Fig. 21.1
Two lesions. The first one in the left side on the picture is atrophic, white centre surrounded by brown borders. The second one showed ulcerative centre containing fibrin, surrounded by erythematous, active borders

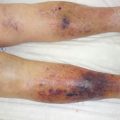
Fig. 21.2
Waxy, smooth, white plaque surrounded by erythematous borders
As mentioned, the lesions are mostly painless due to nerve damage, but ulcerated lesions may cause pain. These ones may occur following minor trauma in up to 35 % of cases [4].
In 90 % of patients NL arises on legs, bilaterally and symmetrically [1]. Less frequently, lesions may appear on the scalp, face, trunk, forearms and penis, which are less considered associated with diabetes mellitus [1, 5].
The progression is slow, and sometimes regression of lesions may happen in 20 % of cases [1]. The main complication is ulceration [1, 4] with secondary infection [6]. Some exceptional cases of squamous cell carcinoma have been reported in long standing NL [1, 4]. The origin of malignant transformation is even unclear [4].
21.5 Treatment
The first step is to prevent lesions by avoidance of trauma [2]. Indeed, NL may also occur by Koebner effect, in addition to ulceration risk [2, 4]. Control of diabetes seems to be without any improvement [1, 4, 5].
Several treatments have been tested with random results. Most of them are based on case reports.
Treatment by topical corticosteroids is effective to prevent progression and reduce inflammatory process, especially on the active borders [1, 2, 4, 5].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree