CHAPTER 23 Metal-on-Metal Hip Resurfacing Arthroplasty
KEY POINTS
 Removal of osteophytes from the femoral head-neck region is critical for sizing and seating of the femoral component.
Removal of osteophytes from the femoral head-neck region is critical for sizing and seating of the femoral component. The femoral component should be placed in 5 to 10 degrees of valgus to the femoral neck-shaft angle. Care must be taken to avoid femoral notching.
The femoral component should be placed in 5 to 10 degrees of valgus to the femoral neck-shaft angle. Care must be taken to avoid femoral notching. Femoral-acetabular mismatches can occur and should be identified preoperatively to ensure appropriate component selection and sizing.
Femoral-acetabular mismatches can occur and should be identified preoperatively to ensure appropriate component selection and sizing.Resurfacing arthroplasty has experienced resurgence in popularity over the past decade. With improvement in design technology and metallurgy, many of the problems that plagued early designs have been overcome. The initial high failure rates with earlier designs were largely attributed to the cemented acetabular component as well as the high polyethylene wear rate associated with the larger femoral head sizes.1–4
Current systems utilize a hybrid design, with a press-fit acetabular component and a cemented femoral component.5 Early and midterm results have been favorable and comparable to those of the traditional total hip arthroplasty, with survival rates of 97% to 99% at 4 to 5 years of follow-up.6–9 As long-term follow-up becomes available, the role of resurfacing arthroplasty in orthopedic hip reconstruction will become better defined. In this chapter we review the main indications for this hip implant as well as the surgical technique necessary to avoid short-term failures.
INDICATIONS AND CONTRAINDICATIONS
The absolute indications and contraindications for resurfacing arthroplasty are constantly evolving. The ideal candidate is younger than 55 years of age and functions, or wishes to function, at a high activity level.10 The underlying cause of disease has not been shown to affect outcome and should not be used as an exclusion criterion.8
Given the inability to substantially alter leg length or offset, it has been suggested that leg length discrepancy of greater than 2 cm and significant varus alignment of the proximal femur be considered relative contraindications to resurfacing.11,12 In addition, significant bone loss on the acetabular side may preclude achieving acceptable fixation and therefore should also be considered a relative contraindication. Femoral component loosening and stem subsidence have been associated with large cysts, female gender, and small component size in male gender.8,13,14
Beaulé and associates13 formulated the Surface Arthroplasty Risk Index (SARI) to provide a guideline for patient characteristics associated with early failure. It is based on a 6-point scoring system, with a score greater than 3 having a 89% survival at 4 years, compared with a 97% survival in patients with scores less than or equal to 3 (Table 23-1).8
TABLE 23-1 Surface Arthroplasty Risk Index
| Risk Factor | Points |
|---|---|
| Femoral head cyst >1 cm | 2 |
| Weight <82 kg | 2 |
| Previous hip surgery | 1 |
| UCLA activity score >6 | 1 |
Data from Beaulé PE, Dorey FJ, LeDuff MJ, et al: Risk factors affecting outcome of metal on metal surface arthroplasty of the hip. Clin Orthop Relat Res 418:87-93, 2004.
PREOPERATIVE PLANNING
Preoperative planning is essential to successful resurfacing arthroplasty with one of the reasons being that the femoral and acetabular components come as a matched pair. Preoperative templating utilizes an anteroposterior pelvic and cross-table lateral radiograph, with acetabular sizing being done first. This enables the surgeon to select the size that provides a good fit while minimizing the amount of bone resection on the acetabular side. With the acetabular size selected, one can then verify if the matched femoral component will be adequate for the patient’s anatomy (i.e., the femoral head-neck offset). In most patients the hip will be in an externally rotated position, giving the appearance of a diminished femoral offset as well as poorly defined femoral head-neck junction. The appropriately sized femoral component should abut the inferomedial femoral neck, leaving a 1- to 2-mm clearance at the superolateral head neck junction with a 5- to 10-degree valgus alignment of the femoral component in respect to the native femoral neck-shaft angle. It is essential to avoid notching the femoral neck both from a vascular and a mechanical standpoint.15,16 Patients with large osteophytes along the head and neck junction will require careful débridement to optimize the femoral head-neck offset and ensure proper orientation of the femoral component within the femoral neck.10,17
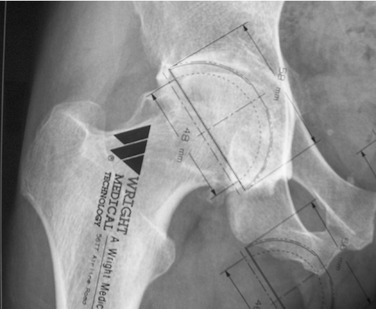
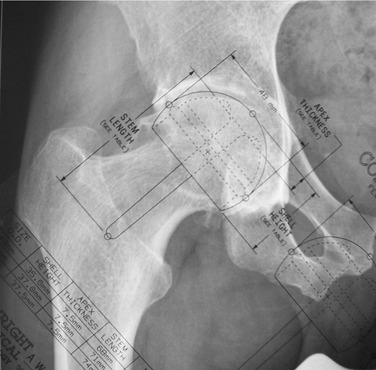
By sizing the acetabulum first, mismatches between the femoral neck and acetabulum can be identified appropriately. In 80% to 90% of cases a mismatch is not present. Therefore, the majority of cases can be started with femoral preparation. In a small portion of cases the acetabulum will be oversized relative to the femoral neck. This case may require the utilization of a thicker acetabular shell. Identification of this mismatch preoperatively ensures that the appropriate sized shells will be available. Figures 23-1 and 23-2 illustrate a case of femoral-acetabular mismatch. Figure 23-1 shows an acetabulum that templates to size 56. The standard thin-shelled acetabular component is 6 mm, corresponding to a femoral size of 50. Figure 23-2 shows the accompanying femoral templating. As illustrated, the femoral side templates to size 46, which would correspond to a size 52 thin-shelled acetabular component. The thicker shell acetabular component addresses this mismatch, allowing for a size 56-acetabular component and a size-46 femoral component.
TECHNIQUE
The majority of resurfacing arthroplasty is performed through a posterior approach. Concerns have been raised in regard to this approach because the main blood supply to the femoral head enters through the ascending branch of the medial circumflex artery along the posterolateral aspect of the femoral head, which is usually dissected during the posterior approach.15,18,19 In light of this risk, the senior author has chosen to perform the resurfacing arthroplasty through an anterior dislocation, in conjunction with a modified trochanteric slide osteotomy.20,21
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree