9 Non-surgical skin tightening
Summary and Key Features
• Non-invasive skin tightening is a popular concept with a burgeoning number of devices entering the market
• The main types of non-surgical skin tightening devices include radiofrequency, light, and ultrasound technologies
• Treatment protocols have evolved over the years to focus on reduced energy settings, making the procedures safer and more comfortable for patients
• All skin-tightening devices work by delivering heat in the form of energy to the skin or underlying structures. They create mechanical and biochemical effects that lead to both immediate contraction of collagen fibers and delayed remodeling and neocollagenesis via wound healing
• Patient selection is key for best results and overall patient satisfaction
• Patients who are concerned about risk and recovery and who are willing to accept reduced efficacy in exchange for an improved side effect and healing time profile are ideal candidates for non-ablative approaches
• Non-ablative skin-tightening devices are capable of improving both skin laxity and facial contours. The physician must analyze the patient’s three-dimensional facial structure to determine those areas that would benefit most from the procedure. Typically, this would include the upper face / brow region and the lower face / jawline region
• Skin-tightening procedures can be performed along with fillers, neurotoxins or other laser or light-based devices to address multiple issues and achieve a more global overall improvement
• Rarely, patients may experience side effects related to overly aggressive treatment such as burns, indentations, scars or changes in pigmentation. The overall incidence of such problems is extremely low with all current devices owing to updated protocol trends using lower energies and patient feedback as a guide to safe energy delivery
Introduction
In terms of skin laxity specifically, the gold standard of treatment remains rhytidectomy or surgical redraping. The goal of this chapter is to review the major types of minimally invasive, non-ablative tissue tightening techniques, including radiofrequency-, light-, and ultrasound-based devices (Table 9.1). These devices are not a replacement for surgical procedures and appropriate patient selection remains key to overall satisfaction.
Table 9.1 Major types of skin-tightening technologies
| Skin-tightening technology | Device |
|---|---|
| Monopolar radiofrequency | Thermage® (Solta) |
| Pelleve® (Ellman) | |
| Bipolar radiofrequency with light energy | Galaxy®, Aurora®, Polaris®, ReFirme® (Syneron) |
| Bipolar radiofrequency with vacuum | Aluma® (Lumenis) |
| Bipolar radiofrequency delivered via a micro-needle electrode array | ePrime® (Candela-Syneron) |
| Broadband infrared light | Titan® (Cutera) |
| StarLux IR® (Palomar) | |
| SkinTyte® (Sciton) | |
| Unipolar and bipolar radiofrequency | Accent® (Alma) |
| Ultrasound technology | Ulthera® (Ulthera) |
Thermal collagen remodeling
All skin-tightening devices work by delivering heat in the form of energy to the skin or underlying structures. This creates mechanical and biochemical effects that lead to both immediate contraction of collagen fibers and delayed remodeling and neocollagenesis via a wound-healing response (Box 9.1).
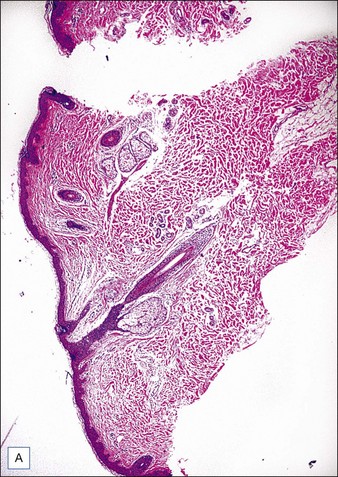
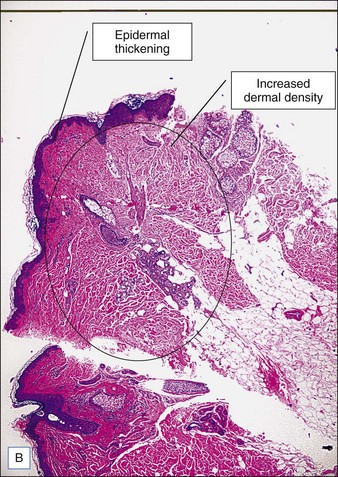
Collagen fibers are composed of a triple helix of protein chains linked with interchain bonds into a crystalline structure. When collagen fibers are heated to specific temperatures, they contract due to breakage of intramolecular hydrogen bonds. Contraction causes the crystalline triple helix structure to fold, creating thicker and shorter collagen fibers. This is thought to be the mechanism of action of immediate tissue tightening seen after skin-tightening procedures. Studies have also found selective contraction of fibrous septae in the subcutaneous fat, which is thought to be responsible for the inward (Z-dimension) tightening (Fig. 9.1).
Radiofrequency devices
Radiofrequency energy is energy in the electromagnetic spectrum ranging from 300 MHz to 3 kHz. Unlike most lasers, which target specific absorption bands of chromophores, heat is generated from the natural resistance of tissue to the movement of electrons within the radiofrequency field as governed by Ohm’s law (Box 9.2). This resistance, called impedance, generates heat relative to the amount of current and time by converting electrical current to thermal energy. Consequently, energy is dispersed to three-dimensional volumes of tissue at controlled depths.
The configuration of electrodes in a radiofrequency device can be monopolar or bipolar, and both have been used for cutaneous applications. The main difference between the two is the configuration of electrodes and type of electromagnetic field that is generated. In a monopolar system, the electrical current passes through a single electrode in the handpiece to a grounding pad (Box 9.3). This type of electrode configuration is common in surgical radiofrequency devices because there is a high density of power close to the electrode’s surface with the potential for deep penetration of tissue heating. In tissue-tightening applications, surface cooling is used to protect the outer layers of the skin and heat only deeper targets. In a bipolar system, the electrical current passes between two electrodes at a fixed distance (Box 9.4). This type of electrode configuration has a more controlled current distribution; however, the depth of penetration is limited to approximately one-half the distance between the electrodes.
With radiofrequency technologies, the depth of energy penetration depends upon not only the configuration of the electrodes (i.e. either monopolar or bipolar), but also the type of tissue serving as the conduction medium (i.e. fat, blood, skin), temperature, and the frequency of the electrical current applied (Box 9.5). Tissue is made up of multiple layers, including dermis, fat, muscle, and fibrous tissue, all of which have different resistances to the movement of radiofrequency energy (Table 9.2). Structures with higher impedance are more susceptible to heating. In general, fat, bone, and dry skin tend to have low conductivities such that current tends to flow around these structures rather than through them. Wet skin has a higher electrical conductivity allowing greater penetration of current. This is why, in certain radiofrequency procedures, improved results can be seen with generous amounts of coupling fluid and increased hydration of skin. The structure of each individual’s tissue (dermal thickness, fat thickness, fibrous septae, number and size of adnexal structures) all play a role in determining impedance, heat perception, and total deposited energy despite otherwise equal parameters.
Table 9.2 Dielectric properties for human tissue at 1 MHz and room temperature
| Type of tissue | Electrical conductivity (Siemens/m) |
|---|---|
| Bone | 0.02 |
| Fat | 0.03 |
| Dry skin | 0.03 |
| Nerve | 0.13 |
| Cartilage | 0.23 |
| Wet skin | 0.22 |
| Muscle | 0.50 |
| Thyroid | 0.60 |
Monopolar radiofrequency
The first monopolar tissue-tightening device on the market was the ThermaCool® device (Solta Medical, Hayward, CA), introduced in 2001. It remains the most exhaustively studied and published apparatus. The ThermaCool® device uses a capacitive coupled electrode at a single contact point and a high-frequency current at a frequency of 6 MHz. A disposable membrane tip is used to deliver the energy into the skin, with an accompanying adhesive grounding pad serving as a low-resistance path for current flow to complete the circuit. The use of capacitive rather than conductive coupling is important because it allows the energy to be dispersed across a surface to create a zone of tissue heating. With conductive coupling, the energy is concentrated at the tip of the electrode, resulting in increased heating at the contact surface and an increased risk of epidermal injury (Fig. 9.2).

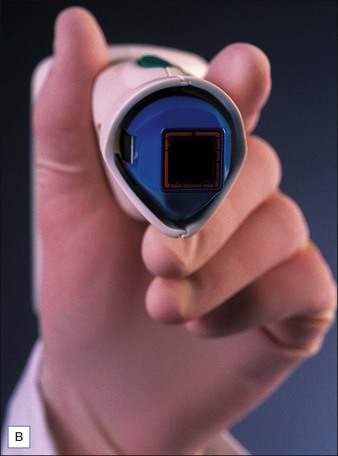
Figure 9.2 (A) Thermage ThermaCool® device; (B) capacitively coupled electrode treatment tip.
Photographs courtesy of Solta.
In the early clinical experience, one of the main drawbacks to the ThermaCool® procedure was a high degree of discomfort during the procedure, requiring heavy sedation or frank anesthesia. The protocol at that time was to perform 1–2 passes at higher energies. The treatments were quite painful, results tended to be inconsistent from patient to patient, and some adverse events such as fat necrosis and atrophic scarring were noted. Over the years, treatment protocols have evolved to a paradigm utilizing lower energies, multiple passes, and patient feedback on heat sensation as the end point of therapy. This has all but eliminated the risk of unacceptable side effects and has greatly reduced the pain involved such that most procedures can be performed without any anesthesia. Monopolar radiofrequency energy is now commonly used to accomplish skin tightening of the face, eyelids (Case study 1), abdomen (Fig. 9.3), and extremities.
The clinical results of non-ablative radiofrequency skin tightening were first reported by Fitzpatrick and colleagues for the periorbital area in 2003. At least some degree of clinical improvement was reported in 80% of subjects (Figs 9.4–9.6) In 2006, Dover and colleagues compared the original single-pass, high-energy technique with the updated low-energy, multiple-pass technique using immediate tissue tightening as a real-time end point. With the original treatment algorithm, 26% of patients saw immediate tightening, 54% observed skin tightening at 6 months, and 45% found the procedure overly painful. With the updated protocol, 87% had immediate tissue tightening, 92% had some degree of tightening at 6 months, only 5% found the procedure overly painful, and 94% stated the procedure matched their expectations (Figs 9.7, 9.8). The low-energy, multiple-pass protocol has also been reported to be significantly safer, lowering the incidence of adverse events to less than 0.05%.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree