CHAPTER 5 Management of Complications After Correction of Hallux Valgus
GENERAL PRINCIPLES OF MANAGING COMPLICATIONS
In any case, the following general principles should be addressed in surgical planning:
NONUNION
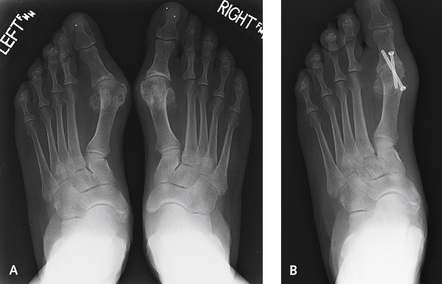
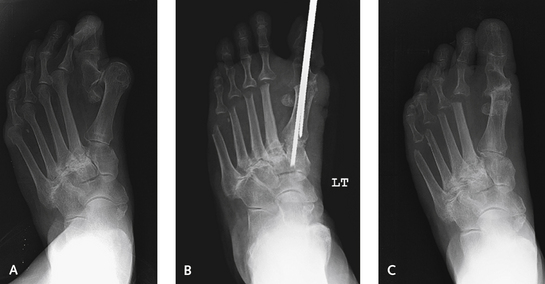
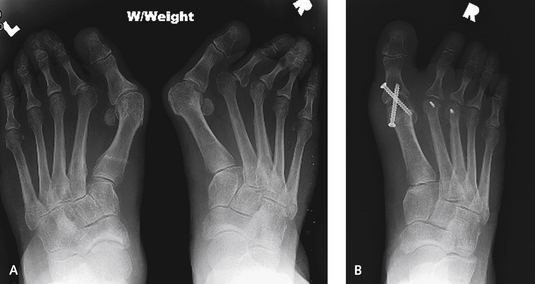
During the operation, the surgeon must establish the correct length of the metatarsal with a laminar spreader after debridement at the osteotomy nonunion site (Figure 5-7). In restoring length to the metatarsal, it is important to ensure that too much stress is not present on the hallux MP joint, because this will decrease motion of the hallux considerably. Once I have stretched the metatarsal back out to its appropriate length, multiple Kirschner wires (K-wires) are inserted transversely among the first, second, and third metatarsals to stabilize the first metatarsal in the desired position while fixation options are explored. The same applies to repair of a malunion or nonunion of the metatarsal head after a distal metatarsal osteotomy, although here, the risk of stiffness is markedly increased. Salvage of a distal metatarsal nonunion must be considered as an alternative to an arthrodesis. If arthrodesis is performed, however, most of the metatarsal head will need to be excised, and a very large bone graft must be used to restore length. For this reason, I am always prepared to attempt salvage of the distal metatarsal nonunion with restoration of length, and then, if painful arthritis develops, to perform an arthrodesis later on (Figure 5-8
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree