Chapter 8 Management of the Tuberous Breast
Management of the tuberous breast represents perhaps the greatest challenge in all of aesthetic breast surgery as, in its most dramatic form, the preoperative deformity in breast shape can be significant. It is important to remember, however, that at times the condition can also be subtle and yet significantly impact in an adverse way the result obtained after aesthetic breast surgery. To avoid poor results in these types of patients, it is very important to recognize which elements of the deformity are present preoperatively and then develop a sound surgical plan designed effectively to correct the anatomic abnormalities that are present.
Clinical Presentation
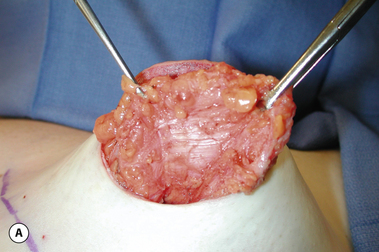
Typically, a fully involved tuberous breast deformity will include a superiorly malpositioned inframammary fold that appears high in relation to what would be considered a ‘normal’ breast position. Present along with this is usually a constricted lower pole skin envelope that is likewise tight and unexpanded. As a result, whatever breast parenchyma is present variably protrudes through the areola, creating a ‘pseudoherniation’. It appears as if the embryonic breast bud was restricted to a small area of the anterior chest wall with an abnormally absent peripheral expansion and, as the breast develops during puberty, it has nowhere to go as it grows except forward. Because the areolar dermis is more elastic than the surrounding breast skin, there is a preferential expansion through the areola, which leads to the herniated appearance (Figure 8.1). Anatomically, in severe tuberous breast cases, fibrous bands can be identified along the underside of the breast in association with the constricted breast base diameter (Figure 8.2 A). Once these bands are cut, the entire breast mound can be observed to expand, creating a more normal breast appearance (Figure 8.2 B). Currently, it is not known if these bands are responsible for the deformity or, conversely, are present as a result of the deformity. Either way, it is interesting to postulate what role these bands might have in the development of the condition.
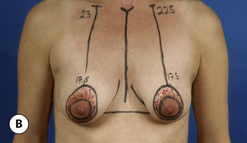
Further complicating the altered overall appearance of the breast is the fact that asymmetry is a very common finding in patients with this condition. At times this asymmetry can be as dramatic a finding as the basic abnormality itself (Figure 8.3). It is not at all uncommon for one breast to present as a hypoplastic, misshapen mound that contrasts starkly with an enlarged, ptotic and disproportionate opposite breast with a nipple–areola complex (NAC) that appears to be medially translocated. Clearly, adequate surgical treatment must be geared toward artistically reshaping both breasts to maximal advantage in an attempt to restore symmetry.
Additionally, the tuberous breast deformity is not an all or none entity and, for any given patient, there can be varying degrees of involvement. As a result, the appearance of the breast can range from a subtle tightening of the inframammary fold all the way to the fully developed deformity with asymmetry as described previously (Figure 8.4). All of these factors combine to make treatment of the tuberous breast one of the most demanding surgical challenges in all of aesthetic breast surgery.
Surgical Strategies
Management of the Constricted Skin Envelope
It must be emphasized that, even in patients who demonstrate only a mild tendency toward a tuberous breast, the inframammary fold contour can create significant problems in breast shaping. This can become very important in a general breast augmentation practice as the subtly high and mildly tight inframammary fold can escape the notice of the surgeon, only to become a problem later at the time of surgery when the lower pole of the breast appears constricted or the previous fold fails to soften completely as a new and lower fold position is created. These types of patients can be recognized by carefully observing the nature of the medial inframammary fold crease. If there is any convexity or superiorly oriented curving of the medial lower pole contour, a mild tuberous breast can be diagnosed (Figure 8.5). Recognition of this deformity preoperatively can help prepare the surgeon for what is to come at the time of surgery and allow for appropriate preoperative technical planning to be done. Also, the patient can be advised ahead of time as to the nature of her deformity, which then allows reasonable expectations to be set.
Perhaps the most difficult determination that must be made by the surgeon is whether or not the constricted inferior pole skin can be expanded enough to allow the primary placement of a breast implant to create a natural contour in the lower pole of the breast. Also, it must be determined whether or not the crease created by the old inframammary fold (IMF) can be overcome by the implant once the new and more inferiorly located fold is created. This is a critical decision point in designing a successful operative strategy as, in fully developed tuberous breast cases, a persistent fold and a flattened and tight lower pole contour will very commonly persist despite aggressive release of the underlying soft tissue support structures. In these patients, better control of the lower pole and the location of the IMF can be afforded with the primary use of a tissue expander. In this fashion, the constricted skin envelope can be stretched sufficiently over time to allow the subsequent placement of an implant and any persistent crease in the old IMF can be softened. Deciding between the primary insertion of an implant versus the use of a staged tissue expander/implant strategy is the major determination that must be made when treating a patient with a tuberous breast deformity. This decision is complicated by other factors. To a certain extent, an old IMF crease that does not completely soften initially may subsequently relax over time due to the influence of the underlying implant. When this old fold will fill out and to what extent will be very patient dependent and is therefore subject to a significant degree of variability. As a result, an early persistent fold that can detract from the overall result after surgical correction may or may not improve over time and in no way can this be predicted with certainty. Added to this is the desire on the part of many patients to accomplish surgical correction in one operation. Besides the basic advantages of needing only one operation on traditional considerations such as operative risk, recovery and time off work, many patients have a financial incentive to effect correction in one stage. Unfortunately, insurance companies very commonly do not extend benefit coverage for tuberous breast correction and the procedure is considered cosmetic. As a result, a great many patients have financial constraints that allow only one procedure. All of this combines to place a fair amount of pressure on the surgeon to provide a one-stage correction.
To this end, several surgical strategies can be employed to maximally expand the skin of the lower pole and accurately lower the IMF. By placing the implant in the subglandular plane, direct force is applied to the skin of the lower pole and any tethering effect created by the pectoralis major muscle can be obviated. Also, by using the subglandular plane, the underside of the breast can be stretched and released as needed. As noted previously, there may be tethering fascial bands running horizontally along the underside of the breast. By radially scoring up into the parenchyma and dividing these bands, a visual and palpable release of the underside of the breast will be noted, resulting in a softer and more compliant breast mound. Taken together, these two maneuvers will allow the soft tissue envelope and the implant to better complement one another, resulting in a smooth and naturally contoured lower pole.