4 Laser hair removal
Summary and Key Features
• Laser hair removal is the most commonly requested cosmetic procedure in the world
• The extended theory of selective photothermolysis enables the laser surgeon to target and destroy hair follicles, thereby leading to both permanent and temporary hair removal
• The ideal candidate for laser hair removal (LHR) is fair skinned with dark terminal hair; however, LHR can today be successfully performed in all skin types
• Thin hairs and hairs with white, blond and red color are extremely difficult to treat with laser hair removal devices
• Wax epilation should be avoided prior to laser hair removal treatments
• Lasers pose a safety risk to both the patient and device operator
• Informed consent should be reviewed with every patient prior to treatment
• Wavelengths, spot size, pulse duration, and skin cooling are key variables that can be used to tailor laser–tissue interactions for a given patient
• Roughly 15–30% of hairs can be removed with each treatment session using ideal parameters. Remaining hairs are often thinner and lighter in color
• The most common complication is pigmentary alteration, which can be temporary or permanent
Basic hair biology
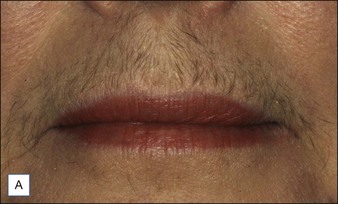
The hair follicle is a hormonally active structure (Fig. 4.1) that is anatomically divided into an infundibulum (hair follicle orifice to insertion of the sebaceous gland), isthmus (insertion of the sebaceous gland to the insertion of the arrector (erector) pili muscle), and inferior (insertion of the arrector pili to the base of the hair follicle) segments. The dermal papilla provides neurovascular support to the base of the follicle and helps form the hair shaft.
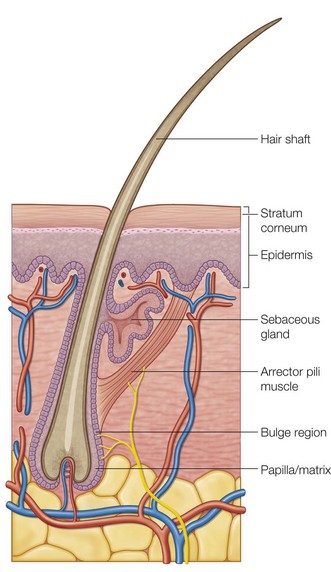
Figure 4.1 Hair follicle anatomy.
Reproduced from Tsao SS, Hruza GJ 2005 Laser hair removal. In: Robinson JK, Hanke CW, Sengelmann RD, Siegel DM (eds) Surgery of the Skin. Elsevier Mosby, Philadelphia, p 575-588.
Mechanism of LHR
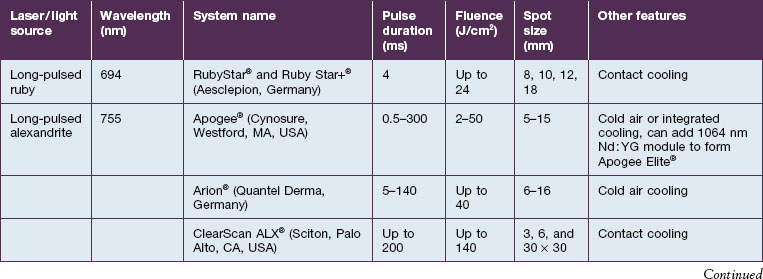
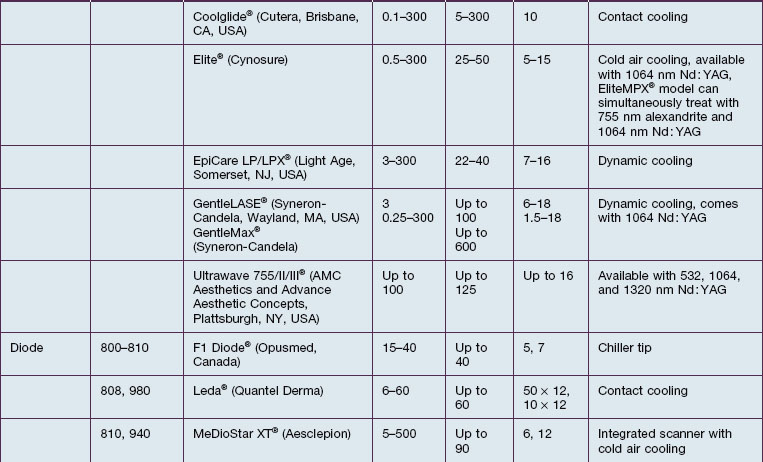
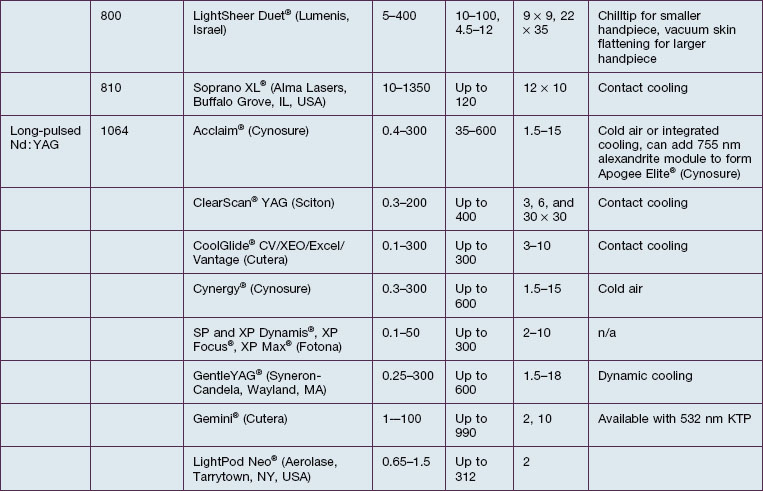
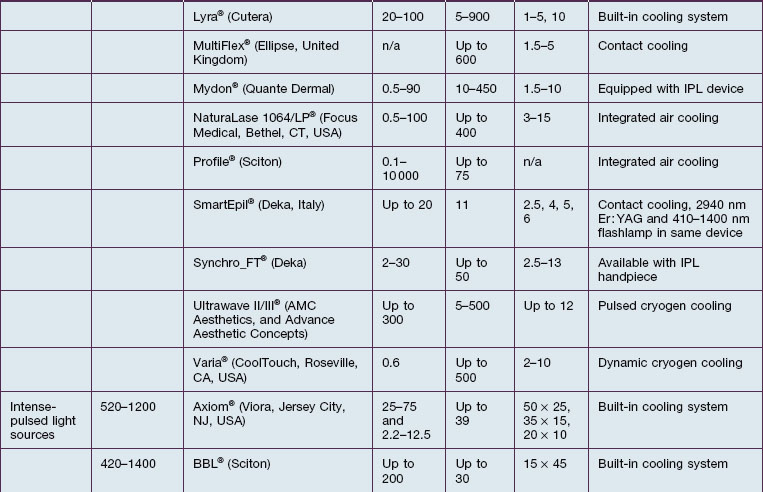
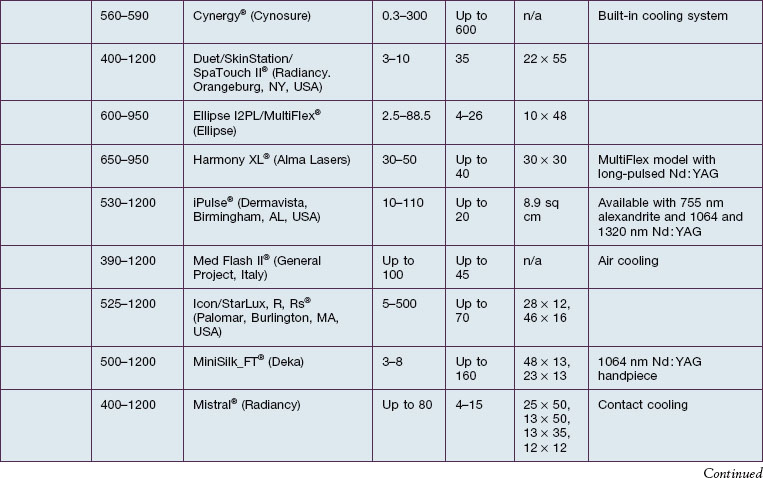
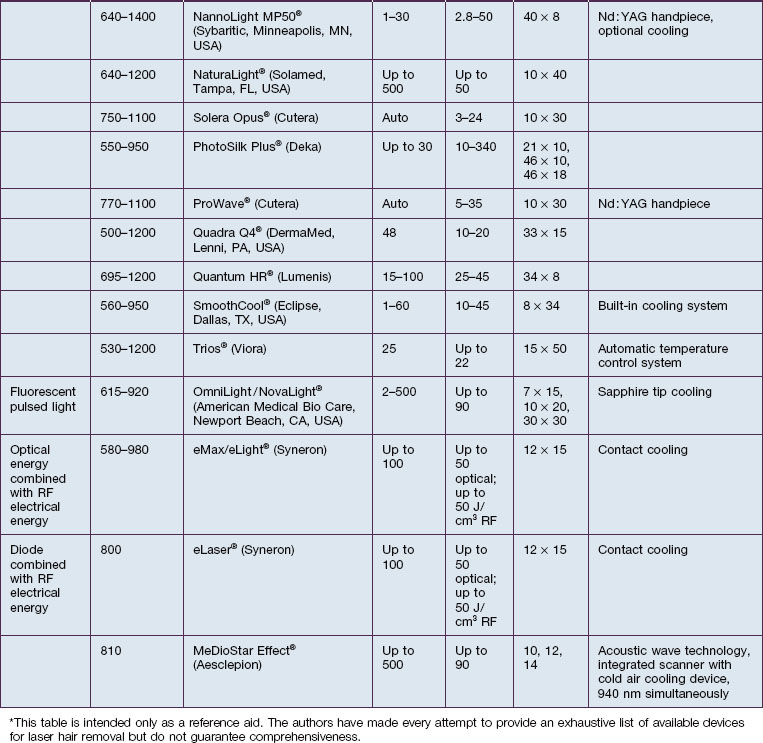
The theory of selective photothermolysis enables precise targeting of pigmented hair follicles by using the melanin of the hair shaft as a chromophore. Melanin has an absorbance spectrum that matches wavelengths in the red and near-infrared (IR) portion of the electromagnetic spectrum. To achieve permanent hair removal, the biological ‘target’ is the follicular stem cells located in the bulge region and / or dermal papilla. Due to the slight spatial separation of the chromophore and desired target, an extended theory of selective photothermolysis was proposed that requires diffusion of heat from the chromophore to the desired target for destruction. This requires a laser pulse duration that is longer in duration than if the actual chromophore and desired target are identical. Temporary LHR can result when the follicular stem cells are not completely destroyed, primarily through induction of a catagen-like state in pigmented hair follicles. Temporary LHR is much easier to achieve than permanent removal when using lower fluences. Long-term hair removal depends on hair color, skin color, and tolerated fluence. Roughly 15–30% long-term hair loss may be observed with each treatment when optimal treatment parameters are used (Fig. 4.2). A list of laser and light devices that are currently commercially available for hair removal is given in Table 4.1.
Key factors in optimizing treatment
Patient selection
A focused medical history, physical examination, and informed consent, including setting realistic expectations and potentials risks, should be performed prior to any laser treatment (Box 4.1). Patients with evidence of endocrine or menstrual dysfunction should be appropriately worked up. Similarly, patients with an explosive onset of hypertrichosis should be evaluated for paraneoplastic etiologies. Treatment of a pregnant woman for non-urgent conditions is discouraged by the authors, although there is no evidence suggesting a potential risk to pregnant women undergoing LHR. The past medical history should be reviewed to identify patients with photosensitive conditions, such as autoimmune connective tissue disorders, or disorders prone to the Koebner phenomenon. A history of recurrent cutaneous infections at or in the vicinity of the treatment area might warrant the use of prophylactic medications. Any past history of keloid or hypertrophic scar formation should be elicited as well. Previous hair removal methods, including past laser treatments, should be reviewed. Any methods of hair shaft epilation (e.g. waxing or tweezing) that entirely remove the target chromophore render LHR less effective for at least 2 weeks. Although there is little evidence for the time frame a patient must wait after complete epilation of the hair shaft and laser treatment, we recommend a minimum of 6 weeks. Shaving and depilatory creams can be used up to the day of laser treatment as they do not remove the entire hair shaft.
Box 4.1
Pertinent medical history for laser / pulsed light hair removal
 Presence of conditions that may cause hypertrichosis:
Presence of conditions that may cause hypertrichosis:
 Drugs (i.e. corticosteroids, hormones, immunosuppressives, self or spousal use of minoxidil)
Drugs (i.e. corticosteroids, hormones, immunosuppressives, self or spousal use of minoxidil)
 History of local or recurrent skin infection
History of local or recurrent skin infection
 History of herpes simplex, especially perioral
History of herpes simplex, especially perioral
 History of herpes genitalis, important when treating the pubic or bikini area
History of herpes genitalis, important when treating the pubic or bikini area
 History of keloids / hypertrophic scarring
History of keloids / hypertrophic scarring
 History of koebnerizing skin disorders such as vitiligo and psoriasis
History of koebnerizing skin disorders such as vitiligo and psoriasis
 Previous treatment modalities – method, frequency, and date of last treatment, as well as response
Previous treatment modalities – method, frequency, and date of last treatment, as well as response
 Recent suntan or exposure to tanning or light cabinet
Recent suntan or exposure to tanning or light cabinet
 Onset of hair regrowth (recent)
Onset of hair regrowth (recent)
 Patient’s hobbies or habits which might interfere with treatment
Patient’s hobbies or habits which might interfere with treatment
The physical exam should corroborate the patient’s Fitzpatrick skin phototype. This will help determine which lasers and light sources are safe to use for that patient (see Table 4.1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree