Chapter 30 Mycobacterial infections
1. What is the classification system of mycobacteria?
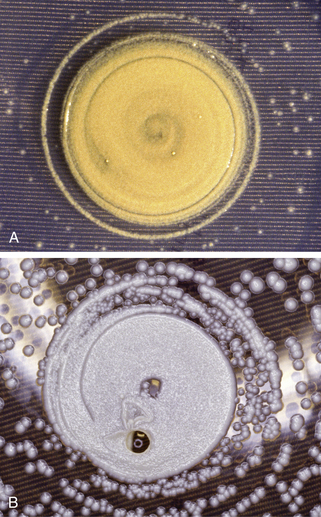
Extensive taxonomic work has been done to classify the more than 60 species of organisms belonging to the genus Mycobacterium. In the 1950s, Runyon classified the atypical mycobacteria based on their rate of growth, ability to form pigment, and colony characteristics (Fig. 30-1). The Runyon classification may also include distinctions among obligate human pathogens requiring direct person-to-person transmission, facultative human pathogens found in the environment that are rarely responsible for direct person-to-person spread, and nonpathogens (Table 30-1).
2. What are the staining characteristics of mycobacteria?
Mycobacteria are aerobic, non–spore-forming, nonmotile bacilli. They do not stain readily, but their most useful staining characteristic is acid fastness. Acid fastness refers to the ability to retain carbol fuchsin dye after washing with acid or alcohol as a result of a high content of cell wall mycolic acids, fatty acids, and other lipids. The acid-fast stain is also called the Ziehl-Neelsen stain. Other staining methods include the Dieterle, Fite, hematoxylin-eosin, auramine-rhodamine, and phenolic acridine orange stains. Acid fastness is also shared by Nocardia, Rhodococcus, Legionella micdadei, Isospora, and Cryptosporidium.
Table 30-1. Classification of Pathogenic Mycobacteria
| CLASSIFICATION | OBLIGATE HUMAN PATHOGEN | FACULTATIVE HUMAN PATHOGEN |
|---|---|---|
| Slow Growers | ||
| M. tuberculosis complex | ||
| M. tuberculosis | x | |
| M. bovis | x | |
| M. africanum | x | |
| M. mycoti | x | |
| Photochromogens (Runyon Group 1) Form Yellow-Orange or Rust Pigment with Light | ||
| M. kansasii | x | |
| M. marinum | x | |
| M. simiae complex (M. simiae, M. triplex, M. genavense, M. heidelbergense, and M. lentiflavum) | x | |
| Others include M. intermedium, and M. asiaticum | x | |
| Scotochromogens (Runyon Group 2) Form Light Yellow to Orange Pigment with and without Light | ||
| M. scrofulaceum | x | |
| M. szulgai | x | |
| Others include M. injectum, M. lentiflavum, M. gordonae | x | |
| Nonchromogens (Runyon Group 3) Unable to Form Pigment | ||
| M. avium-intracellulare complex (M. avium, M. intracellulare, and other unidentified species) | x | |
| M. haemophilum | x | |
| M. xenopi | x | |
| M. ulcerans | x | |
| Others include M. celatum, M. genavense, M. gastri, and M. malmoense | x | |
| Rapid Growers (Runyon Group 4) Growth within 7 Days | ||
| M. fortuitum | x | |
| M. abscessus | x | |
| M. chelonei ssp. chelonei, abscessus, unnamed subspecies | x | |
| Others include M. phlei, M. smegmatis, M. fredericksbergense | x | |
| Noncultivable Unable to Cultivate in Media | ||
| M. leprae | x | |
Data from Bhambri S, Bhambri A, Del Rosso JQ: Atypical mycobacterial cutaneous infections, Dermatol Clin 27(1):63–73, 2009.
5. What is tuberculosis?
Tuberculosis is a systemic infectious disease that can affect any organ system, including the skin. Only approximately 5% to 10% of infections lead to clinical disease. The lungs, however, are the most commonly involved organ. Cutaneous tuberculosis has a broad clinical spectrum depending on the route of infection, virulence of the organism, and immune status of the host (Table 30-2). Lupus vulgaris and scrofuloderma, although rare, are the two most common forms of cutaneous tuberculosis.
7. Explain the route of infection in cutaneous tuberculosis.
Cutaneous tuberculosis may be acquired by three possible routes. The first route is exogenous infection acquired from an outside source (primary-inoculation tuberculosis and tuberculosis verrucosa cutis). The second route of infection is endogenous spread. This can occur by contiguous spread (scrofuloderma) or by autoinoculation (periorificial tuberculosis) as organisms are passed from internal organ involvement. The final route is through hematogenous or lymphatic dissemination (lupus vulgaris, miliary tuberculosis, and gummas).
Table 30-2. Classification of Cutaneous Tuberculosis
| CLASSIFICATION | PRIMARY INFECTION (NONIMMUNE HOST) | SECONDARY INFECTION (IMMUNE HOST) |
|---|---|---|
| Exogenous | ||
| Primary inoculation tuberculosis | x | |
| Tuberculosis verrucosa cutis | x | |
| Endogenous | ||
| Scrofuloderma | x | |
| Periorificial tuberculosis | x | |
| Hematogenous/lymphatic | ||
| Lupus vulgaris | x | |
| Acute miliary tuberculosis | x | |
| Gummas | x | |
Data from Semaan R, Traboulsi R, Kanj S: Primary mycobacterium tuberculosis complex cutaneous infection: report of two cases and literature review, Int J Infect Dis 12(5):472–477, 2008.
8. Who is at risk of acquiring tuberculosis?
In the United States, the incidence of tuberculosis was decreasing until 1985 when it reached its nadir. Since 1985, the incidence of tuberculosis has markedly increased. Crowded urban environments, immigration, poverty, homelessness, intravenous drug abuse, loss of tuberculosis control programs, increased use of immunosuppressive medications (e.g., TNF-α inhibitors), and, most importantly, the HIV epidemic account for the rising incidence. High-risk groups include the elderly, urban homeless, alcoholics, intravenous drug abusers, prison inmates, migrant farm workers, minorities, and immunosuppressed patients (with HIV or from iatrogenic causes).
9. Describe the histopathologic hallmark of tuberculosis.
The caseation granuloma (also known as tubercle) is the histopathologic hallmark of tuberculosis. This consists of giant cells and epithelioid cells and usually has varying amounts of caseation necrosis. This pattern can also be seen in other infections and is not pathognomonic. Acid-fast bacilli are usually easy to find in the early lesions, but there are very few bacilli once granulomas develop.
10. How can one acquire primary cutaneous tuberculosis?
Primary-inoculation tuberculosis occurs from direct inoculation of M. tuberculosis into the skin and includes the chancre at the site and affected regional lymph nodes. The organism cannot penetrate intact skin and requires a break in the skin, such as a minor cut or abrasion. Reports have also implicated tattooing, ear piercing, circumcision, mouth-to-mouth resuscitation, and needle-sticks. In some cases, there is no documented injury.
11. Describe the clinical manifestation of primary-inoculation cutaneous tuberculosis.
Primary tuberculosis may occur in any age group, but is most common in children up to 4 years of age and young adults. The face, mucous membranes (conjunctiva and oral mucosa), and lower extremity are the usual sites of infection. A tuberculous chancre develops 2 to 4 weeks after inoculation and presents as a painless, firm, red-brown papule/nodule, which slowly enlarges, eventually eroding to form a sharply demarcated ulcer (Fig. 30-2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree