CHAPTER 15 Lichen Planus
Lichen planus is a relatively common disease that exhibits multiple morphologies, depending upon the location and severity.
Epidemiology and clinical manifestations
Formerly believed to be very uncommon, vulvovaginal lichen planus is now either recognized much more often or has become more common. Lichen planus of any site occurs in about 1% of people, and approximately 57% of women with oral lichen planus exhibit vulvovaginal disease, which is often asymptomatic1,2.
Vulvovaginal lichen planus occurs in several different morphologic forms and individual patients often present with several variants concomitantly (Table 15.1). These include erosive disease; white, reticulate lacy striae; sheets of white epithelium; and, on nonmucous membrane skin, red, or dusky red-brown papules.
Table 15.1 Usual Morphologic Variants of Vulvovaginal Lichen Planus
| Mucous membrane/modified mucous membrane disease |
| Keratinized cutaneous lichen planus |
Most common on vulvovaginal skin is erosive lichen planus, which exhibits characteristic but nonspecific symptoms and signs. Patients generally report introital irritation, burning, superficial dyspareunia, and, sometimes, itching. About two-thirds of women with erosive genital lichen planus experience oral lichen planus usually associated with oral pain3. On physical examination, erosive lichen planus typically exhibits relatively well-demarcated vestibular erosions, with late disease manifested by scarring and resorption of normal landmarks (Figures 15.1–15.3). Many women also experience erosions of the labia minora, medial labia majora, and any area of the modified mucous membranes (Figure 15.4). Agglutination of the labia minora is common, as are adhesions which bury the clitoris. Erosive disease sometimes produces midline fusion of the vestibule, with resultant narrowing of the introitus (Figure 15.5). Rectal involvement is common (Figure 15.6).

Figure 15.6 Perianal lichen planus is common, and is morphologically similar to vulvar lichen planus.
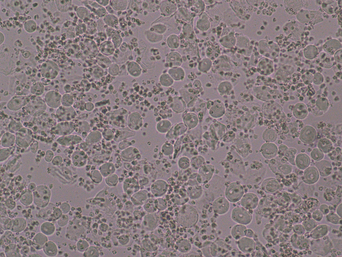
Erosive vulvar lichen planus is usually accompanied by vaginal and oral lichen planus, the “vulvovaginal–gingival syndrome.” Erosive vaginal lichen planus presents as superficial vaginal erosions or deep vaginal redness. Vaginal secretions are grossly and microscopically purulent (Figure 15.7). The yellowish or green discharge microscopically shows multiple white cells (mostly neutrophils), parabasal and basal cells (immature epithelial cells) shed from the base of erosions, and a marked decrease in lactobacilli, leading to an alkaline pH. Just as vulvar lichen planus results in scarring, synechiae of the vagina sometimes occur, occasionally resulting in complete closure of the vagina.
An examination of the mouth of a woman with erosive vulvovaginal lichen planus usually reveals white, lacy papules and striae and/or erosions on the posterior buccal mucosae (Figure 15.8). Often, women with erosive vulvovaginal lichen planus experience associated erosions and intense redness of the gingivae (Figure 15.9). The tongue is sometimes involved, with white, hyperkeratotic surface epithelium and/or erosions (Figure 15.10). Esophageal erosive lichen planus is becoming more recognized and can produce strictures that interfere with swallowing4.
A second morphological presentation of vulvovaginal lichen planus is the classic, lacy, white epithelium (Figures 15.11 and 15.12). Although this classic mucosal lichen planus is much less common than erosive lichen planus, this form is pathognomonic for lichen planus. This manifestation is characterized by white striae, often forming fern-like or reticulate plaques. These distinctive plaques are frequently accompanied by vaginal lichen planus. Oral lichen planus occurs in this setting as well.
Fairly often, mucosal vulvar lichen planus is characterized by a third morphology, that of uniformly white epithelium which often surrounds erosions (Figures 15.13 and 15.14). White lesions of lichen planus, whether fern-like or solid, are always located on mucous membrane or moist modified mucous membrane skin rather than on dry, keratinized skin. Women with white papules and plaques are most likely to experience itching.

Figure 15.14 These white plaques surrounding mucous membrane erosions are typical but not specific for lichen planus.
Yet another morphology of lichen planus occurs on dry, keratinized skin, presenting as dusky red, flat-topped, shiny papules (Figure 15.15). Extragenital lichen planus can occur almost anywhere, although facial involvement is extraordinarily uncommon. Only about 3–5% of women with erosive vulvovaginal lichen planus experience nonmucous membrane disease.
Diagnosis and differential diagnosis
The differential diagnosis of lichen planus depends upon the presenting morphology. Erosive lichen planus most closely resembles mucosal blistering diseases, because the fragile blisters on mucosal surfaces erode as they form, leaving nonspecific erosions (Table 15.2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree