Chapter 45 Malignant melanoma
DevCan: Probability of developing or dying of cancer software, version 6.2.1, Statistical Research and Applications Branch, NCI, 2007. Available at: http://srab.cancer.gov/devcan. Accessed July 28, 2010.
Tucker MA: Melanoma epidemiology, Hematol Oncol Clin North Am 23:383–395, 2009.
Meyle KD, Guldberg P: Genetic risk factors for melanoma, Hum Genet 126:499–510, 2009.
Genetic factors include past medical history of melanoma, familial medical history of melanoma in a first-degree relative, Fitzpatrick type I or II skin, large congential nevi, the presence of dysplastic (atypical) nevi, >50 benign nevi (>2 mm in size), xeroderma pigmentosum, and familial dysplastic mole syndrome (FDMS). In FDMS, which is defined as occurring in families with atypical nevi and two or more blood relatives with melanoma, the estimated prevalence of melanoma approaches 85% by age 48. It is noteworthy that variations in the melanocortin receptor 1 (MCR1) gene, which is a component of pigment diversity, also confer an increased risk of melanoma. Variants differ in their associations with melanoma and nonmelanoma skin cancer, but both red hair and non–red hair variants confer increased risk.
Friedman RJ, Farber MJ, Warycha MA, et al: The “dysplastic” nevus. Clin Dermatol 27:103–115, 2009.
Elder, DE: Dysplastic nevi: an update, Histopathology 56:112–120, 2010.
La Porta C: Cancer stem cells: lessons from melanoma, Stem Cell Rev 5(1):61–65, 2009.
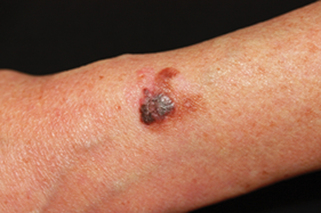
Key Points: Diagnosis of Malignant Melanoma
Bauer J, Bastian B: Genomic analysis of melanocytic neoplasia, Adv Dermatol 21:81–99, 2005.
Miller AJ, Mihm MC: Melanoma, N Engl J Med 355:51–65, 2006.
Campos-do-Carmo G, Ramos-e-Silva M: Dermoscopy: basic concepts, Int J Dermatol 47:712–719, 2008.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree