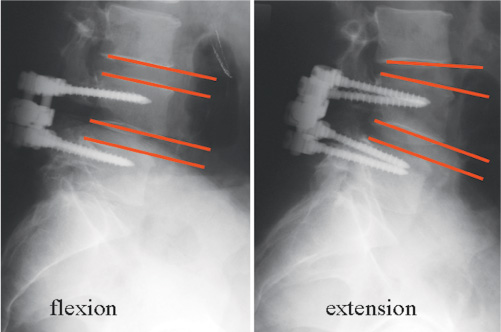
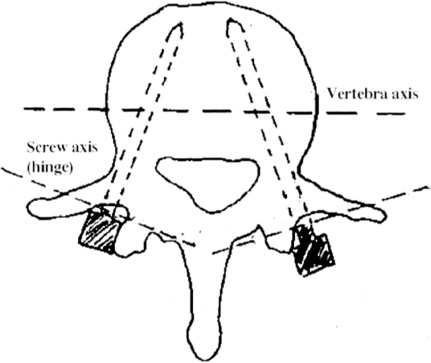
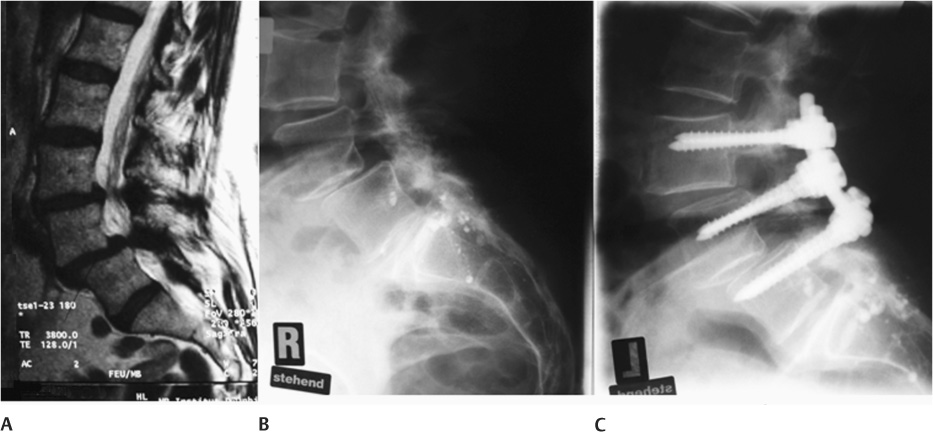
42 Symptomatic Lumbar Stenosis (Claudicatio Spinalis) Chronically Recurring Lumbalgy in the Case of Diskogenic Pain and Facet Syndrome In Combination with a Spondylodesis Extension of an Existing Spondylodesis in the Case of a Painful Adjacent Level Degeneration Stabilizations Extending beyond Three Segments The degeneration of the lumbar motion segment starts with a height loss of the disk caused by water loss of the nucleus pulposus. The facet joints lose their congruence, which may cause a consecutive spondylarthritis.1 The fibers of the annulus fibrosus and the vertebral column ligaments lose tension so that a structural loosening occurs, complete with increased rotation instability.2–4 To compensate for the instability, hypertrophy of the yellow ligament as well as the facet joints occurs very frequently, which may lead to a reduction of the cross-sectional surface of the central as well as the lateral spinal canal. At the same time, the motion segment may lose its original position, and scoliosis, flat back, rotation, and rotation sliding may develop. Further along the course of degeneration, lateral and frontal spondylophytes up to and including syndesmophytes may form, which in turn may lead to spontaneous stiffening of the segment. The complaints depend on the stage of the vertebral column degeneration. In the first phase, with a reduction of the height of the vertebral disk and loss of the congruence of the facet joints, chronically recurrent lumbalgies may occur that increase under load stress. When the stenosis of the spinal channel increases, additional symptoms may occur in one or both legs, with the indications of a claudicatio spinalis. If spontaneous ankylosis of the segment occurs before a symptomatic spinal channel stenosis occurs, the frequency and intensity of lumbalgies decrease. Leg symptoms can be caused by the compression of the neural structures, which results from a narrow spinal channel or recessus or neuroforamen. As a rule, adequate decompression of the neural structures leads to good clinical success. The etiology of the lumbalgy is less clear; also, clinical success does not occur in the same measure as the fusion rate of a spondylodesis. What is certain is that the instability in the motion segment caused by the vertebral disk shrinkage is a trigger for the frequency of lumbalgies. Nonphysiological movements that have become possible due to the vertebral disk shrinkage lead to shifting of the nucleus pulposus or nucleus pulposus fragments within the vertebral disk, with the vertebral disk itself experiencing increased ingrowth of pain-conducting nerve ends as a result of the degeneration.5 This increased innervation of the degenerative vertebral disk is also responsible for the “memory pain” in the diskography.6 The term instability used in this context has been better defined by Panjabi as a “clinical instability” that leads to a pathological movement capability and to pain, deformities, and neurological failures.7 Operative treatment of the symptomatic lumbar vertebral column degeneration has thus far consisted of stabilizing, correcting, and adequately decompressing the diseased segment (s), always in connection with a spondylodesis. In recent years, the various forms of the spondylodesis [anterior and posterior lumbar interbody fusion (ALIF and PLIF), total lumbar interbody fusion (TLIF), posterior lumbar fusion (PLF)] were discussed intensively because 360 degree fusions were believed to provide the greatest clinical success rate. This theory was disproved in a prospective, randomized, double-blind study. The clinical results were independent of the selected fusion form. Complications naturally increased with increased surgical effort (360 degree fusion). In this study, pseudarthroses did not have any influence on the clinical result.8 A possible disadvantage of spondylodesis in the treatment of degenerative lumbar vertebral column diseases is the increased risk of accelerating degenerative processes in the neighboring segment. Following a spondylodesis, 16.5% symptomatic vertebral disk degenerations after 5 years were expected in the neighboring segment, and 36.1% after 10 years.9 Obviously there is a lower risk for spondylodeses without the use of pedicle screw systems.10 It must be questioned whether the risk for the adjacent segment increases with the rigidity of the spondylodesis, which would above all concern the currently favored 360 degree fusions that use a cage in combination with a pedicle screw system.11–13 This does not appear to apply to spondylodeses that were performed for the correction of extended deformities. Thus, even after more than 20 years following a Harrington spondylodesis, low back pain was found in only 13% of cases.14 Until recently, there were few alternatives to a standard spondylodesis. One important reason is that the surgery of the degenerative lumbar vertebral column is a relatively young chapter in spine surgery. The techniques of correction and fusion, so successful in scoliosis surgery, were transferred to this new area of spine surgery, increasing in usage since the early 1980s. An essential task of the spondylodesis consists of protecting the implants used against failure (dislocation, breakage). In contrast to the treatment of adolescent scoliosis, where the correction of the deformity is also the objective of the treatment, there are not very many indications for correction of the degenerative lumbar vertebral column that actually serve the direct objective of the operation with pain release and restoration of neurological functions. Positional deformities in the sagittal and frontal planes that in total do not lead to a loss of the body vertical plumb line need not be corrected. This concerns most lateral deviations. Therefore, the correction of a degenerative lumbar scoliosis is only necessary in exceptional cases. The reduction of the vertebral disk always leads to flattening of the lumbar vertebral column, which also does not need to be corrected as long as the patient assumes an upright, well-balanced posture. True and degenerative olistheses at an adult age are not usually progressive. Stabilization and decompression without correction lead to the objective of the treatment. Therefore, it is not meaningful to transfer the principles of scoliosis surgery noncritically to the surgery of the degenerative lumbar vertebral column. A fusion is required when corrections (mostly in the sagittal plane) are necessary to treat pain. The precondition is a dynamic implant that does not require the protection of a spondylodesis. It must be possible to achieve the treatment objective (pain release, restoration of the neurological function) without correction. The stabilization does not need to include more than three segments. A posterior nonfusion implant system, which can do without protection by a spondylodesis, should not have any rigid characteristics. However, to be able to control instabilities effectively, the system must also feature stable characteristics. The Cosmic Posterior Dynamic System (Ulrich GmbH & Co. KG, Ulm, Germany) is a stable, nonrigid implant. Stability is assured by the 6.25 mm rod, and nonrigidity is assured by the hinged screw head. The screw features a hinged joint between the head and threaded part, which causes the load to be shared between the implant system and the anterior vertebral column (Fig. 42–1). Laboratory tests show that Cosmic allows the same rotation stability as a healthy motion segment.15 In a cyclic loading test with 0.3–3.0 kN/1Hz, we did not find an implant breakage or any debris after 10 million cycles.16 Because Cosmic is used like a stability endoprosthesis, the bone healing of the pedicle screws is of major importance here. For this reason, the threaded part of the screw is coated with bonit. Bonit (Dot GmbH, Rostock, Germany) is the second generation of bioactive calcium phosphate coatings on implants. In 1995, it was originally used for the first time in oral surgery for dental implants.17 In the area of vertebral column surgery, a study on the use of a first-generation bioactive calcium phosphate coating on Schanz screws found significantly improved fixation of the coated screws in comparison with uncoated screws.18 Thus the screw is introduced transpedicularly into the vertebral body, similar to an orthopedic endoprosthesis. To achieve a sufficient press-fit, the pedicle is widened by drilling to 3.2 mm maximum; but only along 50% of the screw. The screw has a self-tapping thread so that the tapping instrument is needed only in cases of extremely hard spongiosa. To prevent early loosening of the screw, the screw must not be manipulated in any major way. Before being implanted, the rods must be prebent such that they can be connected without any problems to the screw heads. Figure 42–1 Cosmic screw. After the screw heads have been connected to the longitudinal rods, there remains only a micromobility in the hinges, which, without rod connections, are caudally and cranially mobile by ~20 degrees (Fig. 42–2). Due to its good rotation stability, Cosmic is used not only for purely diskogenic pain conditions but is also combined with a conventional laminectomy or even a facetectomy. A transverse stabilizer is used for a monosegmental application in combination with a laminectomy. For two- or three-segmental applications, no transverse stabilizer is used. The screws are implanted either by means of a conventional midline approach (point of entry lateral to the facet joint, angle ~15 degrees horizontal to the sagittal plane) or by means of the more laterally situated Wiltse access (a somewhat ventrally located point of entry close to the base of the transverse continuations, angle 20–25 degrees horizontal to the sagittal plane) (Fig. 42–3). A purely sagittal implantation direction is not recommended because this will lead to parallel positioning of the hinges and thus to increased mobility in the sagittal plane. Figure 42–2 Flexion-extension view, 1 year postoperatively. Figure 42–3 Angle of screw direction in the horizontal plan 15 to 25 degrees. Before the rod is implanted, the correct positioning of the patient will be rechecked by means of lordosis that is as physiological as possible. To avoid any early loosening, correction forces must not be applied to the screw. Stand-alone decompression of the spinal channel carries the risk of a recurrence of spinal narrowed because the instability that led to the hypertrophy of the yellow ligament and the facet joints is not taken into consideration. In addition, lumbalgies and deformities may increase as an expression of the increased clinical instability. For this reason, we always carry out an additional stabilization with Cosmic (Fig. 42–4A–C). Degenerated disk disease is present if, in the magnetic resource tomography (MRT), vertebral disk dehydration with height loss and positive Modic signs is detected. If there are further changed vertebral disks (black disk), we carry out an additional diskography. A positive memory pain confirms the suspicion of symptomatic vertebral disk degeneration.19 In the case of a facet syndrome, we carry out a diagnostic local anesthesia under x-ray control, using 2 mL local anesthetic, respectively. If the pain subsides for some hours, the suspected diagnosis is confirmed. In such cases we carry out the Cosmic stabilization using a paraspinous transmuscular approach according to Wiltse20 (Fig. 42–5A–C). In the case of a second recurrence of a disk herniation we carry out a stabilization with Cosmic in addition to the nerve root decompression. Figure 42–4 (A) Spinal stenosis, (B) pseudospondylolisthesis, (C) decompression and stabilization with Cosmic.
Nonfusion Stabilization of the Degenerated
Lumbar Spine with Cosmic
 Why Are Spondylodeses Performed in the Treatment of Degenerative Lumbar Vertebral Column Diseases?
Why Are Spondylodeses Performed in the Treatment of Degenerative Lumbar Vertebral Column Diseases?
 When Is a Correction Necessary?
When Is a Correction Necessary?
 When Will It Be Possible to Do without a Fusion?
When Will It Be Possible to Do without a Fusion?
 Indications for Dynamic Stabilization with Cosmic
Indications for Dynamic Stabilization with Cosmic
Why Are Spondylodeses Performed in the Treatment of Degenerative Lumbar Vertebral Column Diseases?
When Is a Correction Necessary?
When Is a Fusion Necessary?
When Will It Be Possible to Do without a Fusion?
The Cosmic Implant System
Indications for Dynamic Stabilization with Cosmic
Symptomatic Lumbar Stenosis (Claudicatio Spinalis)
Chronically Recurring Lumbalgy in the Case of Diskogenic Pain and Facet Syndrome
Recurrent Disk Herniation
In Combination with a Spondylodesis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 When Is a Fusion Necessary?
When Is a Fusion Necessary? The Cosmic Implant System
The Cosmic Implant System Contraindications
Contraindications Surgical Technique
Surgical Technique Results
Results Discussion
Discussion