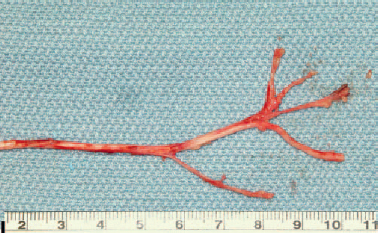
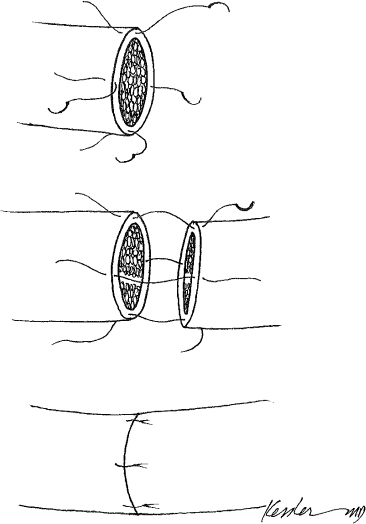
8 Facial paralysis may result from a variety of etiologies, including trauma, viral infection, neoplastic disease, and idiopathic causes. Although the approach to management of the paralyzed face is often predicated on the etiology of the paralysis and the expectations for recovery, this chapter focuses on the techniques commonly used for facial reanimation. Arguably, there are few deficits that impact a person’s self-image more than facial paralysis. The combination of aesthetic and functional impairments that result from a facial paralysis can be psychologically devastating, leading to depression and social isolation. In addition to the obvious aesthetic impact of a facial paralysis, the functional impairment can be significant. Incomplete eye closure can result in visual impairment, midface atony can result in impaired nasal breathing, and laxity of the lower face can result in deficits in speech and oral competence. Rehabilitation of the facial paralysis may be achieved through nerve regeneration, static reconstruction, or dynamic reconstruction. Determining the optimal approach for facial rehabilitation depends on the expectations for facial nerve regeneration and the goals and expectations of the patient. A careful patient assessment is important to determine the appropriate management of a patient with facial paralysis. Understanding the etiology of the injury is essential. This includes an understanding of the likelihood of nerve recovery. Once the degree of injury and the expectations for recovery have been determined, a detailed examination should be performed. The examination should assess the motion of the upper, middle, and lower thirds of the face independently. Beginning with the upper face, visual acuity, corneal integrity, eyelid closure, tearing, Bell’s phenomenon, lagophthalmos, lower lid tone, and brow position should be evaluated. The middle third entails a nasal examination, with a detailed evaluation of the nasolabial fold, nasal alar position, and the nasal airway. The lower third examination should assess the general tone of the lower third of the face with specific emphasis on oral competence, position of the lower lip, and the degree of depressor muscle dysfunction. In addition to the general assessment of facial dysfunction, the lower third evaluation requires a careful assessment of the smile pattern. Smile patterns were initially classified by Rubin1 in 1974 into three types. Type I is the most common smile pattern, occurring in almost two thirds of patients, and it is dominated by action of the zygomaticus major muscle. Type I smiles are characterized by the mouth moving laterally and superiorly, with subtle elevation of the upper lip. Type II, the canine smile, occurs in one third of patients and is dominated by levator labii superioris action, appearing as vertical elevation of the upper lip, followed by lateral elevation of the corner of the mouth. Type III occurs in a minority of patients and is the full denture smile, or “toothy smile,” produced by simultaneous contraction of the elevators and depressors of the lips and angles of the mouth. Noting the smile type is important because suspension techniques can be modified to accommodate the smile type. Before deciding on the approach to facial reanimation, several crucial factors should be defined. These include the timing of the injury, the degree of the injury, and the condition of the proximal and distal facial nerve. Electromyography (EMG) is recommended for all patients whose injuries occurred more than 12 months before presentation (Table 8.1). EMG demonstrates polyphasic or normal voluntary action potentials in those with active reinnervation. In these patients the presence of polyphasic potentials may mean that reinnervation is occurring and facial movement may return. Although temporizing surgical procedures may be warranted, reanimation surgery should not be performed. When the EMG demonstrates fibrillation or denervation potentials, the muscle is denervated, and in this situation cable nerve grafting is an option for management. In long-standing paralysis (more than 18 months), severe atrophy of the facial muscles occurs, limiting reinnervation techniques. EMG is helpful in determining the degree of facial muscle atrophy. When muscle atrophy has occurred, the EMG may demonstrate “electrical silence,” consistent with complete denervation atrophy of the facial muscles. In these cases, nerve grafting or nerve transfer is not indicated, and muscle transfers may be considered. Table 8.1 Electromyography Guide Normal voluntary action potentials indicate the presence of functioning motor axons with stimulating motor units of facial muscle. Polyphasic potentials indicate reinnervation and may precede clinical reinnervation. Denervation or fibrillation potentials indicate that denervated muscle exists. Electrical silence, with no potentials seen, indicates muscle atrophy. The extratemporal facial nerve has five divisions: the temporal, zygomatic, buccal, mandibular, and cervical. Each division innervates a group of muscles. Understanding the general nerve muscle distribution of the 18 paired muscles of the face is important in determining the impact of a facial paralysis and the optimal reconstructive technique to address the deficit. An understanding of these relationships is helpful, but facial expression is highly individualized. No two smiles are the same, and although the muscles of action may be similar between two people during a smile, the angles and vectors of muscle contraction result in a unique smile pattern. Replicating the smile pattern in the paralyzed face is a challenge that continues to elude us in spite of our rather complex reconstructive techniques. A variety of facial nerve grading scales have been described, but the House-Brackmann scale has been adopted by the Facial Nerve Disorders Committee of the American Academy of Otolaryngology–Head and Neck Surgery in 1985 because of its reproducibility and ease of use (Table 8.2).2 The HouseBrackmann scale is useful for evaluation of general function, but it is insufficient for precise assessment of defects affecting one or more branches of the facial nerve. When the facial nerve is acutely transected, an immediate neurorrhaphy will yield the best results for reinnervation. Acute injury may occur during a surgical resection or traumatic injury. If it occurred less than 72 hours earlier, the injury can still respond to electrical stimulation for nerve identification; however, after 72 hours, the distal nerve does not stimulate and the surgeon must rely on surgical dissection and visual identification of the distal nerve branches. Primary reanastomosis in the acute setting offers the best opportunity for recovery. In our experience, an immediate repair that is performed with meticulous surgical technique can provide excellent results. In general, distally occurring injuries result in better outcomes than proximally occurring injuries. It is clear that the best results are achieved when there is a tension-free anastomosis. Table 8.2 The House-Brackmann Grading System Grade Description Characteristics I Normal Normal facial function in all areas II Slight Appearance: slight weakness noticeable on close inspection; may have very slight synkinesis At rest: normal symmetry and tone Forehead motion: moderate to good function Eyelid closure: complete with minimal effort Mouth motion: slight asymmetry III Moderate Appearance: obvious but not disfiguring weakness between the two sides; noticeable but not severe synkinesis, contracture, or hemifacial spasm At rest: normal symmetry and tone Forehead motion: slight to moderate movement Eyelid closure: complete with effort Mouth motion: slightly weak with maximal effort IV Moderately severe Appearance: obvious weakness or disfiguring asymmetry At rest: normal symmetry and tone Forehead motion: none Eyelid closure: incomplete Mouth motion: asymmetric with maximal effort V Severe Appearance: only barely perceptible motion At rest: asymmetric Forehead motion: none Eyelid closure: incomplete Mouth motion: slight movement VI Total No facial function Source: From House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg 1985;93:146. Reprinted by permission. Fig. 8.1 The surgical technique for primary neurorrhaphy requires epineural sutures place meticulously to achieve a tension-free neural anastomosis. The endoneurium should be trimmed, and four to six microsutures should be placed in an interrupted fashion. ♦ When a nerve transaction has occurred, whether incidental or intentional, it is important to examine the proximal and distal nerve for crush injury. The nerve should be trimmed back to achieve an area of clean transection without epineural or perineural crush injury. ♦ When the proximal and distal ends of the nerve are opposed, there should be enough nerve length that there will be no tension on the neural anastomosis. If there is tension, a cable graft should be performed. ♦ Under high-powered magnification, an 8.0, 9.0, or 10.0 microsurgical suture should be used to perform an epineural neural anastomosis. We recommend using the fewest number of sutures to achieve the anastomosis. Four to six epineural sutures typically achieve the desired result. There should be no attempt to realign individual fascicles. ♦ It is ideal that the neural anastomosis be performed in a well-vascularized bed. A bed that has been previously radiated or laden with scar will inhibit healing. In some cases, transposition of healthy vascularized tissue, including muscle or temporoparietal fascia, may help the process of healing. Primary neural reanastomosis is best performed in the setting of an acute nerve transaction when there is no tension on the anastomosis. This approach can be used in cases where the primary injury has occurred up to 1 year earlier; however, the best results are always achieved in those who are treated early in the time course. Results are also best in young patients. A poorly vascularized tissue bed is often a deterrent to healing. Any effort to improve the vascularity of the tissue bed will aid healing. Postoperative nerve regeneration occurs at a millimeter per day in the optimal scenario. The age of the patient, the health of the patient, and the nature of the tissue bed will all play a role in the speed of recovery. A cable or an interposition nerve graft is commonly used following a radical parotidectomy with facial nerve sacrifice, a temporal bone resection, or traumatic avulsion. As discussed, a tension-free repair is critical, and when a tensionfree apposition cannot be achieved using primary nerve ends, cable grafts are recommended. A nerve graft can be harvested from the greater auricular nerve, the sural nerve, the cervical nerve, or the medial antebrachial cutaneous nerve. Although the greater auricular provides a unifascicular nerve with very good diameter, the sural and antebrachial cutaneous nerves offer nerve grafts that branch and can be used when multiple nerve grafts are required (Fig. 8.2). The sural nerve is the longest donor nerve, with up to 70 cm of graft available.
Management of the Paralyzed Face
♦ ASSESSMENT OF THE PATIENT WITH FACIAL PARALYSIS
Patient Examination
Assessment of the Nerve Function
♦ RELEVANT ANATOMY
♦ CLASSIFICATION AND GRADING OF FACIAL PARALYSIS
♦ MANAGEMENT OF THE ACUTE INJURY
Option for Management: Primary Reanastomosis
Surgical Technique and Considerations (Fig. 8.1)
Patient Selection and Perioperative Management
Option for Management: Nerve Graft
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine