Quantitative MRI of the ACL-Injured and Reconstructed Knee
Keywords
• Knee reconstruction • MRI • ACL injury • Knee
Key Points
Introduction
Late complications of ACL injury, such as cartilage degeneration, were considered to be a consequence of long-standing functional deficit of the ACL itself. Contrary to this expectation, several studies reported that several cases resulted in degenerative arthritis, even after ACL-reconstruction surgery.1–4 These results indicate that initial injury to cartilage and underlying bony architecture may contribute substantially to the long-term outcomes following ACL injuries. Moreover, there needs to be better evaluation of surgical success because knee kinematics or cartilage health may not be restored despite surgical reconstructions. It is important to detect the extent of injury to tissues other than ACL as early as possible to properly guide the patients and obtain satisfactory outcomes. Recent advances in MRI enable physicians to make accurate morphologic assessment on injured structures and to precisely quantify changes in biochemical composition of cartilage and knee kinematics.
Quantitative MRI
MRI techniques have evolved over the past 2 to 3 decades to improve detection of minor changes in morphology of soft tissues as well as bony structures of knee joint. Various sequences, such as fat-suppression techniques, two-dimensional (2D) and three-dimensional (3D) fast spin echo, spoiled gradient-echo, driven equilibrium Fourier transform, dual echo steady state, and balanced steady-state free precession imaging have been used to delineate articular cartilage of knee joint.5 Scoring systems were also devised to accommodate these changes in semiquantitative fashion, including whole-organ MRI score (WORMS),6 the Boston-Leeds osteoarthritis knee score (BLOKS),7 and the knee osteoarthritis scoring system (KOSS).8 High sensitivity and specificity have been reported with these techniques.9
However, early phenomenon of cartilage breakdown does not always manifest as morphologic change. Earlier events of cartilage degeneration that precede morphologic change are known to be changes in its biochemical composition.10 Detection of early biochemical changes in cartilage is amenable with the recent development in MRI techniques. This article addresses some of the new advancements in quantitative MRI of articular cartilage and bone injuries. Recent literature and research in delayed gadolinium-enhanced MRI of cartilage (dGEMRIC), T2 mapping, T1ρ mapping, and magnetic resonance spectroscopy imaging (MRSI) on bone marrow edema-like lesions (BMEL) is discussed.
dGEMRIC
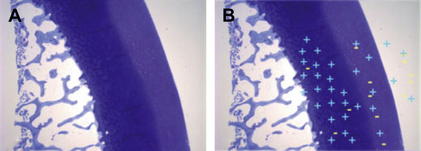
Articular cartilage consists of water, chondrocytes, and extracellular matrix composed of collagen fibrils and proteoglycan, which contains negatively charged glycosaminoglycan (GAG) molecules. Decrease in GAG content is known to be an early event of cartilage breakdown.10 When anions such as gadolinium diethylenetriaminepentaacetic acid (Gd-DTPA)2- enter a joint, they distribute in cartilage inversely to the amount of GAG (Fig. 1). In other words, the more damaged the articular cartilage is, the higher is the concentration of Gd-DTPA2- in the area. The gadolinium-enhanced measurement of tissue T1 values (T1Gd or dGEMRIC index) represents the amount of GAG in cartilage. Low T1Gd index is commonly observed in the area of cartilage degeneration.
Application in ACL Injuries
In an observational longitudinal study, cartilage GAG content after ACL injury was evaluated using dGEMRIC.11 The ACL-injured group (29 subjects) was examined by dGEMRIC at 3 weeks and 2.3 years after injury and compared with a reference cohort (24 normal subjects). T1Gd index was measured at the central weight-bearing portion of lateral and medial femoral cartilage. The healthy reference group showed higher T1Gd value than the ACL-injured group did in both medial and lateral compartments. In the ACL-injured group, the T1Gd index was lower in subjects with concomitant meniscectomy than in subjects without meniscectomy in both medial and lateral compartments. Follow-up dGEMRIC examination in the ACL-injured group showed similar T1Gd values in the medial compartment and minor but significant increase in the lateral compartment. GAG content was lower in the ACL-injured group and more pronounced with associated meniscectomy. T1Gd index was considered to be a useful early biomarker for early posttraumatic osteoarthritis (OA).
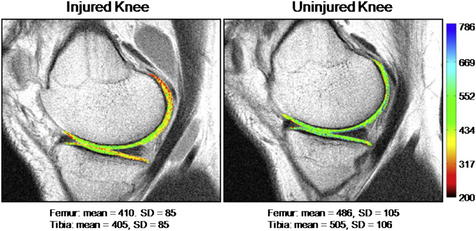
In another study, 15 subjects with unilateral ACL injury were examined using dGEMRIC with the contralateral knee used as control.12 The median time from injury to MRI was 82 days and the median slice of medial compartment was selected for comparison. Index comparisons were made of knee status (ACL-injured vs control group), scan order (ACL-injured first vs control first), and cartilage location (femur vs tibia). There was a significant difference in the mean dGEMRIC indices between injured and uninjured knees (Fig. 2). No significant effects were identified owing to test order or cartilage location.
Disadvantages of dGEMRIC
T2 mapping
Application in ACL Injuries
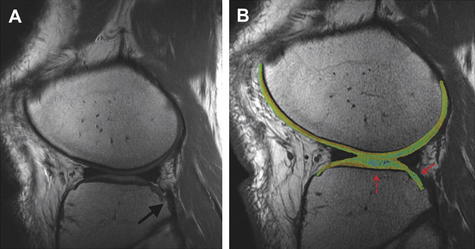
T2 mapping has not been popularized in evaluation of ACL-injured patients. One recent longitudinal study used this technique in part to assess cartilage status of ACL-injured subjects at follow-up.13 Forty-two knees with acute, isolated ACL injury underwent MRI at the time of injury and at yearly follow-up with a maximum of 11 years (Figs. 3 and 4). All subjects showed chondral damage at the time of injury. By follow-up years 7 to 11, the risk of cartilage loss for lateral femoral condyle was 50 times baseline, 30 times for patella, and 19 times for medial femoral condyle.
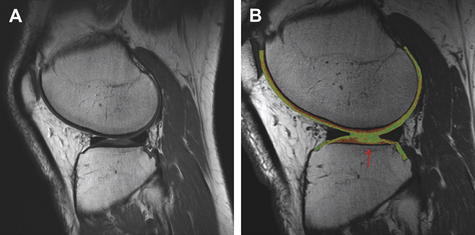
Fig. 4 The patient from Fig. 3, 4 years after injury. (A) Morphologic image shows depression of the far posterolateral tibial plateau. (B) T2 mapping shows progressive prolongation of T2 relaxation times over the central tibial plateau (arrow) compared with the study in Fig. 3.
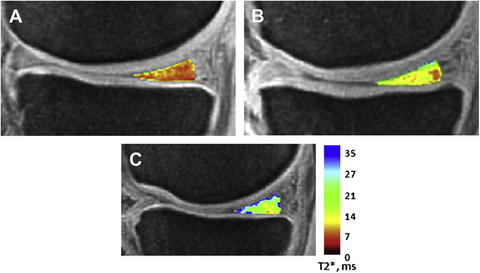
To acquire very short T2 signal from type-I collagen of tendons, ligaments, or menisci, a specific sequence is needed. Ultrashort echo time-enhanced T2* (UTE-T2*) was used in an effort to detect early degeneration of meniscal tissue before surface breakdown.14 The investigators compared UTE-T2* with histologic findings in 16 cadaveric menisci. UTE-T2* values tended to be lower in histologically normal menisci and higher in torn or degenerated tissues. UTE-T2* values of 10 asymptomatic subjects were compared with ACL-injured subjects with or without meniscal tear. Posteromedial meniscus UTE-T2* values in ACL-injured subjects with medial meniscus tear were 87% higher than in asymptomatic control subjects (P<.001). Posteromedial meniscus UTE-T2* values in ACL-injured subjects without medial meniscus tear were 33% higher than control (P = .001) (Fig. 5). The investigators stated that UTE-T2* mapping is sensitive to subclinical degeneration of meniscal tissue.
Review
Advantages of T2 mapping
Disadvantages of T2 mapping
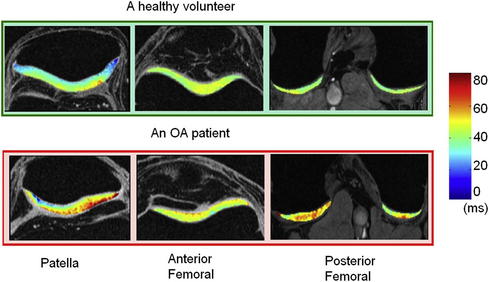
T1ρ mapping
T1ρ mapping can measure the low-frequency interactions between spinning hydrogen proton and local macromolecular environment. Therefore, changes in local macromolecular environment, such as proteoglycan depletion, will result in changes in T1ρ values.21 Changes in collagen content may also influence T1ρ values. Eventually, degenerated cartilage will show higher T1ρ values than normal (Fig. 6).