(1)
Department of Neurosurgery Faculty of Medicine, Saga University, Saga, Japan
Keywords
Jugular foramenLateral suboccipital approachTransjugular process approachInfralabyrinthine approachGardner’s approachTransjugular approachJugular foramen schwannoma20.1 Introduction
The jugular foramen (JF) is formed by the temporal and occipital bones. It is located inferomedial to the temporal bone, inferior to the internal auditory canal (IAC), lateral to the jugular tubercle, and anterosuperior to the jugular process [13, 14, 18, 31]. The jugular bulb, which connects the sigmoid sinus to the internal jugular vein, is situated in the JF, and the lower cranial nerves (CNs) pass through it. In addition, the meningeal branches of the ascending pharyngeal artery pass through the JF to enter the posterior cranial fossa after ascending between the internal carotid artery (ICA) and internal jugular vein. Because the JF opens on the intra- and extracranial sides, most tumors of the JF grow in these two directions [4, 12, 17, 24, 25, 32, 42, 43].
The JF is one of the most difficult areas to understand and approach because of its complicated anatomy. Surgical access is complicated by surrounding structures, including the temporal bone, atlanto-occipital (A-O) joint, vertebral artery (VA), sigmoid sinus, internal jugular vein, CN VII, and lower CNs. A comprehensive understanding of the microsurgical anatomy and radiological findings of the JF and its surrounding structures is crucial to select the most appropriate surgical approach in each case [13–15, 19, 25, 40].
Hakuba A et al. first reported on skull base surgery for tumors of the JF [9, 10]. Since then, many different approaches to the JF have been reported [3–8, 20, 24, 29, 30, 35, 37, 39, 43]. It is challenging to understand them and their differences because of the complexity of the anatomy and their names. Moreover, some of them are very similar and some are a combined approach.
First, we will explain the basic anatomy of the JF, including the bony, nervous, and venous structures. Second, we will describe the various surgical approaches to the JF.
20.2 Basic Anatomy
20.2.1 Bony Structure
The JF can be regarded as a hiatus between the temporal and occipital bones; its shape is irregular and complex (Fig. 20.1a–c) [13, 14, 31]. Its anterolateral wall is formed by the temporal bone and posteromedial wall by the occipital bone, particularly the jugular tubercle. The posterior wall, which is the inferior edge of the sigmoid sinus, is formed by the jugular process of the occipital bone (Fig. 20.1b, c). The JF is situated between the petroclival fissure and occipitomastoid suture. The petroclival fissure lies between the lateral edge of the clival part of the occipital bone and the posteromedial edge of the petrous part of the temporal bone, and it intersects the anteromedial edge of the JF. The occipitomastoid suture—the suture between the mastoid part of the temporal bone and condylar part of the occipital bone—intersects its posterolateral edge. When viewed from the intracranial side, the JF appears to be gourd-shaped. The JF is separated into two components, petrosal and sigmoid, by the intrajugular process of the temporal bone and, occasionally, smaller opposite processes of the occipital bone (Fig. 20.1a). The small anteromedial part is the petrosal part (pars nervosa), which connects with the groove of the inferior petrosal sinus, and the large posterolateral part is the sigmoid part (pars venosa), which connects with the sigmoid sulcus. The anterolateral wall of the petrosal part consists of the pyramidal fossa, and the cochlear canaliculus opens into it from the bony labyrinth. The sigmoid part is large and ovoid and is occupied with the jugular bulb, which receives blood from the sigmoid sinus and posterior condylar emissary vein. When viewed from the extracranial posterior side, the jugular process between the occipital condyle and mastoid process forms the posterior wall of the JF. Because the JF is located anterolateral to the condyle, it is possible to reach its posterior wall from the posterolateral side by following the posterior condylar canal anterolaterally (Fig. 20.1c, d). The transverse process of C1 and the extracranial VA are obstacles in this direction. The mastoid canaliculus on the lateral wall of the sigmoid part and the tympanic canaliculus on the carotid ridge—the ridge between the carotid canal and JF—can be observed. The mastoid canaliculus travels the tympanomastoid suture, opening on the lateral surface of the temporal bone posterior to the external auditory canal, and the auricular branch (Arnold’s nerve) of CN X courses through it (Fig. 20.1b). The tympanic canaliculus is connected to the tympanic cavity, and the tympanic branch (Jacobson’s nerve), arising from the inferior glossopharyngeal ganglion of CN IX, courses through it.
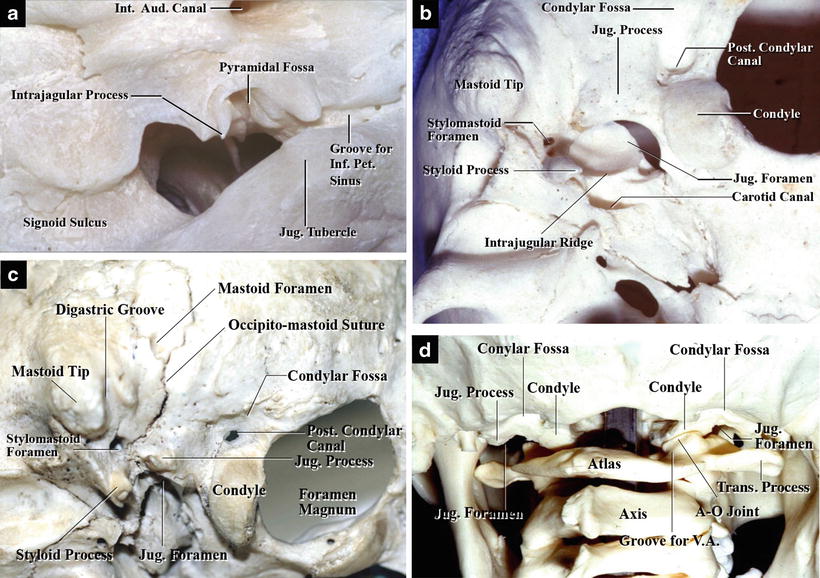
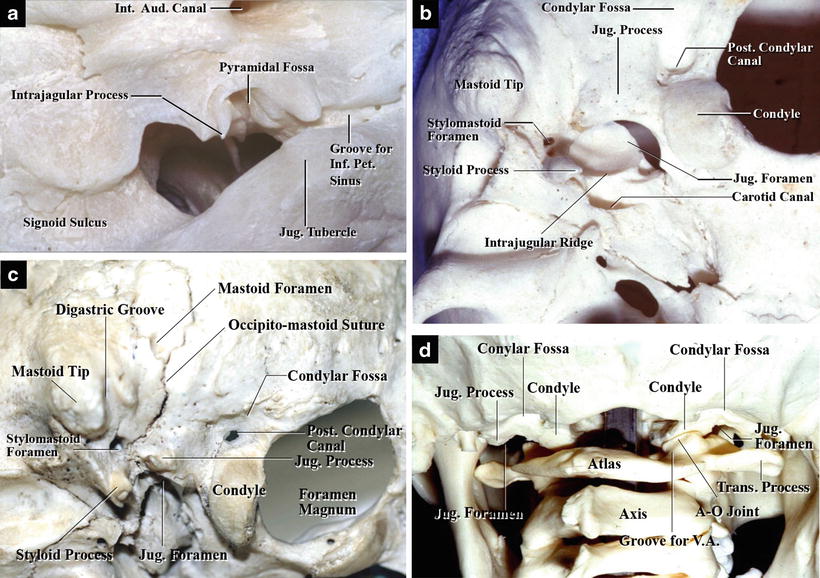
Fig. 20.1
Bony structure of the jugular foramen (JF); left side. (a) Internal view of the left JF. The left JF is observed from the superomedial side. The JF is formed by the temporal and occipital bones. The intrajugular process divides the JF into two compartments (from Katsuta T et al. [13] with permission). (b) External view of the left JF. The left JF is seen from the inferior side. It is located between the styloid process and the condyle. The intrajugular ridge, which divides the JF into the petrosal and sigmoid parts, is visible. The jugular process, which exists between the condyle and the mastoid process, forms the posterior edge of the JF (from Matsushima T [23] with permission). (c) Inferolateral view of the left skull base composed of the temporal and occipital bones. The left condyle, mastoid tip, digastric groove, and left styloid process are visible. The occipitomastoid suture runs between the digastric groove and the jugular process. The JF is behind the jugular process (from Matsushima T [23] with permission). (d) Posterior view of the craniocervical junction. The condyles and condylar fossae are situated at the lateral portions of the foramen magnum. The jugular processes, which form the posterior edges of the JF, are visible lateral to them (from Matsushima T [23] with permission)
20.2.2 Lower Cranial Nerves
The lower CNs pass through the JF, and CN XII passes through the hypoglossal canal located just below the JF (Fig. 20.2a). The JF, when viewed from the intracranial side, is covered by the dura mater, and the lower CNs pass through the dura mater. The lower CN bundles are separated by a dural septum, and CN IX and the CNs X and XI bundles usually pass anterosuperior and posteroinferior to the septum, respectively (Fig. 20.2b). The jugular dural folds (glossopharyngeal and vagal dural folds) are lateral to the nerves. After removing the dura mater, the sigmoid and inferior petrosal sinuses are exposed, and the intrajugular processes of the temporal and occipital bones can be identified. The JF is separated into the petrosal and the sigmoid parts by the intrajugular processes and a fibrous bridge called the intrajugular septum. All lower CNs pass through the petrosal part at the intracranial orifice. The lower CN bundles running in the JF can be seen through the thin anterior wall of the jugular bulb, which is situated in the sigmoid part (Fig. 20.2c).
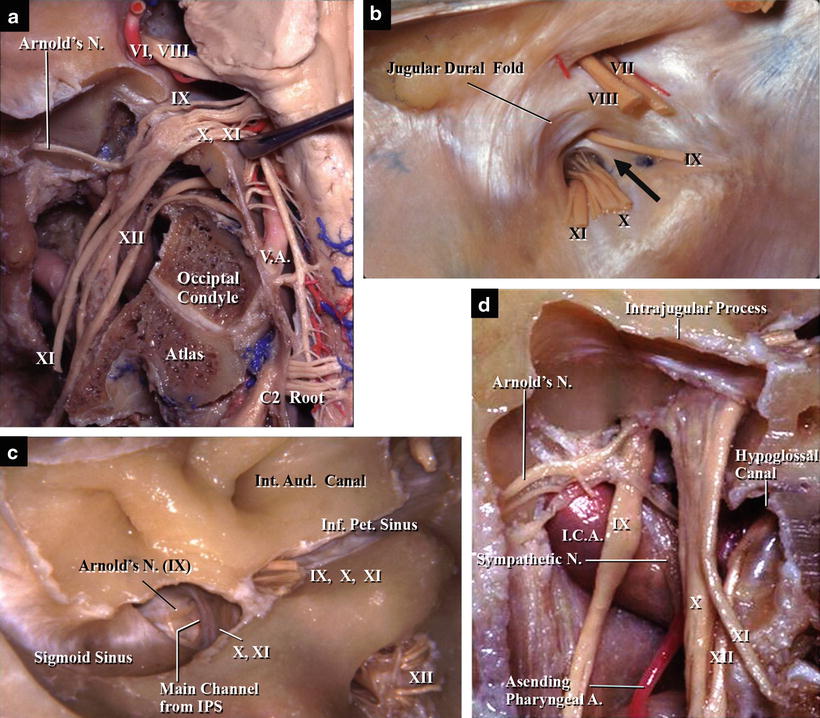
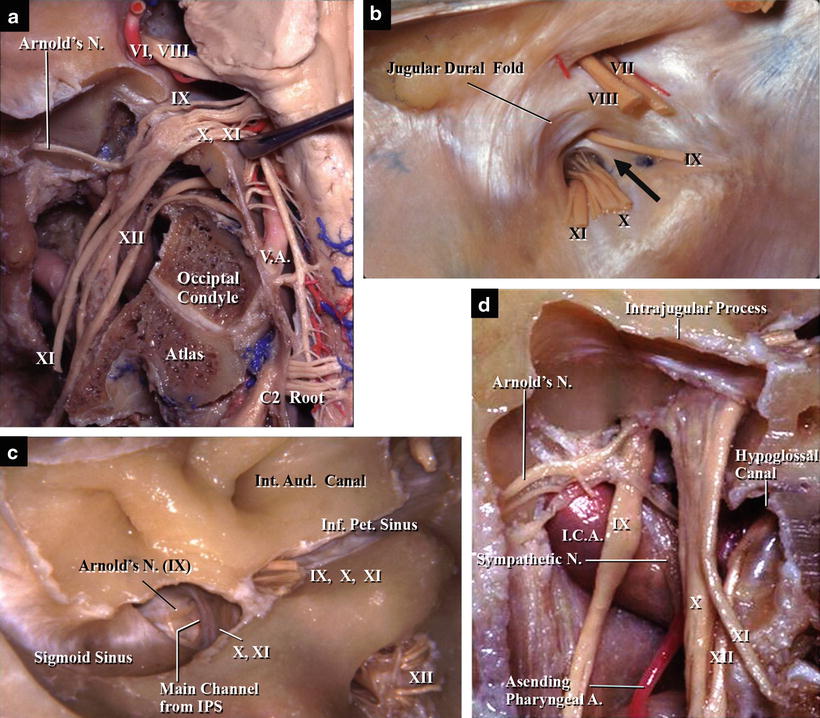
Fig. 20.2
The lower cranial nerves (CNs) and the jugular foramen (JF); left side (from Katsura T et al. [13] with permission). (a) Posterior view of the left JF after removal of the posterior wall. The sigmoid sinus and jugular bulb have been removed, exposing the lower CNs in the JF. They pass through the JF, and the hypoglossal nerve passes through the hypoglossal canal. (b) Intracranial view of the left JF with the dura mater intact. The JF is divided into two parts by a dural septum (arrow). CN IX and the CN X and XI bundles are situated in the anterior and posterior parts, respectively. The jugular dural fold is lateral to the nerves. (c) Intracranial view of the left JF with the dura mater removed. CNs IX–XI are located in the same compartment as the petrosal part at the intracranial orifice of the foramen. The nerve bundles in the JF can be seen through the thin wall of the jugular bulb. (d) Intraforaminal posterior view of the left JF with the anteromedial wall removed. The JF has been cut and the anteromedial wall of the JF has been removed to reveal its interior. The lower CNs, internal carotid artery, ascending pharyngeal artery, and sympathetic trunk are exposed. CN IX is located anterior to the intrajugular process at all levels in the JF. The CN X and XI bundles are also situated anterior to the intrajugular process at the intracranial orifice of the JF; however, they merge into the jugular bulb as they pass downward
Removing the jugular bulb wall exposes the intraforaminal portions of the lower CNs, sympathetic trunk, ICA, and ascending pharyngeal arteries (Fig. 20.2d). CN IX descends apart from and anterior to CNs X and XI. After passing through the JF with CN XI, CN X descends with CN XII. CN XI diverges from CN X outside the JF. The lower CNs descend near the internal jugular vein, and CN XI often descends entwined around the internal jugular vein (Fig. 20.3a, b).
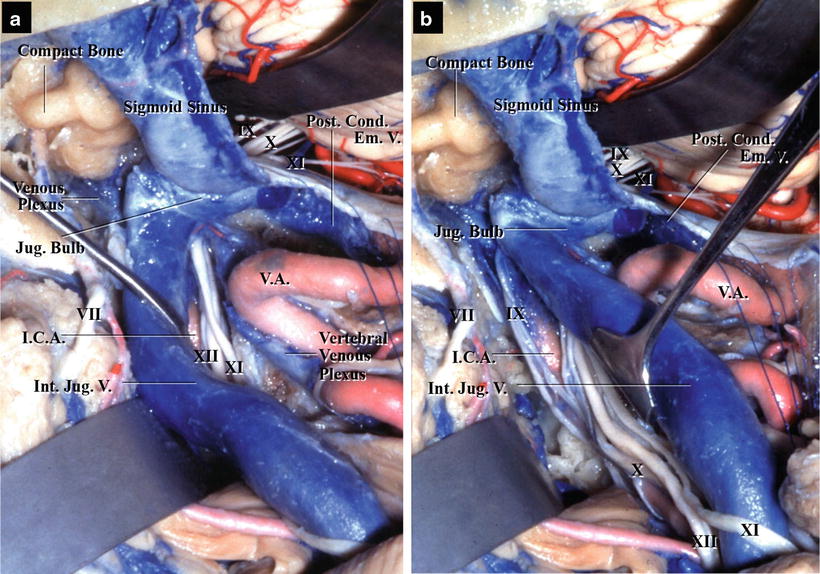
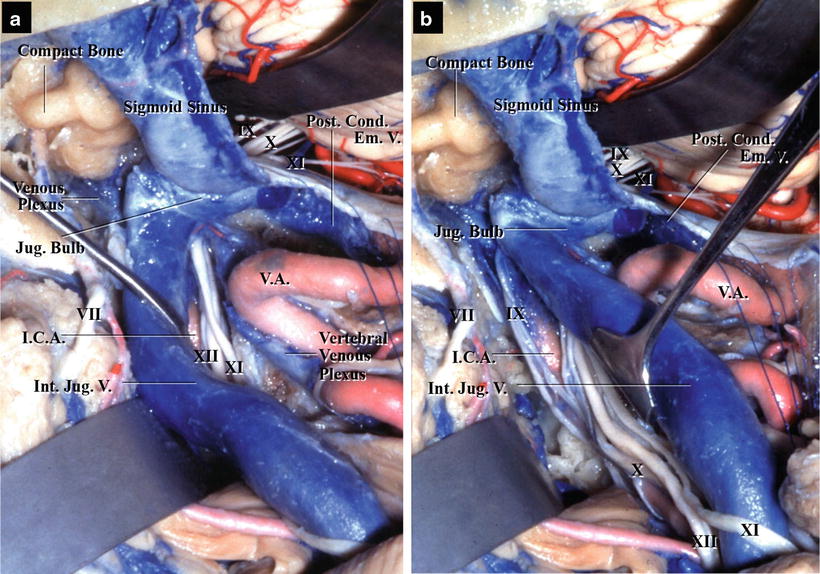
Fig. 20.3
The internal jugular vein and cranial nerves (CNs); left side (from Matsushima T [23] with permission). (a) Posterolateral view of the entire venous system on the left side after complete bony removal. The entire venous system, from the left sigmoid sinus to the left internal jugular vein, is exposed. The loop of the left vertebral artery is also visible after removal of the transverse process of C1. The internal jugular vein is retracted anterolaterally. CNs XI and XII run anteromedial to the upper part of the internal jugular vein. (b) The same view. The internal jugular vein is retracted posteromedially. CNs XI and XII, running anteromedial to the upper part of the internal jugular vein, pass behind the vein, whereas CN XI courses posterior to the lower part of the vein
20.2.3 Venous System
The jugular bulb in the JF communicates with several venous systems with both intracranial and extracranial sources, such as the inferior petrosal sinus, inferior petroclival vein, sigmoid sinus, venous plexus of the hypoglossal canal (anterior condylar emissary vein), and posterior condylar emissary vein, finally draining into the internal jugular vein. It is important to understand the venous system to select the appropriate surgical approach to the JF (Fig. 20.4). The inferior petrosal sinus courses on the intracranial side of the petroclival fissure. The sinus drains into the petrosal confluence in the petrosal part and connects with the jugular bulb through a main channel and several smaller channels. The venous plexus of the hypoglossal canal from the marginal sinus and the inferior petroclival vein on the extracranial surface of the petroclival fissure also drain into the jugular bulb after joining the petrosal confluence (Fig. 20.5). The main channel, which is 2–3 mm in diameter, is located between CN IX and the nerve bundles of CNs X and XI. The other channels are usually smaller than 1 mm. The sigmoid sinus is the largest vein draining into the jugular bulb, and the posterior condylar emissary vein is often connected with the junction between the sigmoid sinus and the jugular bulb (Figs. 20.3, 20.4, 20.5, and 20.6c, d).
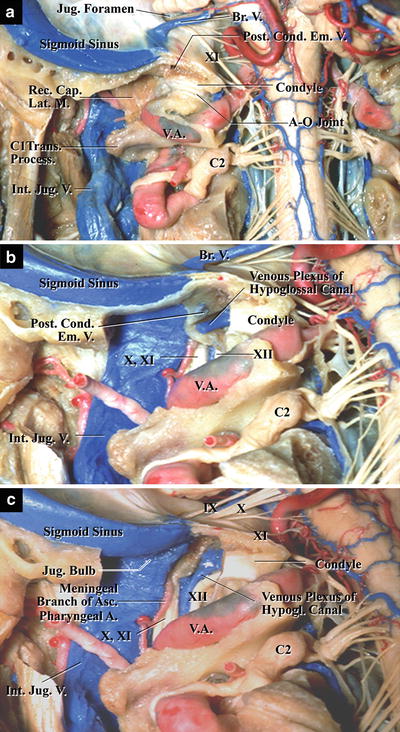
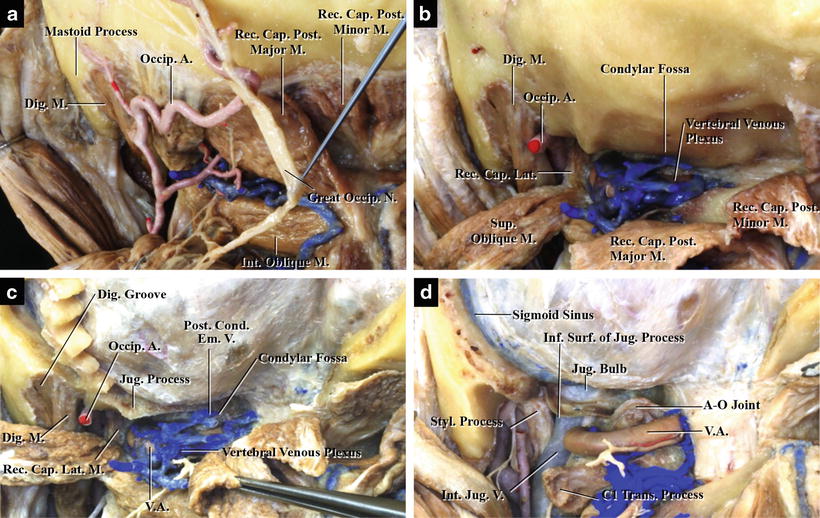
Fig. 20.4
Schematic illustration of the venous system around the jugular foramen; left side, superior view (from Matsushima K et al. [21] with permission). The sigmoid and inferior petrosal sinuses drain into the jugular bulb and petrosal confluence, respectively, in the jugular foramen. The marginal sinus connects with the petrosal confluence through the venous plexus of the hypoglossal canal, and the vertebral venous plexus connects with the inferior end of the sigmoid sinus through the posterior condylar emissary vein. The lateral condylar vein communicates between the petrosal confluence and the vertebral venous plexus
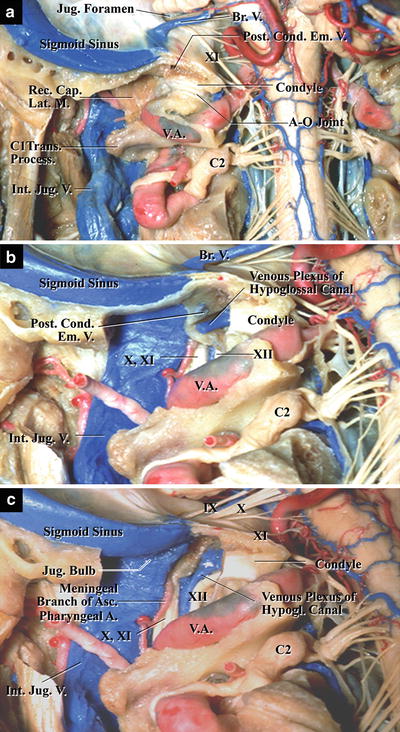
Fig. 20.5
The venous system connecting with the jugular bulb near the lateral craniocervical junction; left side, posterior view. The posterior belly of the digastric muscle has been detached and the jugular process and occipital condyle of the occipital bone have partially been removed to expose the jugular bulb in the jugular foramen (from Matsushima T [23] with permission). (a) The almost intact occipital condyle and the rectus capitis lateralis muscle. The atlanto-occipital joint is exposed after removal of the digastric muscle, but the jugular bulb is not yet exposed. It is hidden by the rectus capitis lateralis muscle, which extends from the transverse process of the C1 to the jugular process of the occipital bone. The posterior condylar emissary vein runs to the inferior end of the sigmoid sinus in the posterior part of the jugular tubercle. (b) Removal of the rectus capitis lateralis muscle and the lateral part of the occipital condyle. The rectus capitis lateralis muscle has been detached and removed, and the condyle partially removed. The origin of the internal jugular vein and venous plexus of the hypoglossal canal is exposed. (c) Removal of the jugular process and lateral part of the condyle. The jugular process and the lateral part of the condyle have been completely removed, exposing the jugular bulb
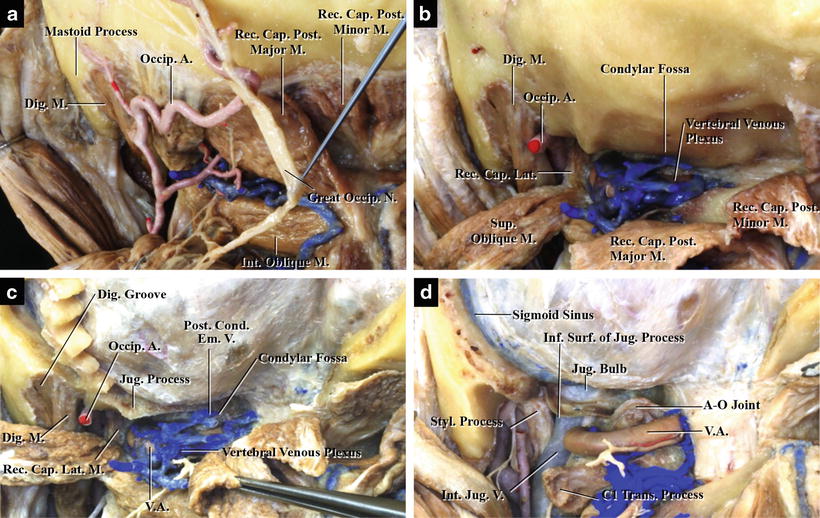
Fig. 20.6
The jugular process and surrounding area, demonstrating its relationship with the jugular foramen (JF); left side, posterior view. (a) The paracondylar region after removal of the first and second layers of the nuchal muscles. The digastric muscle and occipital artery are visible in the digastric groove. The superior and inferior oblique and rectus capitis posterior major muscles are not yet detached. The vertebral venous plexus is partially visible in the suboccipital triangle. (b) The paracondylar region after detaching the superior oblique and rectus capitis posterior major muscles. The superior oblique and rectus capitis posterior major and minor muscles have been detached and reflected, and then the vertebral venous plexus, VA, and rectus capitis lateralis muscle are exposed in the paracondylar region. (c) The condylar fossa and the posterior condylar emissary vein after the suboccipital retrosigmoid craniotomy. The suboccipital craniotomy has been performed. The posterior condylar emissary vein is exposed in the condylar fossa. The rectus capitis lateralis muscle attaching to the jugular process can be seen lateral to the condyle and condylar fossa. The jugular process forms the posterior wall of the JF. (d) Exposure of the jugular bulb after complete removal of the jugular process and partial removal of the occipital condyle. The jugular process, the posterior wall of the JF, has been completely removed, exposing the sigmoid sinus, jugular bulb, and internal jugular vein. The vertebral venous plexus has also been removed, and VA and the atlanto-occipital joint are exposed
20.2.4 Relationship Between the Jugular Foramen and the Lateral Foramen Magnum
When the posterior wall of the JF is approached from the posterolateral side or after the lateral foramen magnum approach, it is important to understand the anatomy of the region lateral to the lateral foramen magnum: the area between the condyle and condylar fossa and the mastoid process and digastric groove (Fig. 20.6). The JF lies lateral to the jugular tubercle and anterior to the jugular process. The posterior condylar canal, containing the posterior condylar emissary vein, courses from the condylar fossa to the posteromedial part of the junction between the sigmoid sulcus and JF. Removing the posterolateral part of the condyle and jugular process by following the posterior condylar canal opens the posterior wall of the JF (Figs. 20.5 and 20.6c, d) [21]. The digastric groove, transverse process of C1, and posterior condylar canal comprise useful intraoperative landmarks during procedures in this region. The rectus capitis lateralis muscle is attached from the transverse process of C1 to the jugular process and covers the origin of the internal jugular vein and lower CNs (Fig. 20.6c, d). The extracranial part of VA sometimes forms an obstacle and, consequently, working space between the suboccipital surface of the occipital bone and VA is too narrow. In such cases, transposition of the extracranial VA is required after opening the transverse foramen of C1.
20.3 Characteristics of and Surgical Approaches to Jugular Foramen Tumors
20.3.1 Characteristic Growing Directions and Locations of Jugular Foramen Tumors and Their Classification
Most tumors of the JF, e.g., schwannoma, meningioma, and glomus jugulare tumor, are often located both intra- and extracranially (Fig. 20.7a) [17, 25, 32, 40, 42]. Because neurosurgeons have greater opportunities to surgically treat schwannomas than other tumors of the JF, we will explain the surgical approaches to the JF using JF schwannomas as an example. Based on the three growth patterns of schwannomas, Kaye AH et al. classified schwannomas of the JF into three types:
Fig. 20.7
Three different locations of the main mass of jugular foramen (JF) neurinomas and their classification. (a) Magnetic resonance imaging and computed tomography scanning in three patients demonstrating three different locations of the main mass of JF neurinomas. In one patient with a neurinoma predominantly on the left side, its main mass was in the intracranial region; in a second with a central neurinoma, a dumbbell-shaped mass existed in the temporal bone; and in a third with a neurinoma predominantly on the right side, the main mass was in the extracranial region. (b) Schematic illustration demonstrating Kaye’s classification based on the location of the main mass of JF neurinomas (from Matsushima T et al. [26] with permission)
Kaye’s classification logically considers the location of a schwannoma in each case, but many tumors cannot be simply classified as one of Kaye’s three types. Pellet et al. added another type:
Type D: dumbbell-shaped tumors with both intra- and extracranial components [30]
From the viewpoint of preoperative planning of the optimal surgical approach, Bulsara et al. proposed another modified grading scale:
Type A: intradural tumors
Type B: dumbbell-shaped tumors
Type C: triple dumbbell tumors, with a high cervical extension to guide surgical management [4]
These classifications are useful when considering the appropriate surgical approach in each case. Because no surgical approach can expose all sides of the JF at once, the most appropriate approach or combination of approaches should be selected based on the tumor’s anatomical location in each case.
20.3.2 Four Basic Approaches to the Jugular Foramen and Approaches Previously Reported
When we approach the JF, we should consider the following four basic approaches, based on an approaching direction and an opened area of the skull: (I) posterior approach; (II) posterolateral approach; (III) superolateral approach; and (IV) inferolateral approach (Table 20.1; Fig. 20.8) [23]. The surgical approaches previously reported can be classified as one or combinations of these basic approaches.
Table 20.1
Four basic approaches
(I) Posterior approach | For example, lateral suboccipital retrosigmoid approach |
(II) Posterolateral approach | For example, transjugular process–transcondylar approach |
(III) Superolateral approach | For example, infralabyrinthine approach |
(IV) Inferolateral approach | For example, superior cervical dissection with or without mastoidectomy |
(V) Combined approach | Combination of some of the four basic approaches |
Fig. 20.8
Four different basic surgical approaches to the jugular foramen (JF); left side, posterolateral view. (a) The external surface of the skull and JF. The posterolateral part of the skull is composed of the occipital and temporal bones. The mastoid process, condyle, and occipitomastoid suture are visible. The dotted lines indicate the course of the sigmoid sinus, and the jugular process between the mastoid tip and the condyle forms the posterior wall of the JF. (b) Relationships between the four basic surgical approaches and their bony opening areas. Four different bony openings are shown on the occipital and temporal bones. The green-colored area shows the bony opening for posterior approaches such as the lateral suboccipital retrosigmoid approach; the blue-colored area shows the bony opening for posterolateral approach such as the transjugular process–transcondylar approach; the pink-colored area shows the bony opening for superolateral approach such as the infralabyrinthine approach; and the yellow-colored area shows the bony opening for inferolateral approach such as mastoidectomy of the tip of the mastoid bone. The bony opening for each approach overlaps. (c) The venous system related to the JF. The sigmoid sinus, jugular bulb, and internal jugular vein are completely exposed after removal of the muscles and bones and complete mastoidectomy. (d) Schematic drawings showing the four basic surgical approaches to the JF. A green arrow indicates the posterior approach, a blue arrow indicates the posterolateral approach, a pink arrow indicates the superolateral approach, and a yellow arrow indicates the inferolateral approach
The posterior (I) approach includes the lateral suboccipital retrosigmoid approach, through which the intracranial orifice of the JF and the intraforaminal surface are exposed from the intracranial side. The far-lateral and transcondylar approaches also belong to this group [2, 11




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








