7 Laser resurfacing
Summary and Key Features
• Laser resurfacing is a very popular procedure
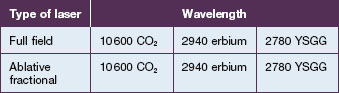
• A variety of carbon dioxide, Er : YAG and yttrium-scandium-gallium-garnet (YSGG) lasers are included in this category
• Full field means 100% of the treated area is removed to the selected depth
• Fractional means discontinuous portions of the treated area are removed
• Recovery time is linked to amount of damage created
• Fractional treatments have less downtime than full field treatments
• Experience with these lasers is important to outcomes
• Post-treatment care is very important
• Complications can arise with all of these laser treatments
Introduction
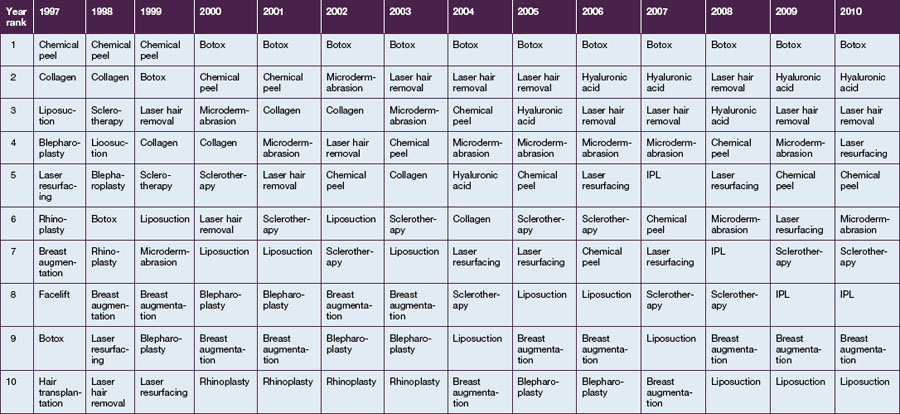
Laser resurfacing is a very popular procedure in the United States and worldwide. Data from The American Society of Aesthetic Plastic Surgery collected yearly from core specialists since 1997 through 2010 has shown the rise, fall, and rise again of this procedure as devices have been introduced (Table 7.1). In the mid 1990s carbon dioxide lasers were extremely popular, but toward the turn of the century they fell out of favor and were somewhat replaced by non-ablative technology. Laser resurfacing resurged in the last 5 years with the introduction of fractional lasers.
History
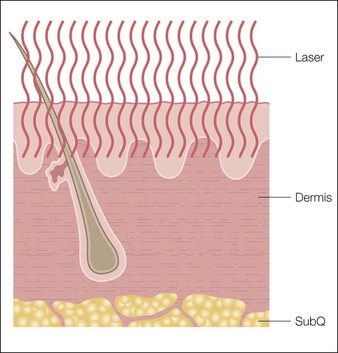
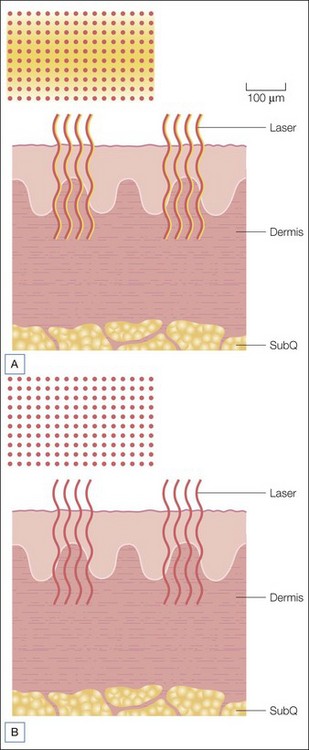
In 2004 Manstein et al introduced the concept of fractional photothermolysis. Full field or traditional laser resurfacing as described above removes the entire skin surface in the area being treated with depth of injury depending upon energy level, whereas fractional laser resurfacing treats a small ‘fraction’ of the skin at each session, leaving skip areas between each exposed area (Fig. 7.1). This was first performed commercially using non-ablative fluences at 1550 nm (Solta Medical, Mountain View, CA). These non-ablative fractional lasers created a column of thermal damage with intact epidermis. Healing occurred from deeper structures as well as from adjacent structures. This differs from full field resurfacing in which healing occurred from only deeper structures. Deeper treatments (i.e. to the reticular dermis) can safely be performed using this approach than would be tolerated using a full field treatment. Advantages of this approach include avoidance of an open wound and very low risk of pigment disturbance or scarring. Disadvantages have included the need for multiple treatments and somewhat less clinical response than with full field ablative resurfacing. Since the introduction of the original system there have been many manufacturers that have introduced similar non-ablative fractional devices with wavelengths of 1440 nm, 1540 nm, and 1550 nm. These devices differ in power output, spot size, density, etc. and comparisons of clinical efficacy are difficult, yet similar degrees of tissue injury should produce similar clinical results.
Fractional ablative resurfacing with carbon dioxide, erbium, and yttrium-scandium-gallium-garnet (YSGG) systems was introduced with the intent of providing more significant results than non-ablative fractional systems while achieving shorter healing times and complications when compared with full field ablative systems (Fig. 7.2). These devices differ not only in wavelength but in system power, spot size, and amount of thermal damage created adjacent to and deep to the ablated hole. One popular erbium system, the Sciton ProFractional®, allows one to vary the amount of thermal damage similarly to their full field system. Other newer carbon dioxide fractional lasers allow variation of the thermal damage zones (Deka Medical) while others allow superficial and deeper penetration with a single scan (Syneron, Yokneum, Israel). As with the non-ablative fractional systems, direct comparison between devices is difficult as devices differ in power output, spot size, density, and degree of thermal damage, but similar degrees of injury should produce similar clinical results.
Expected benefits and alternatives
Pearl 5
The potential for improvement depends upon the device used and depth and degree of injury produced.
Lasers and technical overview
As discussed above, current devices used for ablative laser resurfacing include carbon dioxide, Er : YAG, and YSGG lasers, in both full field and fractional modes, and non-ablative devices in a variety of wavelengths including 1440 nm, 1540 nm, 1550 nm, and 1927 nm (Table 7.2). Some machines offer upgradeable expandable platforms where full field devices and fractional devices are available in one machine whereas other companies offer only isolated full field or fractional devices.