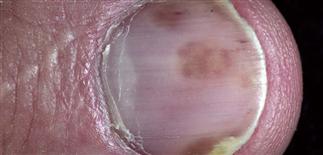
Nail pitting is a change seen in psoriasis. The nails appear to have a tiny ice pick depression. Affected by psoriasis, this nail has distal subungual hyperkeratosis, onycholysis, and a yellow-brown color change termed oil spot lesion, due to serum accumulation. All five fingernails are affected with psoriasis. There is onycholysis and some yellow-brown discoloration typical of oil spot change. The oil spot sign of psoriasis is a brown color. Often, there are other psoriasis findings such as onycholysis or pitting. Nail changes are characteristic of psoriasis, and the nails of all patients with suspect psoriasis should be examined. Psoriasis of the nails may be the only sign that the patient has psoriasis; these patients may have no skin lesions. • The incidence of nail involvement in psoriasis varies from 10–50%. • Nail involvement may be the only sign of psoriasis, but it usually occurs simultaneously with skin disease. One or several nails may be involved. • Pain may restrict activities. • Pitting is the most common finding. There may be a few or many pits, and they are haphazardly distributed on the nail plate surface. • Onycholysis is separation of the nail from the nail bed. Separation begins at the distal groove or under the nail plate and may involve several nails. The separated nail appears yellow and is often misinterpreted as a fungal infection. • Subungual scaly debris may accumulate under the distal nail plate. The yellow-white debris elevates the distal nail. This also is commonly mistaken for nail fungus infection. • Surface distortion of the nail plate occurs when psoriasis affects the nail matrix. • Oil spot lesions are yellow-brown spots seen through the nail surface. Psoriasis of the nail bed causes serum and scaling debris to accumulate under the nail plate. • Nail psoriasis may have a very similar appearance to tinea of the nail unit. Culture of nail clippings or subungual debris, potassium hydroxide preparations, and nail biopsy will help establish the diagnosis of fungal nail infection. Nail biopsy is performed by submitting nail clippings to the laboratory for histologic identification of hyphae to rule out fungal infection. • Many topical agents (calcipotriol, tazarotene, and anthralin) have been tried, but results are discouraging. • Intralesional injections at monthly intervals into the matrix and lateral nail folds are effective but painful. Triamcinolone acetonide (Kenalog) 2.5–5 mg/mL is delivered with a 30-gauge needle. The procedure is painful and most patients do not continue. • Treatment of skin disease with systemic agents such as tumor necrosis factor inhibitors adalimumab, etanercept, or other immune suppressive such as ciclosporin, methotrexate, or acitretin will improve the nails, but not indicated for nail disease alone. 154b Acute paronychia. The pus is collecting in the lateral nail fold and should be drained. The most common cause is Staphylococcus aureus. Chronic paronychia presents as swelling and tenderness of the proximal and lateral nail folds. The problem often occurs if there is repeated wet work. Candida is the most common cause. Separation of the nail from the nail bed results in a warm moist space that predisposes to Pseudomonas infection (green color) under the nail. Soaking the finger makes it worse.
154a
Nail diseases: Psoriasis



DESCRIPTION
HISTORY
PHYSICAL FINDINGS
TREATMENT
Nail diseases: Paronychia, Pseudomas infection, white spots or bands



![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine






