CHAPTER 32 Management of Osteochondral Lesions of the Talus
SURGICAL APPROACHES TO OSTEOCHONDRAL LESIONS OF THE TALUS
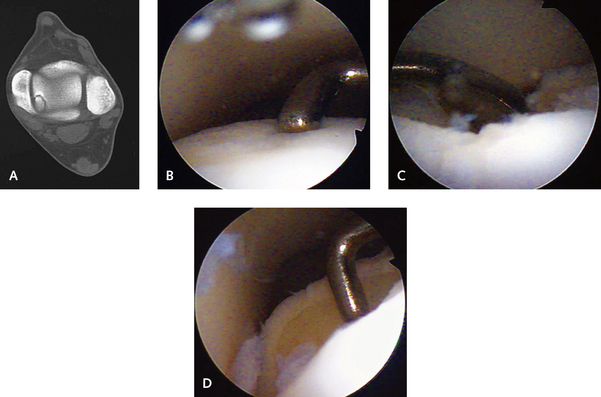
I generally initiate treatment arthroscopically, with abrasion, drilling, and microfracture (Figure 32-1). For lesions that are large and those that have not responded to arthroscopic treatment, use of an osteochondral graft should be considered. Moderate-size defects can be filled with several small osteochondral autografts from the ipsilateral knee. Larger defects, particularly those involving the medial or lateral talar wall, may require an allograft. These marginal sidewall lesions are difficult to treat with an osteochondral autograft because the graft must be inserted perpendicular to the axis of the talar dome. With these marginal defects, a medial or lateral malleolar osteotomy must be performed.
APPROACH TO LATERAL TALAR DOME LESIONS
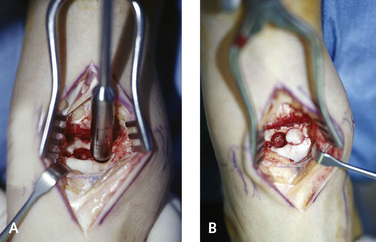
Most lateral talar dome lesions have a more anterior location, and if a graft is to be used, an anterolateral incision plus arthrotomy is used. The incision begins over the anterolateral aspect of the ankle, 2 cm proximal to the ankle joint, and is extended distally by 4 cm over the ankle joint (Figure 32-2). The intermediate dorsal cutaneous branches of the superficial peroneal nerve should be identified and protected. The extensor retinaculum is incised, the extensor digitorum longus tendon is identified and retracted medially, and the joint capsule is incised in line with the incision. Slight plantarflexion of the ankle will further facilitate exposure for access to debridement or grafting (Figure 32-3).
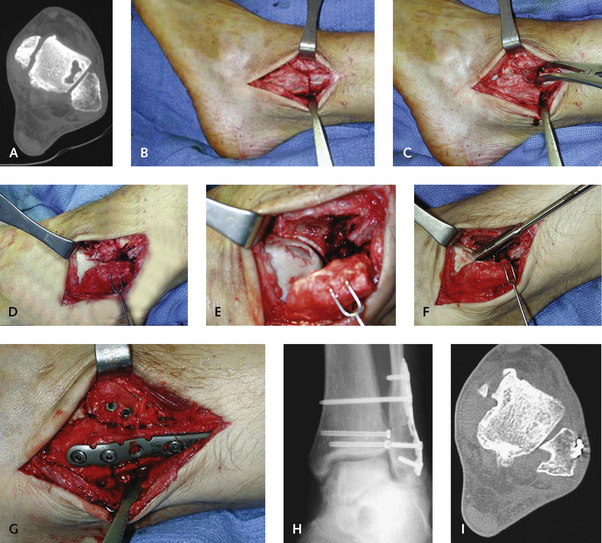
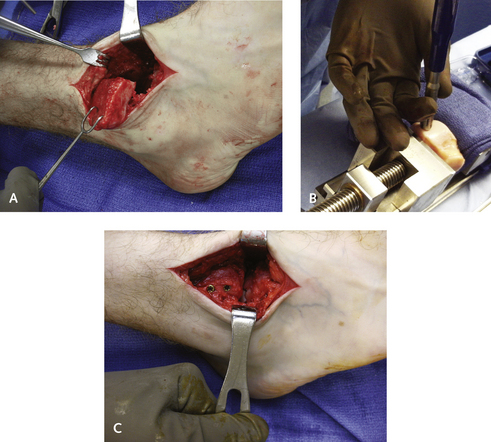
A fibular osteotomy is rarely necessary to treat a lateral talar dome lesion and is used only for very large lesions that are located centrally or posterolaterally and that cannot be accessed with arthrotomy (Figure 32-4). If a fibular osteotomy is required, then I use a 6-cm incision over the distal fibula, starting from 1 cm distal to the joint and extending proximally. The osteotomy cut is made with a microsagittal saw, oriented obliquely at an angle from lateral and proximal to distal and medial, so that the distal edge is at the level of the joint line. The advantage of the oblique osteotomy is the greater surface area for healing, as well as preservation of the interosseous ligaments. The lesion is unlikely to be visible or accessible once the osteotomy has been performed. In the rare instance in which the lateral lesion has a more central location and cannot be accessed by simply inverting the ankle, an anterolateral tibial osteotomy, in addition to the fibular osteotomy, can provide excellent visualization of the lesion.
For large cystic anterolateral lesions, an osteotomy of the fibula is not enough, and an osteotomy of the anterior tibia will be needed for exposure of the defect, as shown in Figure 32-5. In the case illustrated, a massive defect of the anterior talus was in a more central location and therefore inaccessible for grafting with the arthrotomy alone. The treatment plan was to use an osteoarticular allograft to fill the defect, but because the graft had to be inserted perpendicular to the axis of the talus, a tibial osteotomy was necessary. The osteotomy was made in an oblique plane (as a large fracture of the anterolateral distal tibia); 90% of the cut was made with a saw, with completion achieved by fracturing the tibia using an osteotome. The osteotomized bone was then peeled laterally, retaining the soft tissue attachments including the anterior inferior syndesmotic ligament (see Figure 32-5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree