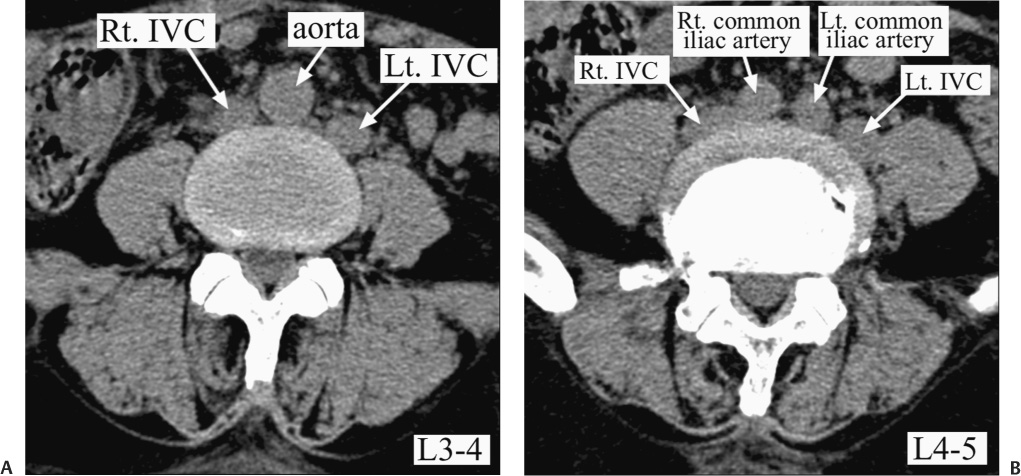
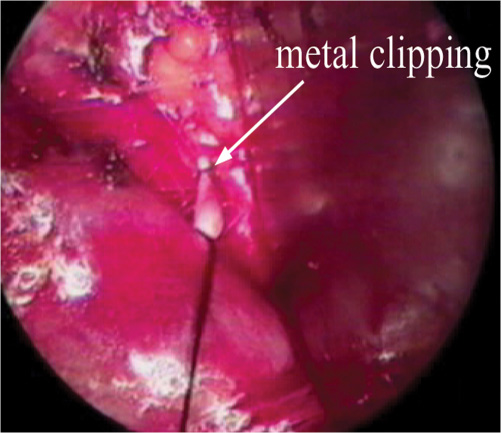
28 Peripheral Nerve Complications Wide exposure of the ventral disk space is necessary for good implant position and safety of instrumentation in relation to heavy and complex artificial disk instruments. Therefore, extensive vascular mobilization is inevitable, resulting in the fact that surgeons are confronted with the risk of vascular injury. However, most approach-related complications are avoidable when surgeons are more experienced. The surgical planes of properly selected patients are more easily separable due to less degenerative inflammatory change, as well the patients’ being relatively young and less obese compared with fusion patient cases.1 The authors’ collaborative professional surgical team, composed of vascular and general surgeons, has a great amount of surgical experience with the anterior retroperitoneal approach for spine surgery, with more than 1000 cases per year.2 We present our clinical experiences with complication-reducing techniques and the skill developed in the management of vascular and surgical-related complications, with a review of the literature. It is important to obtain information about the prevertebral vascular structure and its status. Preoperative computed tomographic (CT) scans and magnetic resonance (MR) axial images should contain not only spine pathology but the prevertebral vascular anatomy as well. Digitalized image-viewing systems are especially useful in understanding the three-dimensional relationship between the vascular structure and the ventral vertebral surface. Louis has described six primary variants of the aortocaval anatomy based on the level of the aortic split and vena cava bifurcation.3 In our experience, many unclassified vascular variations exist, including dual infrarenal inferior vena cava (IVC) and situs inversus (Fig. 28–1). Additionally, combinations of lumbar spine segment variants, lumbarization, or sacralization make it more complex. Such exact recognition of the vasculature at the targeted disk level helps to determine an apt approach plan (e.g., entrance between aortocaval bifurcation is better even at the L4–L5 level in some cases) and avoid encountering surprises, such as aortic aneurysm or the rare variations already mentioned. In cases of calcified atherosclerotic plaques, as noticed on CT scan, duplex Doppler ultrasound for lower extremity arterial blood flow can provide more meaningful information. If, due to atherosclerosis, any stenotic portion is noted on a lower-extremity duplex scan, an anterior retroperitoneal approach for total disk replacement (TDR) is contraindicated. Preoperative abdominal ultrasound checks are routinely performed to rule out urogenital, visceral anomaly, or an unexpected pathology, such as a congenital single kidney, ureter duplication, hidden abdominal solid organ malignancy, gynecological abnormalities, or abdominal aortic aneurysms. All these efforts may lead to decreases in vascular and other approach-related complications. In our clinical experience of TDR in 620 patients, the incidence of venous bleeding was 1.3% (eight cases), with tearing of the left common iliac vein being the most common during L4–L5 disk space exposure. Six cases sustained minor pinpoint bleeding caused by either an avulsion of small radicular branches hidden beneath perivascular soft tissue, containing lymphatics, or losing sight of a tethered perforating vein to the L5 body. Although it was possible to control such occurrences by compression with coagulants, we performed a simple suture with 5–0 Prolene to complete further vessel mobilization. At times, venous injury of the main trunk with large amounts of bleeding can occur due to the laceration of a misread collapsed vein under retraction of underlying soft tissue when the surgeon is less experienced. Therefore, the surgeon should dissect perivascular soft tissue with careful attention to the lateral margin of the venous trunk, especially under conditions of perivascular scarring and adherence caused by reactive inflammation at an osteophytic spur, degenerative changes of the spine, or prior abdominal surgery. Two cases of major venous injury occurred during artificial disk implantation (Table 28–1). One was caused by anesthetic complications; the abdominal pressure suddenly increased with ventilator fighting at the midterm of the ProDisc (Synthes, Inc., West Chester, PA) implantation at the L4–L5 level. The left iliac vein injury occurred during the temporary removal of the retractor system and artificial disk instruments. The other venous injury was caused by the SB Charité instruments (DePuy Spine, Raynham, MA); we had failed at secure retraction transiently because the patient had a heavy abdominal musculature and bulky psoas muscle. Therefore, some of my anesthesiologist colleagues prefer to implement continuous infusion of muscle relaxants during anterior retroperitoneal spine surgery. Figure 28–1 Unusual left infrarenal dual inferior vena cava (IVC). (A) Axial computed tomography (CT) scan showing the left-sided infrarenal dual inferior vena cava (IVC) at the L3–L4 level. (B) Axial CT scan showing the left-sided infrarenal dual IVC at the L4–L5 level. The iliolumbar vein can often be extremely troublesome for most surgeons. Special attention should be paid to this precarious structure early during its exposure. For wide exposure, enough for TDR, ligation of the ascending iliolumbar vein is necessary to prevent avulsion from the mother vessel. If iliolumbar vein injury occurs, it is impossible to control using direct compression alone or with direct suturing due to the large amount of bleeding and the narrow surgical field. In such situations, tentative clipping and cutting of the remnant vein followed by an elective suture and tie are more effective than blind cauterization or a direct suture (Fig. 28–2).
Management of Vascular and Surgical
Approach–Related Complications: Lumbar
Total Disk Replacement
 Preoperative Evaluation and Planning
Preoperative Evaluation and Planning
 Management of Vascular Complications
Management of Vascular Complications
 Other Approach-Related Complications
Other Approach-Related Complications
Preoperative Evaluation and Planning
Management of Vascular Complications
Venous Tear and Bleeding
Complications | Numbers* |
Major venous injury | 2 |
Arterial embolism | 1 |
Deep vein thrombosis | 0 |
Visceral complication | 0 |
Retrograde ejaculation | 0 |
Sympathetic nerve damage | 0 |
Anterior rectus facia defect | 2 |
Figure 28–2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Conclusion
Conclusion