(1)
Department of Neurosurgery Faculty of Medicine, Saga University, Saga, Japan
Keywords
Midline suboccipital approachInfratentorial supracerebellar approachTransvermian approachTranscerebellomedullary fissure approachCerebellar hemispheric tumor6.1 Introduction
In this chapter, the basic techniques involved in the midline suboccipital approach and its variations are explained, focusing on intracranial lesion exposure, patient positioning, and bony opening sites. The midline suboccipital approach varies from case to case: the range of bony openings is altered up and down or left and right, depending on the lesion location. To approach lesions in the fourth ventricle and cerebellar hemisphere accurately, exposure of the vermian and/or cerebellar hemispheric surfaces must be considered when selecting patient positioning and bony opening site [13, 15]. Furthermore, preoperative interpretation of lesion location is vital [6, 10].
To optimize the operative field, the direction of sight through the operative microscope is important when positioning a patient. The relationship between patient position and the standing position of the surgeon should also be carefully considered in each case [3, 15]. Particularly, when using the transcerebellomedullary fissure (trans-CMF) approach with opening of the cerebellomedullary fissure (CMF), the standing position of the surgeon and the degree of forward flexion of the patient’s head in the prone or lateral recumbent position are crucial [11, 13, 14].
As surgery for a fourth ventricular lesion using the trans-CMF approach is described in Chap. 7: “Microsurgical Anatomy of the Cerebellomedullary Fissure and Variations of the Transcerebellomedullary Fissure Approach,” only surgeries for cerebellar hemispheric lesions are described in this chapter.
6.2 Relationship Between Lesion Location and Approach
The midline suboccipital approach is widely used, both for lesions in the vermis, suboccipital (posterior) cerebellar hemispheres, fourth ventricle, and dorsal surfaces of the medulla oblongata and pons and for lesions in the superior cerebellar hemisphere, the dorsal brainstem near the tentorial edge, and near the pineal gland [13, 18].
When considering this approach in the midline, it is possible to expose an operative field from the confluence of sinuses to the medulla oblongata. The midline suboccipital approach is further divided into three approaches, based on lesion height (Fig. 6.1a):
Fig. 6.1
Three variations of the midline suboccipital approach. (a) The midline suboccipital approach is divided into three variations, depending on the height of the approach. Arrow A indicates the infratentorial supracerebellar approach; Arrow B indicates the transvermian approach; and Arrow C indicates the trans-CMF approach (from Matsushima T et al. [13] with permission). (b) Transvermian approach for the removal of tumors originating from the vermis, such as medulloblastoma (from Matsushima T [4] with permission). (c) Trans-CMF approach for the removal of tumors originating from the floor of the fourth ventricle, such as ependymoma (from Matsushima T [4] with permission)
The infratentorial supracerebellar approach to the tentorial (superior) cerebellar surface and superior cerebellar vermis
The transvermian approach toward lesions in the inferior cerebellar hemisphere and/or vermis, through an incision in the inferior cerebellar vermis
The transvermian approach is a conventional approach widely used to remove tumors such as medulloblastoma [18]. The trans-CMF approach has been used for cavernoma in the fourth ventricular floor, ependymoma in the fourth ventricle, intraventricular hemangioblastoma, and choroid plexus papilloma [1, 6, 7, 9, 11]. Even in medulloblastoma originating from the fourth ventricle roof, the incision of the inferior vermis during tumor removal can be reduced by CMF opening. In fourth ventricular tumors with lateral extension into the cerebellomedullary cistern, when the bony opening is extended laterally and the lateral portion of the CMF is opened, the tumor around the lateral recess can be removed through the trans-CMF approach after midline suboccipital craniotomy [7, 9, 11].
Bony opening sites should be altered depending on the depth and/or lateral extension of cerebellar hemispheric lesions. At the end of this chapter, several example cases are presented featuring cerebellar hemispheric lesions.
Surgeons must preoperatively anticipate precise intraoperative images when determining the position, skin incision, and bony opening site. They should imagine what structures will be visible immediately after opening the dura mater and which neural structures should be opened or incised to reach lesions. Precise interpretation of preoperative images is crucial. Lesion location and origin and its relationship with surrounding structures—especially vasculature—must be investigated using magnetic resonance imaging (MRI) and magnetic resonance angiography. Lateral extension of lesions into the lateral recess and/or cerebellomedullary cistern should also be checked [6, 10, 15]. Consequently, the approach and bony opening site are naturally determined. When operative manipulation is required on the tentorial cerebellar surface, attention must be paid to bridging veins on the surface, tentorial sinuses, and the direction of inferior hemispheric veins on the suboccipital cerebellar hemisphere.
6.3 Midline Suboccipital Approach Procedures
6.3.1 Positioning
We perform the midline suboccipital approach in the Concorde or lateral recumbent positions (Fig. 6.2a, b) [3]. Although the sitting position confers the advantage of a bloodless operative field through drainage of blood downwards, we do not use it because of the risk of air embolism, which may develop into serious complications.
Fig. 6.2
Positioning of the patient in the prone position for the midline suboccipital approach. (a) Illustration showing tilting of the patient’s head and surgeon’s direction of sight through the microscope (from Matsushima T et al. [14] with permission). (b) Illustration showing the Concorde position (from Matsushima T et al. [14] with permission). (c, d) Illustrations showing the relationships between surgeon’s sitting position and direction of sight through the microscope (from Matsushima T et al. [14] with permission). (e, f) Photographs of the prone position. The patient’s head is tilted and the shoulder on the surgeon’s sitting side is retracted
The surgeon performs the midline suboccipital approach standing behind or sitting on the posterolateral side of the patient, facilitating observation of the suboccipital (posterior) cerebellar surface from the posterior side (Fig. 6.2c–f). This position offers a wide operative field and easy anatomical orientation of the suboccipital cerebellar hemisphere. It also offers easy observation of the superior cerebellar hemisphere, through the infratentorial subdural space, and the fourth ventricle, through the trans-CMF approach (where the CMF is opened instead of incising the inferior vermis). Particularly, when the tentorial cerebellar surface under the tentorium or fourth ventricular floor is observed through the CMF, the patient’s head should be tilted forward, and the chin pulled to its maximum extent, so that the tracheal tube and internal jugular vein are not excessively compressed (Fig. 6.2b). The degree of head tilting can be checked by the number of fingers inserted between the chin and chest: the maximum tilting should be about two fingers’ width. When the chin is insufficiently pulled, it is difficult to obtain the appropriate surgical field; however, excessive pulling of the chin causes postoperative laryngeal edema. The patient’s head may also be rotated a little so that the surgeon can examine the suboccipital surface face-to-face (Fig. 6.2f).
When performing the midline suboccipital approach in the prone position, a right-handed surgeon usually stands on the patient’s left side (Fig. 6.2c). However, when a tumor extends to the left lateral portion of the fourth ventricle or the surgeon is left-handed, it is better to stand on the patient’s right side (Fig. 6.2d). As the direction of sight through the microscope is straight, it is easy for the surgeon to observe the opposite side of the fourth ventricle through the CMF [11, 13, 15].
6.3.2 Skin Incision
In the midline suboccipital approach, midline linear or unilateral horseshoe-shaped incisions are usually used. For a midline skin incision, the skin is incised from a few centimeters above the external occipital protuberance to the fourth–sixth cervical vertebrae. Attention should be paid to avoid a narrow operative field, e.g., with insufficient lower or lateral exposure. The confluence of sinuses and internal occipital protuberance should be examined on radiograms of the head and the top edge of the skin incision made based on their relationship with the external occipital protuberance. The internal occipital protuberance is usually present inferior to the external occipital protuberance. When a tumor extends downwards from the foramen magnum or the fourth ventricle must be observed from below through the CMF, laminectomy may be required additionally to craniotomy. As the purpose of laminectomy is to extend a midline incision of the dura mater downwards, partial laminectomy in the midline is also helpful in some cases.
For a unilateral horseshoe-shaped incision, a 4–5 cm lateral extension of the top of a midline straight skin incision is also useful. If necessary, the incision can be extended to the level of the mastoid process. These skin incisions are used for lesions in the unilateral cerebellar hemisphere, tumors extending from the fourth ventricle to the unilateral cerebellomedullary cistern, or for the transcondylar fossa approach [12].
6.3.3 Bony Openings and Windows and Operative Range
The shape and size of bone windows depends on the extent to which the suboccipital cerebellar surface, medulla oblongata, and foramen magnum must be exposed for the surgical treatment of a lesion. Bony openings are related to lesion location, with or without lateral extension, and to the selected approach to that lesion. The upper limit of a bony opening is the transverse sinus, which must be exposed when the superior vermis and/or tentorial cerebellar surface are approached as per Craniotomy A in Fig. 6.3. When a lesion is supplied from the ventral side by superior cerebellar artery (SCA), it is preferable also to expose the lateral side to reveal SCA feeding the lesion. In such cases, the upper margin of the bone window should be longer along the transverse sinus. The lower limit of the bony opening depends on how much of the spinal canal must be exposed for the surgical treatment of a lesion with an inferior extension. The inferior margin of lesions must be exposed (Fig. 6.3a, b).
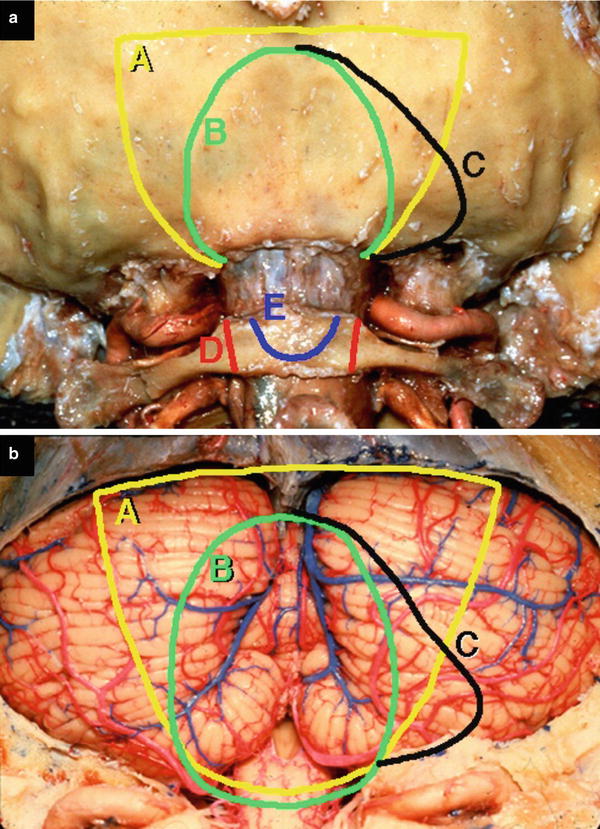
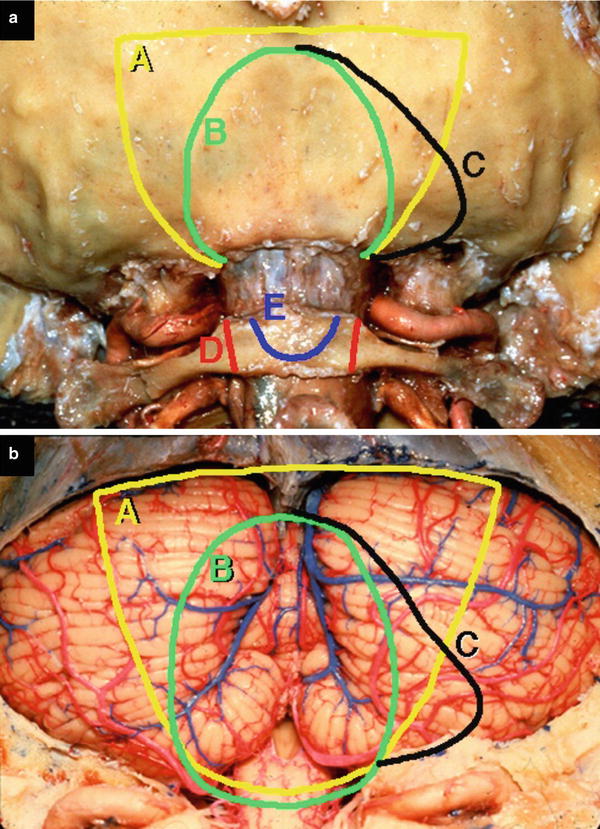
Fig. 6.3
Bony opening and the exposed cerebellar vermis and hemisphere (from Matsushima T et al. [13] with permission). (a) Bony openings for each variation. Circle A indicates an opening for the infratentorial supracerebellar approach; Circle B indicates an opening for the transvermian and trans-CMF approaches; Circle C demonstrates a bony opening for a lesion with lateral extension; Circle D indicates C1 laminectomy; and Circle E indicates partial laminectomy. (b) Exposed neural structure for each bony opening of circle A, B, and C
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree