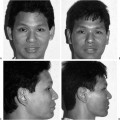
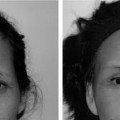
14 The past decade has marked an exciting period for management of the Asian skin. With the rise of nonablative laser and light therapy, a host of skin ailments that afflicted Asian skin can now be addressed without the burden of a protracted recovery period traditionally observed in the postresurfaced Asian skin. Use of ablative modalities, for example, carbon dioxide (CO2) laser resurfacing, medium to deep chemical peeling, and mechanical dermabrasion, led to an unacceptably long recovery in most Asian patients, who suffered from postinflammatory hyperpigmentation, hypopigmentation, lingering erythema, and potential scarring.1 Judicious and conservative use of these ablative treatment modalities still play an important adjunctive role when nonablative therapy is inappropriate or ineffective. The CO2 laser is a particularly poor tool for the Asian skin, which can face a recovery time that approaches a year and can lead to permanent pigmentary loss. Lighter chemical peels (15 to 35% tricholoroacetic acid [TCA] with or without Jessner’s solution or Jessner’s solution alone) can be used in combination or separately from nonablative therapy to effect maximal improvement in cutaneous dyschromias and wrinkles. Asian skin stands in marked distinction to that of Caucasian. The fine to deep wrinkles that characterize mature Caucasian skin are less prevalent in Asian skin partly due to the photo-protective effect of the darker complexion and to the thicker dermal structure. Asians are instead plagued by superficial dyschromias, including solar lentigines, melanocytic nevi, ephelides (freckles), nevi of Ota, and melasma. Although these conditions exist in the Caucasian, they tend to be less common, and Caucasians better tolerate ablative removal of these lesions than Asians. Although freckles may be deemed charming in Western culture, Asians from the Far East may consider any skin discoloration to fall short of the unblemished complexion idealized in the Orient. Understanding this cultural difference may help Western physicians in their treatment objectives with the Asian patient. A new paradigm has been proposed that may facilitate a more systematic appraisal for the complexities that define the disparate Asian populations and their related skin types. Dr. Nabil Fanous has recently delineated a racially based skin classification system that divides the globe into latitudinal zones (Fig. 14-1).2 His taxonomy envisions the West as subdivided into Nordic, European, Mediterranean, Indo-Paki, and African as the latitudes are traversed from northernmost to southernmost. Accordingly, the finer features and fairer complexion (Nordic) in the far northern climes give way to increasingly darker and coarser attributes (African) of the southern reaches. In the East, Fanous argues that Asians may also be classified according to the same methodology as their Occidental counterparts. However, the geographic span of the Asian world roughly parallels the corresponding latitudes of the Mediterranean to the African. Therefore, despite a milky-white complexion, northern Koreans who occupy the northernmost Asian latitude will have a similar response to ablative resurfacing as Mediterranean skin. Likewise, the Polynesian skin of the southernmost zone will be more akin to the Western equivalent of African skin. Actual skin color (Fitzpatrick grading) becomes only one variable in the overall racially defined (features and skin type) classification scheme. As far as the West is concerned, Fanous argues that the European skin type is most suitable for resurfacing. The Nordic race has very thin skin that is more susceptible to atrophic scarring and telangiectasia. Conversely, the Indo-Paki and African skin types have a greater propensity to hypertrophic scarring and pigmentary abnormalities, ranging from transient hyperpigmentation to more irreversible hypopigmentation. Therefore, the extremes of skin color and type represent the most precarious recipients of resurfacing. The intermediate skin types, the European followed by the Mediterranean, constitute the most favorable skin types for resurfacing. Similarly, as mentioned, the Asian hemisphere falls along latitudinal lines that parallel the Mediterranean to the mid-African zones but oftentimes behaves more like the European to the African in terms of response to resurfacing. Therefore, perspicacious attention to these factors that delineate different Asian skin types will help to navigate a safe course for the physician about to embark on a resurfacing plan for the Asian patient. Figure 14-1 A new racially based skin classification system divides the globe into latitudinal zones. The West is divided into the Nordic, European, Mediterranean, Indo-Paki, and African zones, in which both skin color and facial features change from lighter and finer to darker and coarser from north to south. A similar zonal distribution is paralleled in Asia that roughly corresponds to the Mediterranean and African zones in the West. These corresponding latitudes serve to define skin response to therapy. Beyond all the dissimilarities that flourish between Asian populations, definite anatomic traits unify these apparently disparate groups. Overall, Asian dermis tends to be thicker and more sebaceous in quality, a characteristic that is independent of skin color. Even the fairer-complected northern Asian races exhibit this skin quality, which informs their response to peeling as well as their postoperative course. Most Asians, except the darker Malay or South Asians, tend to be suitable candidates for resurfacing if the proper risks and limitations are grasped by surgeon and patient alike. The most troublesome sequela or complication that arises concerns pigmentary problems, including prolonged erythema, hyperpigmentation, and hypopigmentation. It is unclear whether a rigorous preoperative course of tretinoin and/or hydroquinone can circumvent this outcome. West and Alster’s prospective, blinded and controlled study of their patients (who were primarily Caucasian) proved that intensive preoperative regimens failed to suppress postoperative melanin production. Their theory holds that the superficial melanocytes that have been curbed by the topical agents are eventually removed by the peel anyway and that the deeper melanocytes remain undisturbed by the preoperative treatment.3 Nonablative skin therapy refers to laser and light therapies that do not efface the epidermis but instead target a specific chromophore in the skin (e.g., melanin pigment or a red vascular lesion), based on the principle of selective photothermolysis expounded by Anderson and Parrish.4 Each type of laser possesses a certain characteristic wavelength that may be better suited to address a lesion of a particular color. Nonablative lasers and broadband light devices can also rejuvenate the skin by increasing collagen in the dermal layer via nonselective thermal stimulation (Fig. 14-2).5 Wrinkle reduction and treatment of acne scarring have been addressed with variable success using nonablative therapy. To overstate the impact that nonablative therapy has on wrinkles and scarring would be fallacious, as this technology provides only subtle but definite improvement. When significant rhytidosis or scarring is present, then traditional ablative techniques may be used instead or in combination with nonablative therapy. Similarly, recalcitrant pigmentation may be best addressed with both ablative chemical peeling and nonablative laser therapy. This section is not intended to be exhaustive in nature but reflects the author’s clinical experience as well as reviews techniques that have been effective in the Orient for Asian skin. Figure 14-2 Illustration shows the nonablative laser or light beam (green arrow) passing into the dermal layer of the skin to effect collagen stimulation by thermal injury without any epidermal damage. Q-switched (QS) lasers customarily have been thought to have the greatest utility with effacing pigmented cutaneous lesions. Q-switching permits a short burst of intense energy that leads to a temperature gradient between the target and neighboring tissue. As the temperature difference falls, local shockwaves are emitted that cause tissue fragmentation and thereby melanasomal injury. QS lasers that have been used successfully for pigmentary ablation in Asian patients include the QS neodymium: yttrium alumium garnet (Nd:YAG) (potassium-titanyl-phosphate (KTP)) 532 nm laser, the QS ruby laser, and the QS alexandrite laser.6,7 One prospective, randomized study evaluated the efficacy of the Medlite QS 532 nm Nd:YAG laser, the Versapulse QS 532 nm Nd:YAG laser, and the Versapulse long-pulsed 532 nm Nd:YAG laser in 34 Chinese patients who had their hemifaces treated with the respective laser types.8 A visual analog questionnaire given to the patients and two blinded observers found that the long-pulsed laser was significantly better than the Versapulse QS 532 nm Nd:YAG laser but comparable to the Medlite QS 532 nm Nd:YAG laser in terms of efficacy for pigmentary clearing and associated complications of hyperpigmentation, hypopigmentation, and erythema. A long-pulsed laser can be safely and effectively used for the Asian skin as long as the pulse duration is kept shorter than the thermal relaxation time of 10 msec given an epidermal thickness of 100 mm. This shorter pulse duration theoretically limits the thermal diffusion from the epidermis to the dermis, which could in turn engender scarring. However, when the principal pathology resides in the dermis, targeting vascular ectasias and the local blood supply to various lesions (verrucae, sebaceous hyperplasia, etc.), the pulse duration may be intentionally lengthened to penetrate to the intended depth. The author has the most experience with the long-pulse 532 nm (KTP) Nd:YAG laser to address a host of cutaneous disorders in Asian patients, including unwanted pigmentation, vascular lesions, fine wrinkles, sebaceous hyperplasia, and verrucae (Figs. 14-3A-D, 14-4A,B). The patient who desires treatment of unwanted pigmentation should be carefully evaluated first for any suspicion of neoplasia before electing to proceed with aesthetic removal. The patient should also be fully cognizant that treatment of aberrant pigmentation may take several sessions, depending on the type of skin pathology, and should be combined with topical agents for maximal benefit. The patient may be started on 4% hydroquinone or alternative lightening regimen (e.g., kojic acid or azelaic acid) throughout the treatment period as well as a sunblock containing SPF 30 or 35. Proper avoidance of sun exposure is the key to success and to maintain the longevity of the result. Because abnormal pigmentation is a result of chronic sun exposure, the patient should also be made aware that ongoing sun exposure would predispose toward an early recurrence of solar lentigines and ephelides. Use of a lightening agent and sunblock are particularly important in the peritreatment period to minimize the risk of unwanted postinflammatory hyperpigmentation, which is a common sequela in the Asian patient. The sensitive patient may be prescribed a topical anesthetic cream, for example, EMLA (Astra Pharmaceuticals, Westborough, MA) or ELA-Max (Ferndale Laboratories, Ferndale MI), to be applied to all proposed treatment areas at least 1 hour before laser therapy. Figure 14-3 (A,B) This 39-year-old Vietnamese man had multiple pigmented lesions on both cheeks. (C,D) Patient shown 2 weeks after one treatment with the 532 nm KTP laser. The settings used were 7 J/cm2, 8 msec pulse duration, and two passes per lesion. After informed consent is obtained, the patient is brought to the treatment room, which should comply with proper laser precautions. The room door should be closed (preferably locked), a laser warning sign should be posted on the door, and the patient and physician should don wavelength-specific protective eyewear (Fig. 14-5). Generally, freckles can be treated in one setting, but melasma and deeper (dermal) pigmentation may require 5 to 10 sessions, with an interval of 4 to 6 weeks between treatment sessions. Depending on the lesion size, a 1, 2, or 4 mm handpiece is employed. Generally speaking, a 2 mm spot size is preferred to address the majority of dyschromias, as the 1 mm size is often too small, and the 4 mm size may cause too much deep thermal injury. A fluence of 7 to 10 J/cm2 set at a 7 to 10 msec pulse duration can be used, depending on the amount of observed pigmentation, with a higher fluence used for light-colored lesions and a lower fluence for more pigmented lesions. A lower fluence can be used for darker lesions because the more pigmented lesion readily absorbs the wavelength-specific energy of the laser than a comparable lighter lesion. The color end point of treatment should be an ashen gray without discernible purpura. The lowest fluence that can bring about this color change should be used to minimize adverse effects. Patients may benefit from a test patch with the fluence and other laser parameters recorded to determine the efficacy and likelihood for postinflammatory hyperpigmentation. Even patients who do not report tanning after sunbathing can develop hyperpigmentation and therefore should be assessed for this development with a test patch. Figure 14-4 (A) This 30-year-old Chinese woman shows large areas of post-inflammatory hyperpigmentation on her cheeks and smaller, discrete areas across the remainder of her face due to acne flare-ups. (B) She is shown 1 month after one treatment with the 532 nm KTP laser, with notable improvement in areas of hyperpigmentation. She now shows some new areas of hyperpigmentation from new acne flare-ups. She was treated with 6 J/cm2, 8 msec, and two pulses and was retreated for the new areas of hyperpigmentation. She also underwent topical therapy for her acne. Figure 14-5 A patient undergoing treatment for pigmented lesions with a long-pulsed 532 nm laser. The physician wears wavelength-specific protective goggles, and the patient also wears protective eyeshields and is further instructed to keep his eyes closed during the entire treatment session. In accordance with laser precautionary measures, a danger sign warning that a laser is in use is posted outside the door, and the room door is locked from entry. The 2 mm handpiece is used to treat these superficial dyschromias set at 7 J/cm2 and 8 msec pulse duration for this particular patient with two passes per lesion to achieve an ashen gray color end point. For pigmented lesions, the author prefers to begin in a less conspicuous area away from the central aspect of the face for the test spot. As mentioned, the 2 mm handpiece is used unless the lesions appear to be very small and would be amenable to the 1 mm handpiece. The starting laser parameter preferred for pigmented lesions is 7 to 8 J/cm2, at 8 to 10 msec pulse duration set at two pulses per second. Unlike vascular lesions, the pigmented lesions should generally be hit with two consecutive pulses until the lesion appears ashen gray. Oftentimes, an audible snap sound may be heard after the second pulse that confirms that the pigment has been properly ablated. If the fluence is insufficient to achieve the desired color end point, the laser is adjusted higher. Use of cooling spray or gel may actually make determination of color change more difficult. The lowest fluence that will achieve this color change should be used to avoid unnecessary overtreatment and risk of thermal injury with resultant blistering and potential scarring. This laser can also be used to address vascular lesions, particularly those that are red in color and more superficial in distribution. Although cutaneous lesions of a vascular nature are more common in the fairer-skinned Caucasian patient, telangiectasia, angiomata, and rosacea can also afflict the Asian patient. The size of the handpiece should be 2 mm for both telangiectasia and angiomata, whereas a scanning 1 mm handpiece or a 4 mm handpiece is more appropriate for rosacea. For telangiectasia, the 2 mm handpiece is preferred even though the caliber of the vessel may be only 1 mm in diameter, because the wider beam width will ensure that the vessel is entirely circumscribed and vaporized. With this type of laser, no purpura should be encountered. Unlike treatment of superficial pigmented lesions, only one pass of the laser is used to ablate vascular lesions at a higher fluence. Typically, a setting of 13 to 16 J/cm2 with a pulse duration of 16 to 20 msec is used for vascular lesions, but lower fluences should always be tried first to ensure that the lowest, safe fluence for therapy is used. In addition, a cooling apparatus is favored to minimize epidermal damage and to minimize discomfort. Of note, use of a cooling apparatus obviates the need for pretreatment topical anesthesia. In addition, ultrasound gel will facilitate easy passage of the cooling head over the skin. For sebaceous hyperplasia, a 1 mm handpiece is used at a higher fluence (25 to 35 J/cm2) and longer pulse duration (30 msec) to attenuate the blood supply to the lesion and thereby effect involution. For verrucae, similar parameters are used (30 to 40 J/cm2 and 30 to 40 msec), but the tissue is ablated with multiple stacked hits (typically five or six pulses) until the tissue evaporates. The charred tissue is wiped away with a moistened 4 × 4 gauze, and the process is continued until the wart is brought level with the surrounding tissue or pain is encountered, which signifies arrival at normal tissue. For photorejuvenation of aged Asian skin, a low fluence (6 to 7 J/cm2), a long pulse duration (30 to 40 msec), and a larger handpiece (4 mm) are used with a cooling device and chilled gel and passed over the skin evenly two or three times. Repeat treatment sessions for photorejuvenation may be undertaken every 4 to 6 weeks. The same settings can be used to treat rosacea. After treatment, the patient can apply a light coating of bacitracin or Aquaphor ointment, which can be particularly beneficial in the healing process when a microcrust forms. The patient should be advised not to abrade or manipulate the area during the first week after treatment. The application of hydroquinone and sunblock should be resumed unless the patient reports significant irritation with these topical agents during the healing phase. Blistering after therapy may rarely occur and signifies overtreatment. Any blisters should be reported to the physician immediately for close scrutiny and follow-up. The blistered areas should be treated with bacitracin or Aquaphor until full epithelialization is encountered, and the patient should be sternly advised not to scratch, pick, or manipulate the areas to minimize the risk of scarring. Temporary hypo- or hyperpigmentation may occur, which typically resolves if the proper laser parameters described above are followed. The reader is advised to consult the manufacturer of his or her laser device for specific recommendations as to the proper settings for that particular laser model. As an alternative to the 532 nm laser (or other comparable laser), intense pulsed light (IPL) has been used successfully in Asian skin for a wide spectrum of skin ailments. IPL can be used for dark spots, vascular lesions, and photorejuvenation of fine wrinkles. It is a noncoherent, broadband (500 to 1200 nm) light device in which selective cut-off filters can be employed to block specific shorter wavelengths (e.g., 515, 550, 570, 590, 615, 645, 695, 715, 755 nm). Accordingly, it is not a true laser. Pulse width varies from 0.5 to 25 msec, and fluence ranges from 3 to 90 J/cm2. The fluence can be delivered from one to three separate emissions with a 1 to 300 msec interval between individual pulses. Three spot sizes can be selected: 8 × 8 mm, 8 × 15 mm, and 8 × 35 mm. Epidermal protection is afforded by a cooling gel applied topically and by a built-in thermoelectrically cooled crystal filter and a physical spacer to maintain the requisite 2 mm distance from the skin. The literature has reported effective use of this technology to address solar lentigines, ephelides, telangiectasia, and wrinkles in the Asian patient.9–12 Compared with targeted laser systems, IPL can still address dyschromias effectively but may require more treatment sessions to demonstrate the same benefit. Ultraviolet (UV) photography may also enhance the visibility of epidermal melanocytic hyperpigmentation. The IPL may be associated with less chance of postlaser hyperpigmentation and can be used for those patients who are more predisposed to this outcome. Generally, a total fluence of 23 to 32 J/cm2 in a double-pulse mode of 2.5 to 4.0/4.0 to 5.0 msec pulse durations and an interval of 20.0/40.0 msec between pulses may be used safely for Asian skin. Typically, a topical anesthetic is not required but can be used for more sensitive patients. The color end point should be a slight erythema immediately after light exposure and a slight increase in pigmentation in the treated dark spots. If the patient experiences significant discomfort after light application, a superficial burn may have occurred, and the fluence should be appropriately reduced. The upper eyelids should always be spared as well as the beard distribution in men. Typically, a minimum of three treatment sessions is required, but a benefit may be more noticeable after only five sessions, depending on the type of cutaneous pathology being treated. Safety with IPL is of paramount importance to avoid burn injury (Figs. 14-6, 14-7). Consistency of therapy will be attained with clinical experience. However, certain protective measures may be followed to minimize the risk of burn injury, which may be more likely in the Asian patient, given the darker skin that more readily absorbs the light energy. Use of cooling gel is important for epidermal protection, and the handpiece should be at a uniform distance of ~2 mm from the skin, with the intervening gel serving as the interface. Maintaining this 2 mm distance uniformly is perhaps the most difficult aspect in light therapy and may predispose toward burn injury (Fig. 14-8). When the trigger switch is initially turned on, depressing the button on the handpiece often moves the device too close to the skin, predisposing toward burn injury (Fig. 14-9). Also, passage of the IPL over raised or depressed contours of the face makes maintenance of a uniform distance from the skin demanding (Fig. 14-10), especially because the light-emitting head is broadly configured in a relatively large rectangular block. A physical spacer device that extends from the light-emitting head will help maintain the prescribed 2 mm distance more easily (Fig. 14-11A). Dr. Takahashi has developed a grid-shaped spacer that has proven to be invaluable in achieving the most uniform distance from the skin for the novice to the experienced technician (Fig. 14-11B).* The standard spacer is hollow in the center, allowing the skin to bulge closer to the light-emitting head, especially with slight pressure. The modified grid shape is chosen over a completely flat contour to enhance skin cooling but not overly cool the skin that would arise with the latter design. Cooling gel should still be applied, as it permits ease of gliding over the skin surface and provides additional thermal protection. Careful administration of IPL can result in excellent clinical results, but caution should always be heeded when approaching the darker-complected patient. Figure 14-6 This 27-year-old Japanese woman underwent six intense pulsed light (IPL) treatments and experienced a burn injury on the sixth session. Her first treatment was undertaken at 24 J/cm2; the second, at 25 J/cm2; the third, at 26 J/cm2, the fourth, at 27 J/cm2; and the fifth, at 28 J/cm2. The sixth session was started at 28 J/cm2 initially when the patient complained of some discomfort, so the fluence was reduced to 27 J/cm2, after which she was noted to have a burn injury. Upon recognition of the burn, the patient was treated with topical application of steroid cream (0.12% betamethasone valerate) for a 1-week period, and her condition resolved without any scarring. (Courtesy of Tomoyuki Takahashi, M.D.) Figure 14-7 This 29-year-old Japanese woman experienced a burn injury on the third treatment session at 26 J/cm2, the same setting that was successfully used during the second treatment session. The patient’s burn was treated with steroid cream application with successful resolution without scarring. (Courtesy of Tomoyuki Takahashi, M.D.) Figure 14-8 Given the broad configuration of the light-emitting head, the ability for the entire surface area to maintain a uniform distance from the skin may be difficult. (Courtesy of Tomoyuki Takahashi, M.D.) Figure 14-9 Maintaining a uniform distance to the skin is particularly difficult when the trigger button is depressed, as the light head tends to move closer to the skin, predisposing to burn injury. (Courtesy of Tomoyuki Takahashi, M.D.) Figure 14-10
Management of the Asian Skin
♦ General and Anatomic Considerations

♦ Nonablative Therapy

532 nm KTP Nd:YAG Laser


Intense Pulsed Light (IPL)



![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree