Effects of Anterior Cruciate Ligament Reconstruction on In Vivo, Dynamic Knee Function
Keywords
• Anterior cruciate ligament • In vivo knee kinematics • Dynamic stereo X-ray system • Knee • Anatomic • Double-bundle • Single-bundle
Key Points
Introduction
The goals of anterior cruciate ligament (ACL) reconstruction are to restore stability and enable return to unrestricted function during the short term and ideally to protect joint health during the long term. Current treatment approaches are moderately successful for restoring function, with most individuals able to return to their preinjury level of sports activity.1,2 However, surgical ligament reconstruction does not seem to prevent the development of osteoarthritis after ACL injury.3–5 Although there are many factors that may contribute to joint degeneration, persistent abnormal knee mechanics are often implicated in the initiation and progression of osteoarthritis (OA) in the ACL-injured/reconstructed knee.6,7 Concerns about the high rates of OA are largely responsible for the increased interest during the last several years on more anatomic approaches to ACL repair and reconstruction. Although no current techniques can restore the true insertion site anatomy or physiology of the native ACL, procedures that attempt to improve tunnel placement and graft geometry to more closely resemble the original ligament are gaining in popularity. The premise for these newer procedures is that better restoration of native anatomy will lead to more normalized joint mechanics and improved long-term joint health.
Methodologic considerations for assessing knee function
Laxity Versus Stability
In vivo knee function can be evaluated under a wide range of conditions. Which measures are most relevant to outcomes after ACL reconstruction? With the progression from laxity testing to static weight-bearing to dynamic, functional activities, assessment becomes more technically demanding but also potentially more relevant to joint health. Central to most theories relating joint mechanics to OA development is the idea that altered joint contact patterns and joint loads, encountered during routine activities, can be detrimental to long-term cartilage health.6,8 These theories would suggest that the most relevant measures of joint function are those that reflect the behavior of the knee during common, functional activities. It is especially important to distinguish between evaluations of laxity versus assessments of dynamic knee function and functional stability. In a recent review, Musahl and colleagues9 stated, “In biomechanical terms, laxity is the passive response of a joint to an externally applied force or torque. Stability, on the other hand, is a functional measure; that is, a knee, regardless of laxity, is only unstable if it ‘gives way’ during functional activities.” Laxity tests are typically performed without the compressive joint forces required to properly engage the conforming condylar surfaces, which play an important role in joint stabilization. Thus, although laxity tests may be effective for identifying structural deficits, the results cannot predict joint behavior during dynamic, functional activities. In fact, many studies relating static laxity and clinical/functional outcomes have reported correlations that are at best weak.10–14
Knee Function Is Task Dependent
In vivo studies incorporating body-weight loading and active muscular control provide a much more comprehensive and realistic picture of the natural function of the knee joint as a complex neuromusculoskeletal system. However, the knee has a wide envelope of possible motions, and joint function is highly activity dependent. Patterns of joint motion and articular contact vary considerably with loading and activity, even during similar ranges of knee flexion.15,16 Knee tissues are highly viscoelastic and respond nonlinearly to load magnitude and loading rate,17,18 so the behavior of the knee under low-demand conditions cannot be simply “scaled up” to predict behavior during functional activities. Thus, studies incorporating body-weight loading during quasi-static activities (eg, sequential fixed knee angles19) or low-effort movements (eg, half-speed gait20) may not predict knee behavior during more complex, demanding tasks. This may be especially important for ACL-injured athletes, who will routinely expose their joints to high-magnitude, rapidly changing loads after returning to sports.
Measurement Options for Dynamic, In Vivo Studies
Meaningful characterization of dynamic joint function during common activities poses unique challenges, especially for measurements directly relevant to soft tissue behavior. Peak ACL strains during activities of daily living are on the order of 4% or less21; for a typical ACL size, this represents a length change of only 1.2 mm. Assessing articular contact kinematics (arthrokinematics) requires a measurement error substantially smaller than the thickness of the cartilage layer (typically 2–4 mm thick for the tibiofemoral joint). The most widely used technology for studying knee function after ACL reconstruction is video-motion analysis, which tracks motion of multiple skin-mounted markers placed on the thigh and shank to determine limb movement. This technology is noninvasive, widely available, and reliable and has been effective for identifying differences in knee kinematics between ACL-intact, ACL-deficient, and ACL-reconstructed joints (as described later). But, conventional motion analysis cannot achieve the submillimeter accuracy required for tissue-relevant measurements, because of the displacement of skin-mounted markers relative to underlying bone.22–24 Magnetic resonance (MR) imaging can achieve submillimeter accuracy and enables direct visualization of soft tissue, but sample rates are too slow and the imaging environment is too restrictive for most functional movement tasks.
Dynamic radiographic imaging enables direct visualization and 3-dimensional tracking of bone motion and has been gaining in popularity during the past decade. Although some measurements have been performed using a single imaging plane, dual or biplane imaging systems are generally required to obtain submillimeter resolution in all 3 movement planes. Many systems are now in use across the United States, with capabilities that vary based on the specific equipment and analysis techniques used. Conventional “C-arm” fluoroscopy systems are limited by low frame rates (≤30 Hz) and long exposure times (≥8 ms) but are adequate for quasi-static and low-speed activities.25,26 Custom-built systems can achieve much higher sample rates and have validated submillimeter accuracy for more physically demanding tasks, such as running.27–29
Dynamic knee function: traditional ACL reconstruction
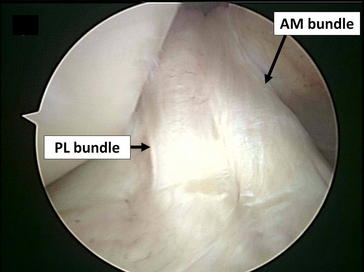
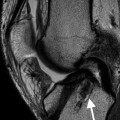
The ACL is often described as consisting of 2 functional bundles, the anteromedial (AM) and the posterolateral (PL) bundles, named in relation to their typical orientation and insertion on the tibia and femur (Fig. 1).30,31 The AM and PL bundles function synergistically to provide both anterior and rotational stability of the knee. Cadaver studies suggest that the AM bundle is taut throughout the range of motion of the knee, reaching a maximum tension between 45° and 60°, whereas the PL bundle is tight primarily in extension.32–35
Traditional ACL reconstruction procedures have been performed using a single graft bundle, without attempting to recreate the native double-bundle ACL anatomy. The tunnel placement techniques commonly used (eg, transtibial drilling of the femoral tunnels and/or the “o’clock” method for drill orientation) also failed to reliably place the graft within the native ACL footprint.36,37 These single-bundle, nonanatomic procedures may eliminate anteroposterior (AP) laxity and successfully restore normal AP translation but fail to restore rotational stability.38,39 Numerous in vivo kinematic studies using a variety of loading conditions have confirmed that these procedures fail to restore normal dynamic knee function. Logan and colleagues,40 using open-access MR imaging, reported that ACL reconstruction reduced sagittal laxity to within normal limits but did not restore normal tibiofemoral kinematics during static weight-bearing. Georgoulis and colleagues41 examined ACL-deficient individuals before and after bone–patellar tendon–bone ACL reconstruction during walking using video-motion analysis. The ACL-deficient patients demonstrated greater tibial internal rotation, which decreased closer to normal levels after ACL reconstruction. In a subsequent investigation with higher-demand activities (stair descent and pivoting), tibial rotation was significantly larger in the ACL reconstructed knees compared with the contralateral, intact legs.42 Kinematics after ACL reconstruction have also been investigated using radiographic techniques to analyze in vivo knee kinematics without errors from skin motion artifacts. Brandsson and colleagues43 found that tibial rotation and AP translation were not restored by ACL reconstruction (using bone–patella tendon–bone autografts) in 9 unilateral ACL patients 1 year after surgery using continuous radiostereometric analysis. Papannagari and colleagues44
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree