Chapter 57 Neonatal infections
1. What are the TORCHES infections in a neonate?
2. Describe the cutaneous findings in neonatal herpes simplex viral (HSV) infections.
HSV infection usually presents as grouped vesicles on an erythematous base. These lesions can be present on any part of the skin but are more common on the face, scalp, or buttocks (Fig. 57-1). They may also be generalized or disseminated or occur in the perianal region in a breech-delivered baby. In the intrauterine-exposed baby, they may present as atrophic areas with scarring.
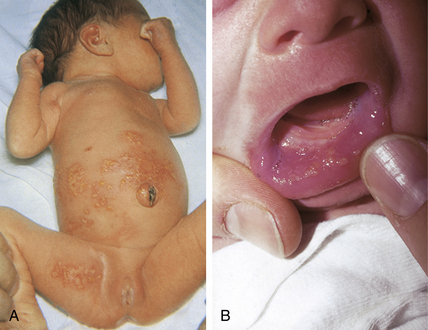
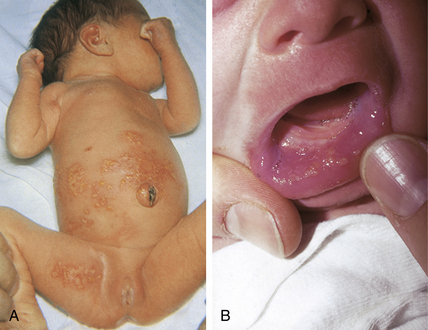
Figure 57-1. A, Congenital herpes simplex virus infection. B, Congenital mucosal herpes simplex virus infection.
(Courtesy of William L. Weston, MD.)
3. Is neonatal herpes simplex dangerous?
Neonatal herpetic infections are usually severe (especially if lesions are disseminated or the central nervous system [CNS] is involved) and require immediate diagnosis and treatment. The majority of infants with HSV infection acquire it in the intrapartum period or postnatally. Even with adequate treatment, the mortality rate approaches 50% in infants with disseminated disease, and the incidence of long-term morbidity is significant.
Kohl S: Herpes simplex virus. In Behrman R, Kliegman R, Jenson H, editors: Nelson textbook of pediatrics. Philadelphia, 2004, WB Saunders, pp 1051–1057.
4. What percentage of herpes-infected neonates display skin or mucosal lesions?
About 65% of infected infants display lesions shortly after birth, with disseminated disease occurring during the first 2 weeks of life. This includes infants with skin, eye, and mouth lesions (40%) as well as those with disseminated disease (25%) that includes the skin. If intrauterine exposure has occurred, lesions are usually present at birth. Fortunately, intrauterine transmission of HSV occurs in fewer than 5% of cases.
Jacobs RF: Neonatal herpes simplex virus infections, Semin Perinatol 22:64–71, 1998.
6. What tests can be done to diagnose herpes infections? How should material be obtained for these tests?
To obtain specimens for diagnostic testing, scrape the base of a blister and smear the material on a microscope slide. Stain (e.g., Wright’s stain) and look for multinucleated giant cells. If available, send another slide for a HSV-fluorescein antibody test. Confirmation of a cytopathic effect can be made by immunofluorescence using antibodies specific to HSV-1 and HSV-2. Material from the blister base can be sent for viral culture. The sensitivity of performing a culture is best for a vesicular lesion. It is also advisable to culture urine, nasopharynx, conjunctiva, and cerebrospinal fluid, if indicated. The polymerase chain reaction (PCR) detects viral DNA and can be important in diagnosing HSV encephalitis.
7. What is congenital varicella syndrome?
Intrauterine infection with varicella virus that occurs in the first trimester may result in congenital varicella syndrome. These infants are born with hypoplasia of the limbs and exhibit cutaneous zosteriform scars and atrophy. Interestingly, there have been reports of neonates developing herpes zoster, which implies that they must have had chickenpox in utero. The future of varicella disease may be altered by the continued use of the varicella vaccine.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








