedure allows simultaneous repair of the ptosis with blepharoplasty. The procedure lends itself to local anesthesia and anatomical defects and leaves the conjunctival surface intact. This procedure provides better corneal protection and less patient discomfort. Postoperative modification is the easiest with this ptosis repair.
SURGICAL TECHNIQUE
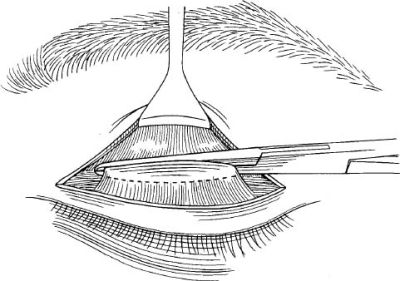
The patient is placed in the supine position and usually is given a local anesthetic. A skin marker is used to make a mark in the eyelid furrow (Fig. 5-1). If it is a unilateral ptosis, it should correspond to the furrow of the opposite eyelid. If the ptosis is bilateral, the marks made in the furrow must be symmetrical. An incision is made along the marked furrow no deeper than the subcutaneous tissue. Blunt dissection with the Stevens scissors separates the skin from the pretarsal muscle a few millimeters on each side of the incision. A small strip of preseptal muscle is removed along the incision just above the superior border of the tarsus (Fig. 5-2). This usually exposes the underlying septum.
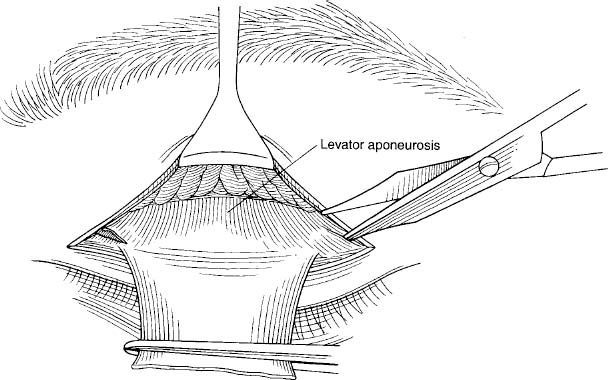
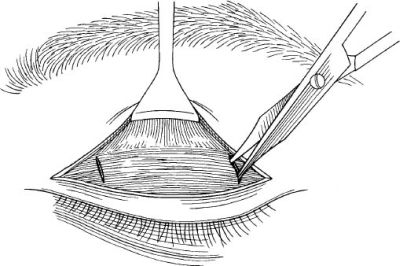
A tightly wound cotton-tipped, short, wooden applicator held in one hand and moved backward and upward while pulling the lid margin inferior with the opposite hand usually exposes the aponeurosis. If this does not work, the fat pad can be seen through the septum with mild pressure on the globe. Buttonhole the septum and cut it medially and laterally (Fig. 5-3). Grasp the preaponeurotic fat and pull it superior while separating it from the underlying levator.
The pretarsal muscle is now undermined over the anterosuperior border of the tarsus (Fig. 5-4). A small cut can now be made in the aponeurosis near the superior border of the tarsus, exposing the tarsus and Müller’s muscle (Fig. 5-5).
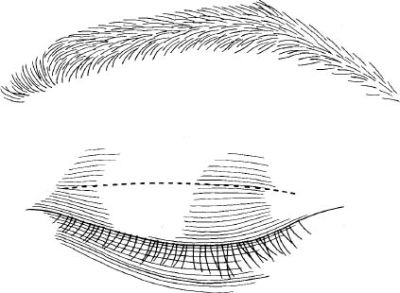
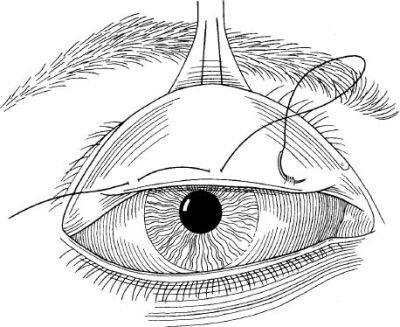
FIGURE 5-1 Marking the skin in the eyelid furrow.
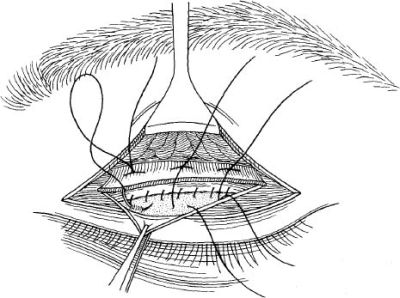
A Dacron suture (5-0) is placed horizontally through the aponeurosis above (Figs. 5-6 and 5-7). To determine where the suture is placed inferiorly in the anterosuperior border of the tarsus, grasp the superior border of tarsus and pull it superior. The spot at which it lifts the lid with its normal curvature is where the needle is placed horizontally through the anterior surface of the tarsus. This maneuver usually prevents any peaking. The suture is tied with the first part of a surgeon’s knot, leaving the trailing end of the suture below the knot so it can be untied easily, like a shoelace bow.
The patient is asked to look up with both eyelids to determine the amount of correction. If the correction is not right, untie and change the suture through the aponeurosis. Usually overcorrect by ~ 2 mm to account for the anesthesia that affects the antagonist muscle and stimulates Müller’s muscle.
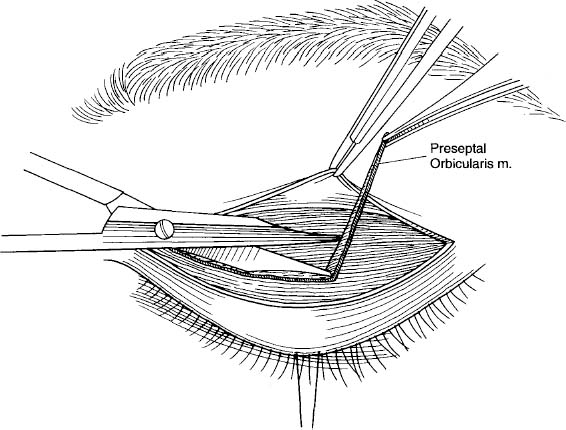
FIGURE 5-3 Buttonhole the septum and cut it medially and laterally.
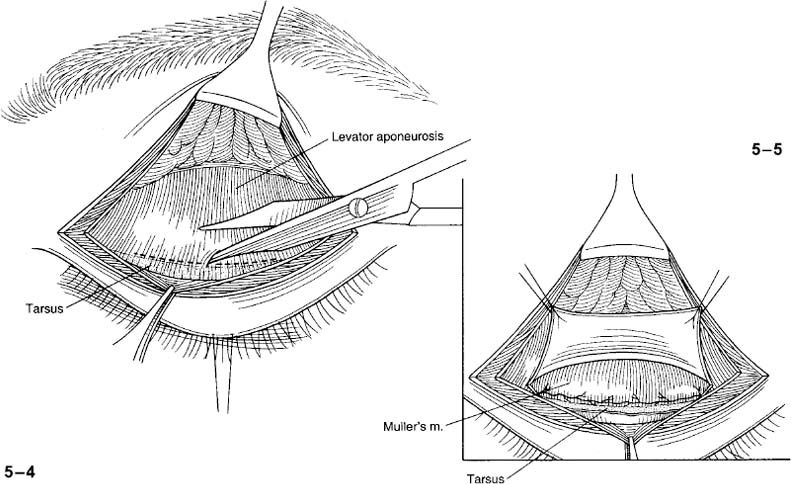
FIGURE 5-4 Undermine the pretarsal muscle over the anterosuperior border of the tarsus.
FIGURE 5-5 Make a small cut in the aponeurosis to expose the tarsus and Müller’s muscle.
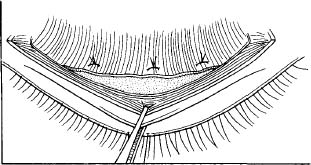
FIGURE 5-7 One, two, or three sutures may be needed.
The skin is closed with 6-0 nylon or fast-absorbing 5-0 chromic in a running fashion. Ointment is placed over the incision; a dressing is optional. If the correction is over- or undercorrected an adjustment can be made up to 7 days postoperative. Under local anesthesia without adrenalin the skin sutures are removed and the wound is pulled open with two forceps to expose the aponeurosis. The correction is made by resuturing for the correct response.
LEVATOR RESECTION
This procedure can be used for the majority of ptosis cases. It is used primarily for ptosis when it is congenital and severe. This procedure requires knowledge of eyelid anatomy from skin to conjunctiva.
SURGICAL TECHNIQUE
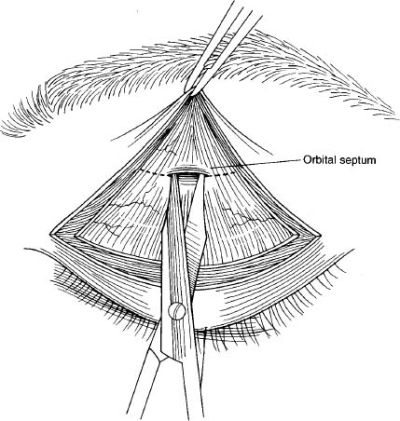
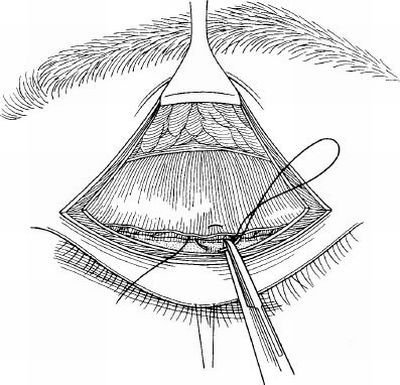
Anesthesia is general for pediatric cases and can be either local with sedation or general for adults. The patient is placed in the supine position. A skin incision is made to correspond to the upper eyelid crease (see Fig. 5-1). The skin and preseptal muscle are undermined above the crease for 5 to 6 mm (Fig. 5-8). Two incisions are then made with scissors full thickness through the lid from muscle to conjunctiva at each end of the crease incision (Fig. 5-9). A straight hemostat is then placed with the deep blade in the fornix and is adjacent to the conjunctiva at the upper border of the tarsus (Fig. 5-10). The hemostat has between its blades the conjunctiva, Müller’s muscle, levator aponeurosis, and some preseptal muscle fibers. No skin is included. Divide the attachments inferior to the lower border of the hemostat (Fig. 5-11). The hemostat is elevated superior, and after undermining the conjunctiva it is incised and returned to its anatomic position. Suture the conjunctiva with 6-0 or 7-0 plain chromic suture to the upper border of the tarsus (Fig. 5-12). Rotate the hemostat inferior and locate the orbital septum. The orbital septum is separated from the levator and allowed to retract (Fig. 5-13). The preaponeurotic fat and levator are now identified. Traction on the hemostat puts tension on the medial and lateral horns of the aponeurosis (Fig. 5-14). They can be severed medially and laterally. The levator can then be resected up to 30 mm. Sutures are chosen if the surgeon prefers absorbable or nonabsorbable suture. Examples are 5-0 Dacron or 5-0 Vicryl. Three double-armed sutures are placed in the muscle at the desired height (Fig. 5-15). The excess levator is excised. The three sutures are fixed to the anterosuperior border of the tarsus (Fig. 5-16). The sutures are tied. The contour of the lid margin can be adjusted by changing position of any of the three sutures. The skin is closed with crease enhancement sutures by including a bite in the levator.
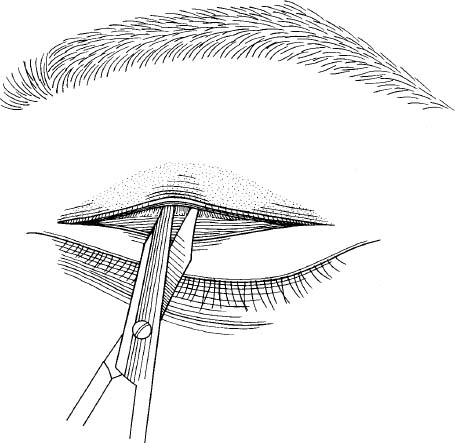
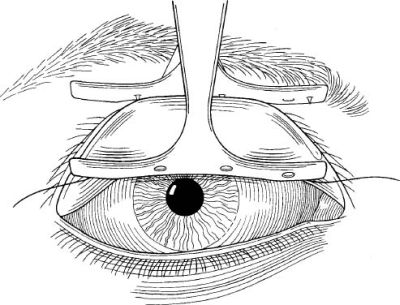
FIGURE 5-8 Undermine the skin and preseptal muscle above the crease for 5 to 6 mm.
Postoperative care of levator resection involves protecting the cornea. Lubrications are used to protect corneal abrasion, and overcorrection of acquired ptosis repair should include massage and stretching of the eyelid. In congenital ptosis, observation may be all that is necessary because the eyelids tend to fall during the first weeks or month.
MÜLLERECTOMY
In 1975, Putterman and Urist described a technique in which Müller’s muscle is partially resected and advanced. The Müller’s muscle-conjunctival resection ptosis procedure is recommended for patients with blepharoptosis whose upper eyelids elevate to a normal level when 10% phenylephrine drops are applied to their upper ocular fornix. Candidates usually have minimal congenital ptosis and varying degrees of acquired ptosis.
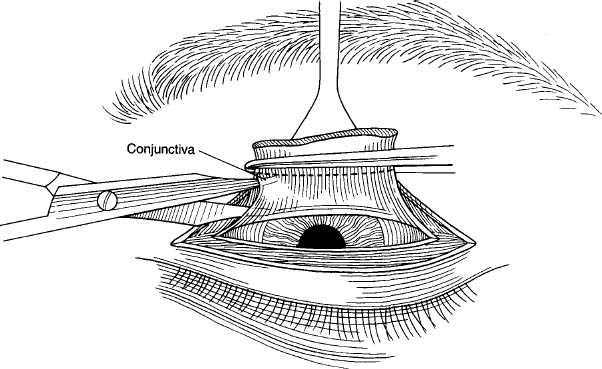
FIGURE 5-11 Divide the attachments inferior to the lower border of the hemostat.
SURGICAL TECHNIQUE
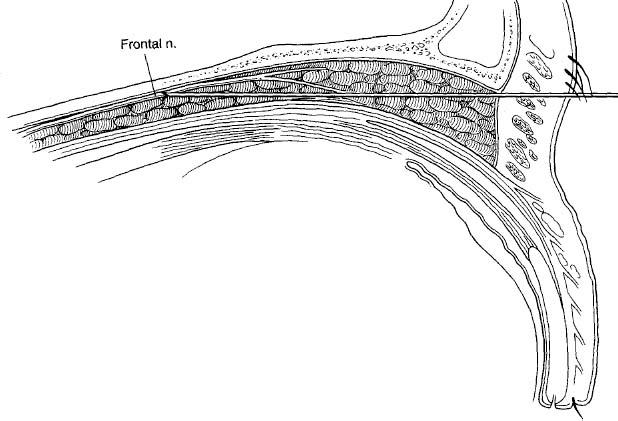
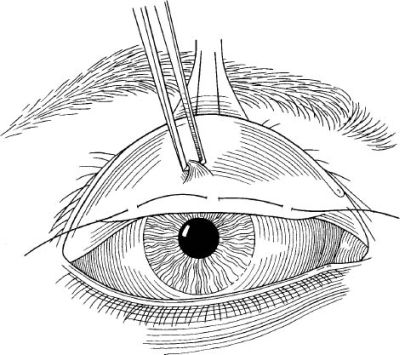
General anesthesia is used in children; local anesthesia is preferred in adults. A frontal nerve block is used with local anesthesia to avoid swelling of the upper eyelid by local infiltration, which would make the operation more difficult and inexact. A 23-gauge retrobulbar type needle is inserted into the superior orbit, entering just under the midsuperior orbital rim (Fig. 5-17). The needle hugs the roof of the orbit during insertion until a depth of 4 cm is reached, then 1.5 mL of 2% lidocaine with epinephrine is injected subcutaneously over the central upper eyelid just above the eyelid margin. A 4-0 black silk traction suture is inserted through skin, orbicularis muscle, and superficial tarsus 2 mm above the lashes at the center of the upper eyelid. A large Desmarres retractor everts the upper eyelid and exposes the palpebral conjunctiva (Fig. 5-18). A caliper set at 8 mm, with one arm at the superior tarsal border, facilitates insertion of a 6-0 black silk suture through the conjunctiva 8 mm above the superior tarsal border. One bite centrally and two others, ~ 7 mm nasal and temporal to the center, mark the site. The suture is usually placed 8 mm above the superior tarsal border, but may be placed 6.25 mm to 9.75 mm above it if the response of the upper eyelid level to the phenylephrine test is slightly more or less than desired.
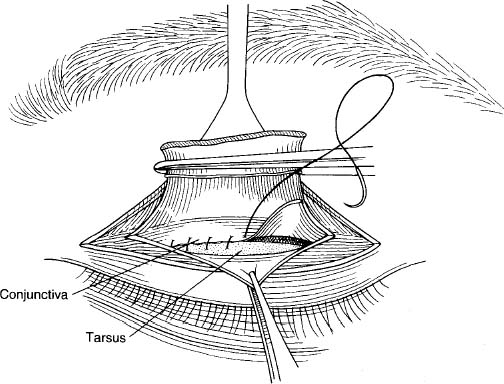
FIGURE 5-12 Suture the conjunctiva to the upper border of the tarsus.
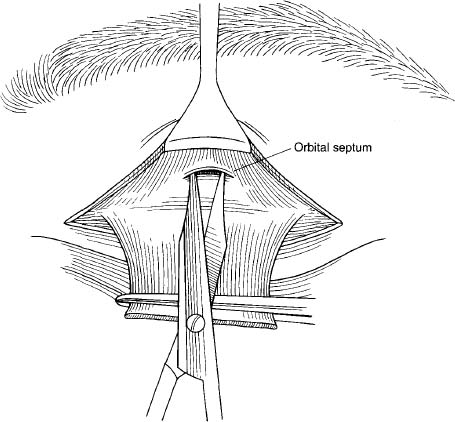
FIGURE 5-13 Separation of the orbital septum from the levator.
A toothed forceps grasps conjunctiva and Müller’s muscle between the superior tarsal border and marking suture and separates Müller’s muscle from its loose attachment to the levator aponeurosis (Fig. 5-19) (this maneuver is possible because Müller’s muscle is firmly attached to conjunctiva but only loosely attached to the levator aponeurosis). We place one blade of a specially designed clamp at the level of the marking suture. Each tooth of this blade engages each suture bite that passes through the palpebral conjunctiva (Fig. 5-20). The Desmarres retractor is then slowly released as the other blade of the clamp engages conjunctiva and Müller’s muscle adjacent to the superior tarsal border (Fig. 5-21). Any entrapped tarsus is pulled out of the clamp by the surgeon’s finger. The clamp is compressed and the handle locked. This leads to the incorporation of conjunctival and Müller’s muscle between the superior tarsal border and the marking suture. The upper eyelid skin is then pulled in one direction while the clamp is pulled simultaneously in the opposite direction (Fig. 5-22). If the surgeon feels a sense of attachment between the skin and clamp during the maneuver, this means that the levator aponeurosis has been inadvertently trapped in the clamp. If this occurs, the clamp should be released and reapplied in its proper position (this maneuver is possible because the levator aponeurosis sends extension to the orbicularis muscle and skin to form the lid crease).
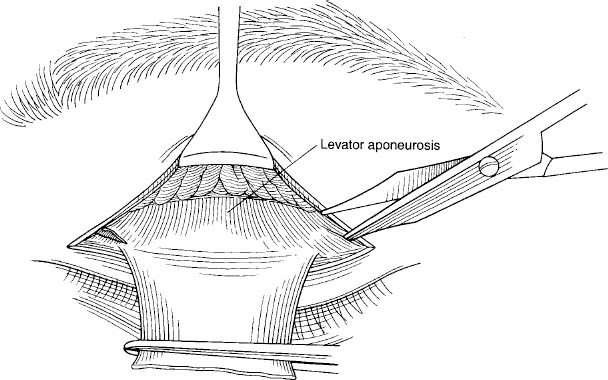
FIGURE 5-15 Placement of three double-armed sutures at the desired height.
FIGURE 5-16 Fixture of three sutures to the anterosuperior border of the tarsus.
With the clamp held straight up, a 5-0 double-armed, plain catgut mattress suture is run 1.5 mm below the clamp along its entire width in a temporal to nasal direction, through the upper margin of the tarsus and through Müller’s muscle and conjunctiva on the other side, and vice versa (Figs. 5-23 and 5-24). The sutures are placed ~ 2 to 3 mm from each other. A Number 15 surgical blade is used to excise the tissues held in the clamp by cutting between the sutures and the clamp. The knife blade is rotated slightly with its sharp edge hugging the clamp. As the tissues are sliced from the clamp, the surgeon and assistant watch to ensure that the stitches on each side are not cut.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree