(1)
Department of Dermatology and Allergology Biederstein, Technische Universitaet Muenchen (TUM), Munich, Bavaria, Germany
(2)
Christine Kuehne Center for Allergy Research and Education (CK-CARE), Hochgebirgsklinik (High Altitude Hospital), Davos, Switzerland
Many patients with atopic dermatitis are desperate, change doctors, and visit “witchcraft” and “shaman” gurus because they have heard that atopic dermatitis is incurable. Many physicians use this sentence to finally be left in peace by demanding patients or parents. Of course they feel correct with this sentence stressing the genetic predisposition which is inborn and which cannot be altered at the moment. However, one has to clearly distinguish: The genetic disposition of atopy or atopic dermatitis cannot be changed today; however, molecular genetics may soon be valuable in predictive diagnostics.
These genetic markers, however, are not the disease; the disease “atopic dermatitis” can very well be treated and very often disappears over long periods or for lifetime. Therefore, I never use the term “incurable”; I prefer to tell the patients that they have a problem and a tendency to develop hypersensitivity reactions of the skin and maybe elsewhere but that these clinical conditions can very well be treated. I tell my patients that streptococcal tonsillitis cannot be called “incurable” just because there may be a relapse. The angina can very well be treated.
Based on the complex etiopathophysiological mechanisms involved, it becomes clear that therapeutic management in most patients requires a complex program of management including aspects of diagnostics, prevention, and actual treatment.
Therapeutic procedures focus on the one hand on the acute treatment of the inflammatory skin disease; on the other hand and at the same time, they have to include preventive aspects regarding the disturbed skin barrier function and individual provocation factors which can be avoided (Abeck and Ring 2002; Abels and Brocks 2006; Akdis et al. 2006; Braun-Falco and Ring 1984; Ellis et al. 2003; Harper et al. 2002; Leung and Barber 2003; Przybilla et al. 1994; Schnopp and Ring 2003; Ring et al. 2012; Darsow et al. 2013; Wollenberg et al. [in press]). The acute eczema flare can be treated very well; it is difficult to predict the intensity and frequency of new flares.
The tendency to develop hypersensitivity reactions of the skin requires special care and may be time-consuming.
Thus, management of atopic dermatitis is much more than writing a prescription for a tablet or an ointment. Rather, it requires intense diagnostics including allergy diagnosis for individual provocation factors and needs a confidential cooperation between physician and patient so that behavioral changes can be induced. The motivation of the patient or the parents to take responsibility for the disease has to be slowly developed (patient “empowerment”) and often needs special educational programs. These aspects will be covered in Sect. 6.4 (Eczema School). I like to call the whole bunch of procedures to be done in order to improve the clinical condition “patient management” (Ring et al. 1996). These procedures comprise much more than diagnostics and treatment and include recommendations regarding nutrition, style of living, leisure activities, occupational counseling, etc.
4.1 Diagnostic Procedures
There are few diseases where diagnostics and therapy are so closely connected as in allergy and especially atopic dermatitis.
This chapter does not deal with the actual diagnosis “atopic dermatitis” and considerations for differential diagnosis, but it reflects the ongoing diagnostic procedures necessary in the individual patient after the diagnosis “atopic dermatitis” has been made (Prucha et al. 2013). Like in all other allergic diseases, the procedure can be classified into four steps (Darsow and Ring 2000; Høst et al. 2003) which are connected to each other (Ring 2005) (Fig. 4.1):
Fig. 4.1
The four major parts of allergy diagnosis
History
Skin test procedures
In vitro allergy diagnostics
Provocation tests
At the moment there is no standard routine procedure for provocation testing with aeroallergens in atopic eczema such as an exposure in a standardized chamber (pollen chamber) with varying concentrations of aeroallergens (Heratizadeh et al. 2015). Thus, provocation tests at the moment are restricted to food and food additives (see below).
4.1.1 History
A very careful history not only considers the clinical course of the disease but also includes questions regarding the symptoms, the onset, the duration, the timely course, and the circumstances with regard to possible triggering factors like seasonal, local, and occupational conditions. Activities in holidays or leisure, application of drugs, hormonal situation, and stress all have to be included in a careful history in atopic dermatitis (Brockow et al. 1999a) (Table 4.1).
Table 4.1
Contents of a good history in atopic dermatitis
Symptoms |
Onset (first onset, acute disease) |
Duration |
Timely course (circadian, around the year, seasonal) |
Intensity (severity) |
Frequency |
Response to therapy |
Exacerbation by therapy |
Hospitalization |
Concomitant diseases |
Personal history (atopy) |
Family history (atopy) |
Other diseases (gastroesophageal reflux, skin or airway diseases) |
Eliciting factors and environmental aspects |
Season |
Local environment (indoor, outdoor) |
Occupation |
Holiday |
Hobby |
Drugs |
Foods |
Exercise |
Stress, emotional excitement |
Common cold (viral infection) |
UV light |
Hormonal situation (menstruation, pregnancy) |
Lifestyle |
Living, apartment |
Animal contact (also passive) |
Tobacco smoke (active, passive) |
House dust mite, molds |
Chemicals |
Plants |
Cosmetics |
Snarling, breathing through the mouth |
4.1.2 Skin Test Procedures
Among various skin test procedures, primarily those which are done percutaneously (scratch test, skin prick test) as well as patch test procedures are discussed.
4.1.3 Prick and Intradermal Test
The most commonly used skin test is the skin prick test where a drop of an allergen extract is applied to the skin and pricked with a special lancet, preferably without bleeding. After 15 min, it is read. Positive prick test reactions are typical for atopic diseases; occasionally, they are exclusively used for the diagnosis of atopy. It is estimated that 90 % of atopics show positive skin prick test reactions against common aero- or food allergens (especially cat, house dust mite, and grass pollen) (Guillett and Guillett 1992; Schäfer et al. 1997a). In the intradermal test, 0.02–0.05 ml of an allergen dilution are injected strictly intradermally, using a small needle. Intradermal tests are necessary when prick tests remain negative in spite of a suggestive history.
The interpretation of the test results has to be done with regard to possible clinical relevance from detailed history or provocation test (see below).
4.1.4 Atopy Patch Test (APT)
Positive skin prick tests or specific IgE antibodies against aeroallergens or foods almost routinely can be found in atopic dermatitis. The relevance of these sensitizations was controversial over decades. In the philosophy of this disease in the last hundred years, the estimation of allergy playing a role went up and down like modes of fashion. Decades where merely the dry skin or the psychological influence was in the focus alternated with phases where the role of allergy was put forward strongly. Mainly due to lack of methods, this uncertainty continued. It is a clear clinical experience that many patients develop flares after contact with animal dander or in dusty environments while they experience improvement in allergen-free rooms or under high-altitude conditions (Borelli et al. 1967; Storm van Leeuwen et al. 1926).
At the end of the 1970s of the twentieth century, several working groups wanted to develop a test procedure as a correlate for these clinical observations, since the skin prick test alone was not suitable. It correlated much better with the allergic airway reactions of hay fever or asthma than with the atopic dermatitis symptoms.
We first tried the intradermal test with a late reading and believed to find a correlate in the so-called late-phase reaction (LPR) similar to severe cases of bronchial asthma (Dorsch et al. 1982). This late cutaneous reaction (LCR) was regarded as a model of atopic eczema; however, the absence of epidermal involvement, which is so characteristic of the eczematous inflammation, was an argument against this idea (see Chap. 1).
Therefore, we and other groups tried to induce eczema by epicutaneous application of aeroallergens; we used intradermal and prick test extracts and remained unsuccessful for many years. Others tried to come to positive test reactions by manipulation of the test areas through tape stripping or preceding scratching with irritation. The breakthrough was done by the group of Thomas Platts-Mills (Mitchell et al. 1982; Platts-Mills et al. 1983) who were able to induce eczematous skin reactions after application of house dust mite extract on rather large skin areas. Therefore, in the future we used larger Finn chambers than normally used for the classical patch test in contact allergy and were equally successful in the procedure which we called “atopy patch test” (APT) (Darsow et al. 1996, 1999; Ring et al. 1989, 1997, 2001b; Vieluf et al. 1993).
In the 1990s, we standardized the APT with regard to methodology, skin test site, influence of medication, extracts used, etc., especially also considering the vehicles (Darsow et al. 1996; Langeveld-Wildschut et al. 2000). Today, we can say that the atopy patch test represents a standard procedure in allergy diagnostics for patients with atopic dermatitis (Darsow et al. 1999) (Fig. 4.2). Contrary to our theoretical considerations, where we thought that a hydrophilic emulsion would be better for the application of protein allergens, petrolatum proved to be the most reliable vehicle also for the atopy patch test (Fig. 4.2a) (Darsow et al. 1996).
Fig. 4.2
Positive atopy patch test after 48 h. (a) Comparison of petrolatum and hydrogel as vehicle. (b) Allergen 200 IR/G (Index of Reactivity) in petrolatum. (c) Grass pollen and petrolatum control
4.1.5 Differences to Classical Patch Test
Apart from the methodology (use of larger diameter Finn chambers), there are differences between the atopy patch test and the classical patch test in contact allergy also in the reading of the test results (Table 4.2). In the atopy patch test, the substances used are protein allergens, while in the contact allergy patch test, small chemicals (haptens) are used. Furthermore, there are differences in morphology, dermatohistology, and time course. The classical patch test shows a typical crescendo pattern with a maximum of the reaction after 72 h; in atopy patch test, often a maximum is already reached after 48 h. The reproducibility of the atopy patch test is very good with 80–90 %. In the histopathology, an early influx of eosinophils and eosinophil products can be seen in the atopy patch test more commonly than in contact allergy. Clinically, often follicular patterns are observed; real vesicular or bullous reactions are extremely rare. The European Task Force on Atopic Dermatitis (ETFAD) has come up with a special reading guide for APT reactions (Darsow et al. 1999).
Table 4.2
Difference between classical patch test in contact allergy and atopy patch test
Criteria | Patch test contact allergy | Atopy patch test |
|---|---|---|
Nature of allergens | Low-molecular-weight chemicals | Proteins |
Kinetic of the reaction | Maximum after 72 h (crescendo) | Often after 24 h |
Morphology | Papulovesicular with spreading | Often follicular, rarely vesiculous |
Dermatohistology | CD4 lymphocytes, Th1 | CD4, Th2 Eosinophils |
Indication | Allergic contact dermatitis | Atopic dermatitis |
Unfortunately, test reagents are in many countries not routinely available; they have to be self-made by best using lyophilized allergens in petrolatum to be mixed by an experienced pharmacist (Darsow et al. 1996).
Pathophysiologically, the atopy patch test represents an artificially induced atopic inflammation after penetration of high-molecular weight allergens into the epidermis. These are recognized and taken up by dendritic cells (see Sect. 3.3). IgE and IgE-binding receptors have been recognized on the surface of epidermal dendritic cells partly in colocalization with house dust mite allergen (Maeda et al. 1992; Tanaka et al. 1990). From atopy patch test biopsies, specific T cell clones could be isolated which characteristically show a Th2 cytokine pattern. At a later point of time—after 48 h or in more chronic lesions—also in atopic inflammation Th1 patterns become visible (Bruijnzeel-Koomen et al. 1989; Kondo et al. 1998, van Reijsen et al. 1992; Wistokat-Wülfing et al. 1998).
In a common study of the European Task Force on Atopic Dermatitis (ETFAD), the atopy patch test was further standardized. Petrolatum was chosen as vehicle; the protein allergens from lyophilized extracts, together with minimal concentrations of an emulsifying agent, cetylpyridinium chloride, were mixed with petrolatum. In large Finn chambers (1 cm in diameter), they are applied to uninvolved and unaltered skin, preferably on the back. For the most common aeroallergens in central Europe, eliciting allergen doses between 5000 and 7000 protein nitrogen units (PNU) were used.
4.1.6 Results
The most common positive APT reactions were found with aeroallergens like house dust mite (Deleuran et al. 1998; Gondo et al. 1986) (Fig. 4.3), but also cat epithelium and pollen allergens are often positive (Darsow et al. 1996). The APT is dose-dependent and especially positive in patients where the eczematous skin lesions occur in air-exposed areas as, e.g., face, hands, or forearms. In a comparison of various test procedures, the clear-cut history in disease exacerbation offers that allergen contact was taken as gold standard; the following sensitivities and specificities could be calculated (Table 4.3). In 75 % of patients who had an exacerbation during the last preceding pollen season, atopy patch test against grass pollen was positive compared to only 16 % in eczema patients without seasonal exacerbation.
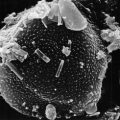
Fig. 4.3
The most common allergen positive in atopy patch is house dust mite Dermatophagoides pteronyssinus
Table 4.3
Sensitivity and specificity of various test procedures in patients with atopic dermatitis using clear-cut personal history as gold standard (Darsow et al. 1999)
Test | Sensitivity (in %) | Specificity (in %) |
|---|---|---|
Grass pollen (n = 79) Skin prick test | 100 | 33 |
Specific IgE | 92 | 33 |
Atopy patch test | 75 | 84 |
European Multicenter Study (n = 314) Skin prick test | 68–80 | 50–71 |
Specific IgE | 72–84 | 2–69 |
Atopy patch test | 15–45 | 64–91 |
German Multicenter Study (n = 253) Skin prick test | 69–81 | 44–53 |
Specific IgE | 65–94 | 42–64 |
Atopy patch test | 42–56 | 69–92 |
Compared to skin prick test and radioallergosorbent test (specific IgE antibodies), APT showed a lower sensitivity (75 %) compared to almost 100 % for the skin prick test, which is natural when we regard the atopy definition (see above). However, the specificity was much higher (80–90 %) for the atopy patch test compared to 40–60 % for skin prick test or RAST. It is possible, using the APT, to evaluate the relevance of an IgE-mediated sensitization for the actual eczematous skin changes and not for general allergy (see Fig. 4.4).
Fig. 4.4
Relevance of pollen exposure for exacerbation of atopic eczema in children (From MIRIAM-Panel-Study Augsburg, see Krämer et al. (2005))
Considerations regarding the concordance of the various test results are of special interest. There are patients with negative prick test and RAST and positive atopy patch test (Kerschenlohr et al. 2003b). In 53 of 314 patients (14 %), at least one allergen was positive in APT without corresponding sensitization in skin prick test or RAST (Table 4.4). This is interesting with regard to the question regarding intrinsic versus extrinsic atopic eczema (see Chap. 1). According to our understanding, positive atopy patch test reactions should be regarded as a sign of extrinsic atopic dermatitis, even if skin prick test and IgE are negative. Possibly the IgE reaction takes place without involvement of mast cells or circulating IgE antibodies but with involvement of IgE on the surface of dendritic cells.
Table 4.4
Positive atopy patch test in patients with negative prick test and negative RAST (43 out of 314 patients)
N | Allergens |
|---|---|
31 | Dermatophagoides pteronyssinus |
7 | Cat epithelium |
8 | Grass pollen |
16 | Birch pollen |
11 | Hen’s egg |
16 | Celery |
18 | Wheat flour |
The atopy patch test meanwhile has become a routine diagnostic procedure starting as a merely scientific instrument. We only recommend house dust mite avoidance with corresponding living and bedroom changes when the atopy patch test is positive.
4.1.7 Problem Food Allergens
The use of the atopy patch test with food allergens remains difficult (Werfel et al. 2007). While some years ago there was the big hope that, by using APT, one could replace time-consuming provocation tests in eczema (Niggemann et al. 2000; 2001), the nature and quality of food allergen extracts seem to be problematic. Direct application of native wheat flour, e.g., may be irritative. Atopy patch test with food is still a matter of scientific studies. However, in our and others’ experience (A Taieb et al., personal communication 1998), there are clear-cut positive APT reactions with foods especially in children who are negative in skin prick test and RAST and where this reaction is of clinical relevance.
4.1.8 Classic Patch Test for Contact Allergy
While some years ago allergic contact dermatitis was not regarded to be a problem in atopic eczema or was expected to occur much less frequently, recent studies have shown that contact allergy also represents a problem in atopic dermatitis. A recent study shows that in 6 % of over 600 patch-tested children with atopic dermatitis, positive epicutaneous tests were found especially for topical preparations such as emollients and antiseptics, particularly in children with severe atopic eczema (Mailhol et al. 2009; Lipozenzic and Wolf 2007).
Many studies have shown that allergic contact dermatitis can occur in patients with atopic dermatitis, especially in chronic hand dermatitis (Lipozencic and Wolf 2007; Rysted 1985; Schnuch et al. 2006; Dinkloh et al. 2015) (see Sect. 2.7.7 Contact Allergy). There are numerous studies showing that patients with atopic eczema also suffer from contact allergy. In our own study, we found 41 % (Enders et al. 1988) positive patch test reactions in atopic eczema patients. This also holds true for children who have been rarely tested epicutaneously so far. In an epidemiologic study, we found in preschool children up to 15 % allergic contact individuals, especially prominent to nickel, whereby there was a clear-cut correlation to ear piercing and nickel allergy in small girls (Kunz et al. 1990). But also chronic foot eczema can be due to contact allergy against shoe materials.
4.1.9 Testing of Corticosteroids
It is recommended to test patients with atopic dermatitis also with classical patch tests in order to rule out contact allergies. Special consideration should be given to the testing of topicals used, especially corticosteroid topicals which in chronic eczema can also act as contact allergens. This is often not easy to diagnose, since the pharmacological effect of anti-inflammatory cortisone acts against the inflammation while at the same time the nature as contact allergen maintains the inflammation. Therefore, in therapy-resistant eczema, the testing of topical corticosteroids is recommended also in children (Mailhol et al. 2009; Rycroft et al. 1991; Rystedt 1985, 1986; Susitaival and Hannuksela 1995; Uehara and Sawai 1989).
4.1.10 In Vitro Allergy Diagnosis
In vitro allergy diagnosis plays an important role in the management, especially in cases of severe atopic eczema with generalized skin lesions or under systemic medications.
4.1.11 Specific IgE Antibodies
The determination of specific IgE antibodies in serum is in the focus and represents the major progress in allergy diagnostics in the last fifty years. Since the introduction of radioallergosorbent test (RAST), a variety of procedures has been developed to measure circulating specific IgE antibodies in the serum in a quantitative or semiquantitative way (RAST classes or units kU/L).
Total serum IgE also should be determined; however, it is of less relevance. In extremely high serum IgE levels (above 1000 kU/L), mostly very severe cases of atopic eczema, the interpretation of specific IgE has to be modified because of the high background noise. Probably the ratio of specific IgE to total IgE may have a better diagnostic relevance with regard to the specific sensitization (Huss-Marp et al. 2011). Total IgE elevations can be regarded as general marker of the atopic diathesis. Atopic eczema is one of those diseases with the highest serum IgE levels measured, higher than in respiratory atopy (Wüthrich 1975; Ring et al. 2006).
4.1.12 Cellular In Vitro Allergy Testing
In rare cases, when no specific IgE is detectable in serum, the determination of basophil activation after allergen stimulation can be helpful, either as activation of basophil leukocytes by expression of CD63 (Basotest) or CD203 (flow CAST) (Sanz et al. 2002). Also the measurement of histamine or sulfidoleukotriene secretion from basophil leukocytes after allergen stimulation can give information (CAST-ELISA). With regard to delayed reactions of eczema exacerbation, also lymphocyte transformation tests have been used. The group around Thomas Werfel found food-dependent allergen-specific T cell clones (Reekers et al. 1996; Werfel and Kapp 2002; Werfel et al. 1996). All these methods are scientific in nature and have not found entrance into daily clinical use.
4.1.13 Oral Provocation Test in Food Allergy
Many patients with atopic eczema suffer from food hypersensitivity with variable manifestation, either as urticaria, angioedema, anaphylaxis (Jäger and Wüthrich 2001; Ring 1978), or exacerbation of an existing atopic dermatitis. The frequency of food allergy in atopic eczema is estimated around 20–30 % in childhood and considerably lower among adults (Ring et al. 2012). The most frequent food allergens in childhood atopic eczema are ovalbumin, cow’s milk, soy, wheat, but also peanut and tree nuts.
In diagnostics of food allergy, the real art is—as general in allergy diagnosis—to evaluate the relevance of a sensitization for the clinical disease. Many children have positive skin prick tests to various foods without ever noticing any deterioration of the symptoms after intake. Therefore, especially in this area, dietary recommendations should be very well considered (Kleine-Tebbe et al. 2009). We recommend the avoidance of a food only when the relevance of a sensitization for atopic eczema or for another allergic disease is certain.
4.1.14 Double-Blind Provocation Test
The determination of relevance can be done by clear-cut history (rather rare) or by oral provocation test best performed in double-blind procedure. The groups around Werfel and Niggemann found, in studies with double-blind, placebo-controlled oral provocation test, clear-cut positive reactions in over 50 % of the children (Niggemann et al. 2001; Werfel and Breuer 2004), similar to the results of Sampson (2001, 2003).
The timely appearance of skin lesions occurred in a majority of cases relatively rapidly (30 min to 2 h). Ca. 15 % react only after 12–48 h, which sometimes is difficult to recognize under daily life conditions. A rather large number of patients also experience immediate-type reactions together with delayed-type reactions to foods.
4.1.15 Practical Performance
The performance of a placebo-controlled oral provocation test needs a good blinding of foods which mostly are applied in porridge form (Bindslev-Jensen et al. 2004; Werfel et al. 2008a). The selection of the vehicle has to be done on the basis of previous allergy tests (skin prick test, RAST) since occasionally there are also allergens against unsuspicious foods like St. John’s bread. The foods to be tested are mixed with the placebo ground substance together with unsuspicious colorings and flavors (e.g., black currant juice) for blinding.
In the oral provocation test, food additives should not be forgotten since they also can trigger exacerbations in atopic eczema, especially in adults (van Bever et al. 1989; Vieluf et al. 1999). According to the schedule of the oral provocation test for idiosyncrasy (OPTI), as it is performed in chronic urticaria (Ring 2005) also in patients with atopic dermatitis, the detection of a pseudo-allergic hypersensitivity against food additives can be achieved (Ring et al. 1987; Worm et al. 2000) especially against sulfites.
With a history of severe anaphylaxis and positive skin prick test or RAST results, one can refrain from oral provocation.
In order to estimate the relevance of a sensitization for atopic dermatitis, however, provocation is often mandatory. The double-blind, placebo-controlled oral provocation test until now remains the gold standard and is usually done in specialized centers (Bindslev-Jensen et al. 2004). It can be further improved by the measurement of mediators in plasma during the provocation procedures (Ohtsuka et al. 1993). For the daily practice, a nutrition diary is recommended where the patient or the parents record the symptoms, together with the food intake (see Chap. 6).
4.1.16 Skin Test Versus RAST
Unfortunately, the predictive value of skin prick test and RAST with regard to food allergy in atopic eczema is limited. The positive predictive value (PPV) of food allergen-specific IgE is only around 30 % for eczematous skin reactions, while it is 60 % for clear-cut immediate-type reactions (Werfel et al. 2008a). Also the nature of the eliciting food allergen plays a role: The relevance of sensitization against hen’s egg or peanut is much higher than that of positive test against cow’s milk or cereals.
The role of atopy patch test in the diagnostic procedure for food allergy is controversial (see Sect. 4.1.4).
4.1.17 Microbiological Diagnostics
Based on the considerations regarding pathophysiology (see Sect. 3.4), microbial factors with colonization or infection of the skin surface should also be considered in the diagnostic procedure.
Microbiological examination makes sense and should cover the following aspects:
Bacteriological swabs of lesional and uninvolved skin as well as nasal mucosa (especially S. aureus)
Mycological examination of squamous material especially in the head/neck region (Malassezia furfur)
Virus detection of HSV when eczema herpeticum is suspected
In infants and small children with oozing skin lesions, superinfection is common not only by staphylococci but also by streptococci (impetiginized eczema). These considerations will also find entrance into the therapy (see Sect. 5.3).
4.1.18 Psychological Diagnostics
The clear-cut influence of psychological factors upon the clinical course of atopic dermatitis should be considered also in the diagnostic steps, and if there is an indication, psychosomatic counseling together with the use of validated questionnaires is recommended (Stauder and Kovacs 2003) (see Sect. 3.5).
In particular the following instruments have proven helpful:
Marburg Skin Questionnaire (Marburger Hautfragebogen MHF)
Cognitive Itch Questionnaire (Juckreiz-Kognitions-Fragebogen JKF) (Stangier et al. 1996)
Dermatology Quality of Life Index DQLI (Finlay and Khan 1994) (Deutsches Instrument zur Erfassung der Lebensqualität bei Hautkrankheiten, DIELH) (Schäfer et al. 2001; Staudt et al. 2002) (German Instrument for Quality of Life in Skin Diseases)
In addition there are specific questionnaires for children (Ravens-Sieberer and Bullinger 1998).
Often the motivation to write a diary for self-observation is very helpful for the patient in order to recognize the influence of psychological factors.
The most common psychological provocation factors comprise stress of any kind, both mental and emotional in nature (Richter and Dahme 1987). Furthermore, memories to significant life events which have not adequately been coped with, also too intensive concern with regard to the own skin disease, may have an enhancing or prolonging character (Hölscher 1998). The naive and well-meant question “How does your skin feel?” can occasionally trigger an intense itch crisis. Parents and relatives should be careful!
4.1.19 Summary
There are only few diseases where diagnostics and therapy are so closely connected as in allergy and eczema. Careful allergy diagnostics is standard in the management of atopic dermatitis and comprises the four steps from history and skin test to in vitro allergy diagnostics and provocation testing. The atopy patch test (APT) deserves special consideration; with this procedure, it is possible to evaluate the relevance of an IgE-mediated sensitization in patients with atopic dermatitis for the actual skin disease. The most common positive atopy patch test reactions are found against house dust mite, animal epithelia, and pollen. Also classic allergic contact patch test reactions should not be overlooked; contact allergy patch testing belongs to the standard diagnostic repertoire also in atopic dermatitis, also in childhood. Food allergy can often only be evaluated by placebo-controlled oral provocation tests. This also holds true for food additives which equally can elicit exacerbations of atopic dermatitis. We do not recommend an allergen avoidance diet unless the relevance of this food for triggering an exacerbation of the disease has been clearly established.
4.2 Avoidance of Individual Provocation Factors
Often patients complain that there is no “causal” therapy of this disease. However, in the individual case, one has to think about “cause” and “trigger factor” in daily life. The latter can very well be diagnosed and often be avoided in the sense of a causal therapy. This procedure, often called allergen avoidance, relies upon the results of careful allergy diagnostics (see Sect. 4.1). The recommendations regarding avoidance of individual provocation factors comprise much more; unspecific and specific stimuli often go together in the maintenance of severe eczema (Fig. 4.5).
Fig. 4.5
Individual trigger factors of eczema flares (With friendly permission of C. Schnopp and C. Kugler, Arbeitsgemeinschaft Neurodermitisschulung)
4.2.1 Avoidance of Unspecific Irritants
Various influences and noxious substances from the environment are able to irritate the sensitive skin of patients with atopic dermatitis compared to healthy persons and trigger eczema flares (Table 4.5).
Table 4.5
Atopic dermatitis: nonspecific irritants
Physical | For example, mechanical, exsiccation, UV light, temperature |
Chemical | Detergents, solvents, acids, alkali |
Pharmacologic | Vasoactive substances (alcohol, nicotine, amines) |
Immunologic | Allergens, superantigens |
Psychologic | Stress, emotional conflicts |
There are leaflets explaining these phenomena which should be given to the patients although this information is often regarded as trivial. Very often we see that especially in this so simple field of avoidance of irritants, heavy mistakes are made. People very early choose strong and possibly risky drugs before they even tried to start with simple avoidance of irritants and skin care. In our leaflet for patients (Table 4.6), we try to explain the importance of many so-called trivial things. A leaflet never replaces the dialogue which is very time-consuming and practically not achievable in the average office time of a practicing physician.
Table 4.6
Information leaflet for patients with atopic dermatitis
The disease is based on a genetic predisposition which can become manifest either as eczema, bronchial asthma, or allergic rhinoconjunctivitis, e.g., hay fever |
The skin of patients with atopic dermatitis is dry, and the hair relatively brittle |
There is an increased tendency to develop eczema, that is, red, squamous, itchy, sometimes oozing skin changes (the latter predominantly occur on the elbows, knee joints, hands, neck, and face) |
The skin of children or adults with atopic dermatitis needs continuous care. The following aspects have to be considered: |
Use mild detergents or soaps or syndets for cleaning |
Avoid too often or too hot showering; no foam bath |
Before showering or bathing, emollient additive (bath oil) should be given |
After bathing or showering, the skin has to be creamed with emollients (lotion cream) prior to using the towel which should only be used as a mild touch, not as an intense rubbing! |
Wool or irritant textiles never should get in direct contact with the skin (preferably use cotton or silk) |
It is important that skin care is performed in the morning and in the evening in order to avoid itchy eczematous reactions |
When there are red itchy or eczematous skin reactions, a doctor should be consulted, or anti-inflammatory therapy should be started |
The treatment of itch is crucial. Itch and the automatically connected scratch reaction cannot be forbidden! The side effects of an anti-inflammatory treatment are definitely less damaging than the damage through injuring the skin by scratching. Especially children with strong itch should find sympathetic parents and teachers. Occasionally children who have problems in school need a special colloquium with the teachers in order to get the necessary understanding |
Patients with atopic eczema principally can eat everything. In individual cases there is hypersensitivity against certain foods which have to be tested specifically. There is no general anti-eczema or anti-allergy diet. Obesity should be avoided. Newborns at risk should be breastfed if possible over 4 months. If this is not possible, hypoallergenic formula should be given |
Pets (cats, dogs, birds, etc.) as well as house dust (old carpets, skirts, etc.) may lead to exacerbation of the disease. The living room should have normal humidity (less than 55 %) |
Sea or high-altitude climate (above 1500 m) is well tolerated. Some rehabilitation programs in these climate zones can be helpful |
Therefore, this is a domain of eczema school and educational programs (see Chap. 6).
4.2.2 Nonspecific Procedures
Apart from adequate skin care (see Sect. 4.3), the consideration of certain principles regarding hygiene and clothing plays an important role (Ricci et al. 2004).
The so-called wool hypersensitivity of many patients is rarely based on a true allergy against sheep wool, but rather as typical marker of patients with atopic diseases shows the increased sensitivity of the skin to the mechanical stimulus of the small fibers.
Negative influences of environmental pollutants are also to be considered, like environmental tobacco smoke (also passive) as well as traffic exhaust. Also chemicals in indoor air, like volatile organic compounds or formaldehyde, can lead to deterioration of eczema (Huss-Marp et al. 2007; Eberlein-König et al. 1998).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree