and Berthold Rzany2
(1)
Clínica Médica Dr Mauricio de Maio, São Paulo, São Paulo, Brazil
(2)
RZANY & HUND Privatpraxis für Dermatologie und Ästhetische Medizin, Kurfüstendamm, Berlin, Germany
7.1 Inverted Nipple
7.1.1 Introduction
7.1.2 Anatomy
7.1.4 Techniques
7.2.1 Introduction
7.2.2 Anatomy
7.2.4 Material to Be Used
7.2.5 Anesthesia
7.2.6 Techniques
7.3.1 Introduction
7.3.2 Anatomy
7.3.4 Material to Be Used
7.3.6 Techniques
Abstract
Patients with inverted nipples are usually ashamed of their condition and may seek surgical correction, often with variable final results. Patients weary of a surgical approach might benefit from filler injections as described in this chapter.
7.1 Inverted Nipple
7.1.1 Introduction
Patients with inverted nipples are usually ashamed of their condition and may seek surgical correction, often with variable final results. Patients weary of a surgical approach might benefit from filler injections as described in this chapter.
7.1.2 Anatomy
The nipple area complex consists mostly of connective tissue and glands. Specifically, the Montgomery glands: large intermediate-stage sebaceous glands which are embryologically transitional between sweat glands and mammary glands. The Montgomery glands lead to the Morgagni tubercles, which are small (1–2-mm-diameter) raised papules on the areola. The nipple-areolar complex also contains many sensory nerve endings, smooth muscle, and an abundant lymphatic system called the subareolar or Sappey plexus (Nicholson et al. 2009).
7.1.3 Patient Evaluation and Selection
Patients that may benefit from the use of injectable fillers in the nipple area include those whose nipples are easily protruded by cold or local stimulation. Patients with local retractions or previous surgery will have limited to no results. Before indicating the use of injectables for the nipple area, it is important to guarantee that patients are properly assessed and have no medical conditions in their breasts. Further, only HA products should be used.
7.1.4 Techniques
Besides providing anesthesia, the local infiltration with lidocaine of the nipple area will show the degree of correction which can be achieved. Usually a total amount of 1.0 ml is sufficient for the nipple and areola complex. It is important to inject into the nipple by bolus technique and into the areola complex by fan technique to give support at the bottom of the nipple. The use of a 21G blunt cannula is preferable since the use of needles may cause inadvertent intraductal product placement which is not desirable and may lead to cysts and injection. No antibiotics are needed. With the correct patient selection, results are expected to last up to 2 years or more (Figs. 7.1, 7.2, and 7.3).
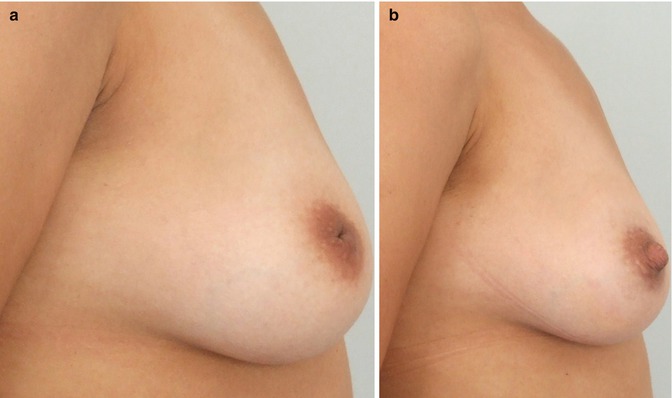
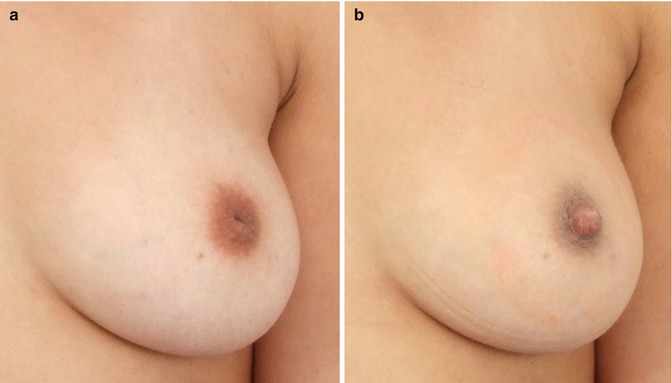
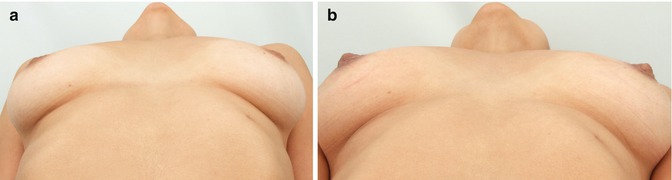
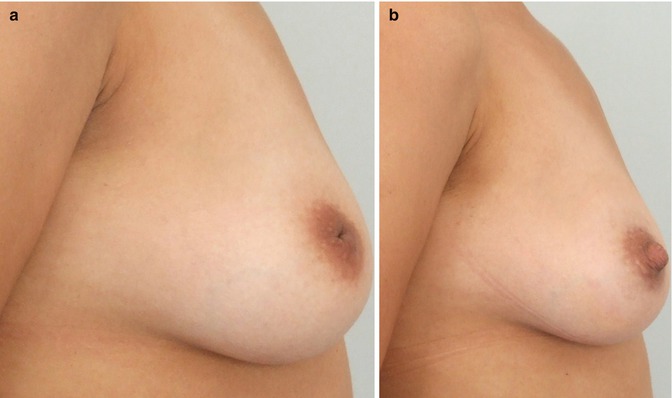
Fig. 7.1
(a, b) Inverted nipple on profile view. A total of 1.0 ml of Juvéderm Voluma was injected with a 21G blunt cannula. Full correction of the deficiency was obtained
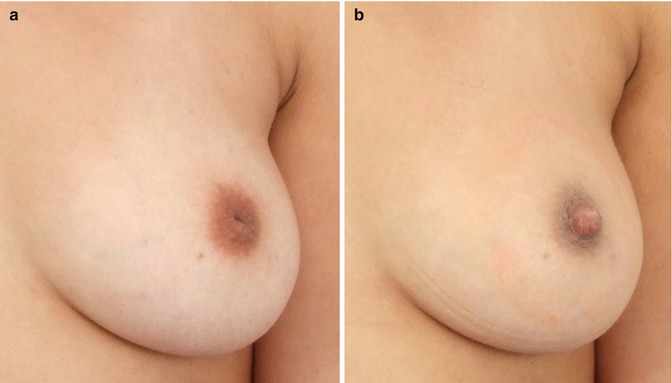
Fig. 7.2
(a, b) Frontal analysis of the correction of the inverted nipple
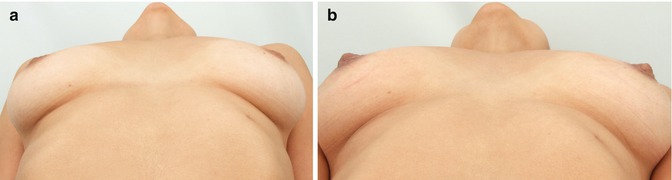
Fig. 7.3
(a, b) Bottom view: Not only the inverted nipples were corrected, but a nice projection of them was obtained
7.1.5 Tips, Tricks and Key Points
Do’s
Inject a local anesthetic first to (1) evaluate the degree of correction that is possible and (2) provide anesthesia.
Use medium- or high-density HAs.
Don’ts
Do not use low-density HA products for this indication, because they are not as long-lasting and patients will be disappointed.
Key Points
In patients with unilaterally inverted nipples, a malignancy should be ruled out beforehand. Bilaterally inverted nipples are usually benign. However again, a thorough past history and inspection should be performed before the aesthetic procedure.
7.2 Hand Volume Replacement
Second only to the face, the dorsum of the hand is the area most visibly affected by aging. Volume loss is often accompanied here by the thinning of epidermis and dermis as well as irregular pigmentation. Therefore, injectable fillers are only one part of hand rejuvenation. To decrease pigmentation or other signs of photoaging, other tools such as lasers or chemical peels must be used to achieve overall best results.
In the past, volume replacement in hands was mainly undertaken by lipofilling. Lately, the introduction of HA volumizers and also CaHa has revolutionized this area.
7.2.1 Introduction
Volume loss of the dorsum of the hand is related to lipoatrophy. The volume loss can be graded from 0 to 4 using a recently developed clinical scale (Table 7.1) (Carruthers et al. 2008).
0 | No loss of fatty tissue |
1 | Mild loss of fatty tissue and mild visibility of veins and tendons |
2 | Moderate loss of fatty tissue and mild visibility of veins and tendons |
3 | Severe loss of fatty tissue and moderate visibility of veins and tendons |
4 | Very severe loss of fatty tissue and marked visibility of veins and tendons |
Lipoaugmentation (Butterwick 2002) and several fillers have been used for this indication (Abrams and Lauber 1990; Fournier 2000; Coleman 1999; Butterwick 2005; Redaelli 2006; Busso and Applebaum 2007; Becker-Wegerich 2008; Man et al. 2008). The evidence, however, is quite limited. There is a small clinical trial (n = 10) investigating hyaluronic acid (Restylane) versus collagen (CosmoPlast). In this small study (Man et al. 2008), the HA did better than the collagen. Besides that, there is a larger case series on poly-l-lactic acid (Redaellie 2006) in which 2–4 ml of a highly diluted poly-l-lactic acid mixture was injected in 3–6 sessions as well as two case reports on hydroxylapatite (Busso and Applebaum 2007) and another on hyaluronic acid (Becker-Wegerich 2008).
7.2.2 Anatomy
The carpus is formed out of two rows – a proximal and a distal – of four carpal bones each. The metacarpus is composed of five short hollow bones. The back of the hand is covered by thin connective tissue so that the bones can be easily felt. The visible and palpable bones serve as leading structures for nerves and blood vessels from the forearm to the dorsal hand. The skin is easily movable over the superficial fascia and can be lifted in folds. Due to the loose and flexible structure of the subcutaneous connective tissue, large amounts of fluids can accumulate causing edema. The tissue flexibility offers ideal conditions for the injection and distribution of fillers. As the veins are minimally fixed by subcutaneous fat, they are to a certain extent movable, reducing the risk for puncture. Cutaneous nerves lie deeper than veins and do not follow their path. They have variable patterns of branching so that the visible veins cannot be perceived as guiding structures to protect cutaneous nerves.
Subcutaneously, the veins coming from the digiti (usually two joined by anastomoses) are continued in the dorsal metacarpal veins of which three are usually particularly well developed. The largest are the dorsal metacarpal veins at the root of the fourth digit which, after merging, become the accessory cephalic vein leading to the forearm. The dorsal metacarpal vein of the fifth digit represents the beginning of the basilica vein. A large number of anastomoses interconnect all the veins to form the venous network of the dorsal hand, which may become quite distracting with the volume loss due to aging process.
On the ulnar side, covered by veins, runs the dorsal branch of the ulnar nerve, while radially the terminal parts of the superficial branch of the radial nerve may be found. After removal of the fascia (subfascial layer), the extensor tendons and the branches of the radial artery become visible. In the region of the radial fovea, the radial artery produces the dorsal carpal branch and runs between the heads of the first dorsal interosseous into the palm of the hand. The dorsal carpal branch merges into the dorsal metacarpal arteries, which again divide into the dorsal digital arteries.
7.2.3 Patient Evaluation and Selection
Which patient is right for volume replacement of the hands? Of course, a patient that presents lipoatrophy of the dorsum of the hand. Some patients may complain of mild to moderate prominence of the vein or tendon, while others are only bothered by a severe skeletonized appearance of the hands. Depending on the grade of lipoatrophy, the choice of filler may vary. Please find below the different stages of volume loss with patients of various ages (Fig. 7.4).


Fig. 7.4
Different stages of volume loss of the dorsum of the hands. These are best candidates for volume replacement
There are other hand positions that are useful for evaluating volume loss and prominence of the tendons (Fig. 7.5) and veins (Fig. 7.6) as follows:






Fig. 7.5
Forming a fist to show the tendons
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








