10 Laser treatment of ethnic skin
Summary and Key Features
• The use of lasers and lights can be safe and effective in ethnic skin
• Sun protection pre- and post-treatment, together with the use of bleaching agents, is important in reducing the risks of post inflammatory hyperpigmentation
• Q-switched and long pulsed lasers are both useful in the treatment of epidermal pigmentation; however, in ethnic skin, long-pulsed lasers are preferred as they have similar efficacy with less side effects
• Using a small spot size avoids inadvertent treatment of surrounding normal skin, which can increase the risk of hyperpigmentation when the contrast between lesional and non-lesional skin is low
• Diascopy during treatment of pigmented lesions reduces the risk of vascular damage
• Longer wavelength lasers allow for dermal pigmentation to be treated
• Q-switched 1064 nm Nd : YAG laser, in conjunction with 1550 nm fractional resurfacing, can achieve optimal results in the treatment of nevus of Ota
• Hori’s macules can be resistant to treatment, requiring multiple treatments. There is also a risk of initial darkening of pigmentation before subsequent lightening with further treatments
• Melasma is a common pigmentary condition in ethnic skin and a challenge to treat. Topical bleaching agents should be used before laser therapy is considered
• Non-ablative fractional resurfacing using lower densities but increasing the number of treatment sessions is recommended for ethnic skin
Treatment of epidermal pigmentation
Freckles and lentigines
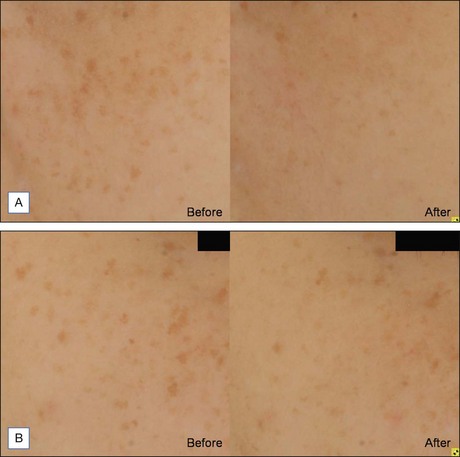
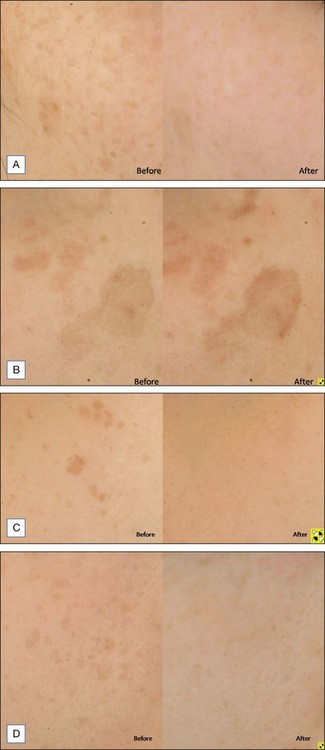
As melanin has a broad absorption spectrum ranging from 250 to 1200 nm, various lasers have been used to target cutaneous pigmentation, usually with excellent results. Anderson et al were the first to demonstrate the effectiveness of Q-switched (QS) lasers in the treatment of cutaneous pigmentation. Frequency-doubled QS neodymium : yttrium-aluminum-garnet (Nd : YAG), QS ruby, and QS alexandrite lasers with respective wavelengths of 532 nm, 694 nm, and 755 nm, have all been used with good results in lighter-skinned patients but PIH risk of 10–25% has been reported when used on ethnic skin. Chan et al compared 532 nm frequency-doubled Nd : YAG lasers with different pulse durations in the treatment of facial lentigines in Chinese patients, and found similar efficacy between QS 532 nm Nd : YAG and long pulsed (LP) 532 nm Nd : YAG, but a higher risk of postoperative hyperpigmentation with the QS device. A recent study by our group comparing QS and LP alexandrite for the treatment of freckles and lentigines in 20 Chinese patients showed similar results (Fig. 10.1). There was significant improvement in pigmentation in both groups, with no difference between the groups. However, the risk of PIH was 22% in the QS group, compared with 6% in the LP group. Patients also complained of more severe pain, erythema, and edema with the QS device. These findings were further validated in a retrospective study due to be published, comparing treatment of lentigines in 40 Chinese patients with four different devices; 595 nm long pulsed dye laser (LPDL), 755 nm alexandrite laser, 532 nm QS Nd : YAG, and 532 nm LP potassium-titanyl-phosphate (KTP) laser (Fig. 10.2). The results showed that a long pulse laser and small spot size appear to reduce the risk of PIH in darker skin types (see Case study 1 at end of chapter).
A treatment algorithm for epidermal pigmentation is as follows:
1. IPL can be recommended for patients who are intolerant of any PIH risk, and are amenable to having several treatment sessions.
2. LP lasers are effective, yet require fewer treatments than IPL, and carry a low PIH risk.
3. The more aggressive approach using QS lasers only requires one to two sessions, but carries the highest risk of PIH and downtime of a week. This should be reserved for patients with time and cost constraints.
Treatment of dermal pigmentation
Nevus of Ota
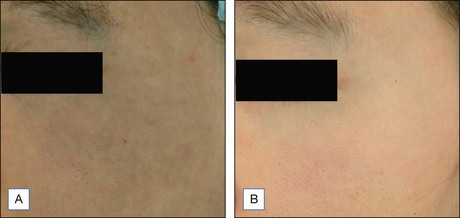
Nevus of Ota is an oculodermal melanocytosis affecting approximately 0.6% of the Asian population at birth or developing in their teens. Clinically, it presents as a bluish-black hyperpigmentation along the ophthalmic or maxillary branches of the trigeminal nerve. QS lasers, including QS ruby, QS alexandrite, and QS 1064 nm Nd : YAG, have all been used to achieve good therapeutic results.Watanabe and Takahashi looked at 114 nevus of Ota patients treated with QS Ruby and reported a good to excellent degree of lightening after three or more sessions. Kono et al confirmed the findings when he reviewed 101 nevus of Ota patients treated with QS Ruby and reported 56% achieving 75% improvement, and 36% achieving complete clearing. Hypopigmentation was seen in 17% of patients and hyperpigmentation in 6%. Studies comparing the use of QS alexandrite and QS 1064 nm Nd : YAG found the former better tolerated but the latter more effective after three or more treatment sessions. The longer wavelength of the QS Nd : YAG targets dermal pigment effectively with minimal epidermal damage in darker skinned individuals (Fig. 10.3). More recently, fractionated laser technology has been added to the currently available options. Near-complete clearance of a case of nevus of Ota after serial therapy using 1064 nm QS Nd : YAG, followed by 1550 nm non-ablative fractionated erbium-doped fiber laser treatments at 2-month intervals; and a further case achieving complete clearance with sequential same day therapy with the same devices have been reported. Treatment of nevus of Ota at a younger age requires fewer treatment sessions and is associated with fewer complications compared with older patients, and early treatment is therefore recommended (see Case study 2). It is important to note that the risk of recurrence is estimated to be between 0.6% and 1.2%8, which has important implications particularly when counseling pediatric patients.