, Madan Ethunandan2 and Tian Ee Seah3
(1)
Poole Hospital NHS Foundation Trust, Poole, Dorset, UK
(2)
Department of Oral and Maxillofacial Surgery, University Hospital Southampton NHS Trust Southampton General Hospital, Southampton, UK
(3)
Orange Aesthetics and Oral Maxillofacial Surgery, Singapore, Singapore
Subunits and Anatomical Considerations
The circumferential neck unit can be defined superiorly by the lower border of the mandible anteriorly and the hairline posteriorly. The inferior limits are the clavicle anteriorly and the upper border of the scapula posteriorly. The neck can be divided into anterior and posterior subunits, with the anterior subunit being further divided into a midline and two lateral units (Fig. 12.1).
Fig. 12.1
Neck subunits
The thickness and mobility of the neck skin varies with the location and is often defined by the age of the person and general body habitus. The platysma muscle overlies the investing layer of the cervical fascia and is often dehiscent in the midline. The anterior and external jugular veins lie immediately beneath the muscle. The nerves of the cervical plexus emerge from the posterior border of the sternomastoid muscle and along with the mandibular and cervical branches of the facial nerve also lie beneath the platysma. The RSTLs are obliquely and transversely oriented in the neck.
The skin of the posterior neck is thicker than that in the anterior/lateral neck and is less mobile. The trapezius muscle enclosed by the investing layer lies beneath the skin.
The skin redundancy and the RSTLs allow flaps to be raised in the neck to reconstruct a variety of neck and adjacent defects, with good aesthetic outcomes. It also enables relatively large defects to be closed primarily.
Central Neck
Primary Closure
Indications
Small and medium defects
Technique
The defect is converted into an ellipse, along the RSTLs. The wound margins can be undermined superficial or deep the platysma and closed in layers (Fig. 12.2a–c).
Tips
Care should be taken to avoid damage to the underlying nerves and vessels, if dissection is undertaken deep to the platysma.
O-Z Flap
Indications
Small- and medium-sized defects
Technique
The defect is modified into a circle. Two curvilinear incisions are made from the opposite poles of the defect. The flaps are elevated superficial or deep to the platysma and mobilised into the defect. The wounds are closed in layers (Fig. 12.3a–c).
Tips
In the case of circular defects, the direction of the “Z” can be adjusted according to the area of maximum skin laxity and RSTLs. Care should be taken to avoid damage to the underlying nerves and vessels, if dissection is undertaken deep to the platysma.
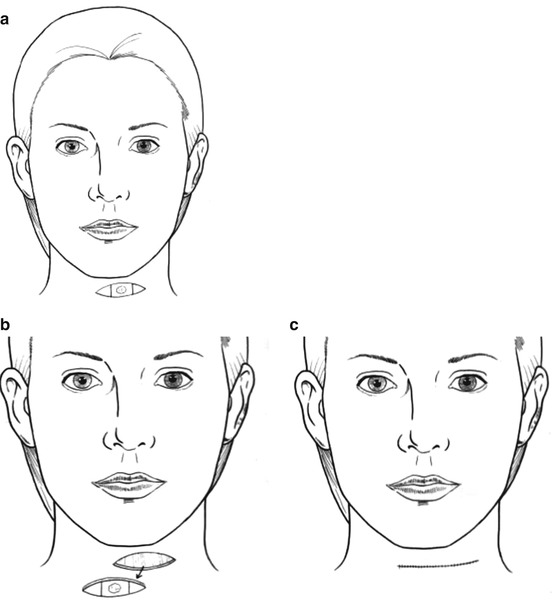
Fig. 12.2
Primary closure
Rhombic Flap
Indications
Medium-sized defects









