Chapter 2 Laparoscopic Ventral Hernia Repair—Standard ![]()
1 Surgical Anatomy
 The laparoscopic repair of ventral hernia borrows from the open technique espoused by Rives and Stoppa. It maintains the tenets of large mesh overlap with transabdominal fixation of the prosthetic. In a standard laparoscopic ventral herniorrhaphy, the biomaterial is placed intraabdominally in juxtaposition to the underlying viscera; therefore, a tissue-separating mesh is required. Traditionally, the hernia defect is bridged with mesh; however, some authors have described reapproximating the midline by closing the defect with transabdominal sutures.
The laparoscopic repair of ventral hernia borrows from the open technique espoused by Rives and Stoppa. It maintains the tenets of large mesh overlap with transabdominal fixation of the prosthetic. In a standard laparoscopic ventral herniorrhaphy, the biomaterial is placed intraabdominally in juxtaposition to the underlying viscera; therefore, a tissue-separating mesh is required. Traditionally, the hernia defect is bridged with mesh; however, some authors have described reapproximating the midline by closing the defect with transabdominal sutures. The amount of mesh overlap required for a durable ventral hernia repair is unknown. Based on Pascal’s principle, the intraabdominal pressure is evenly distributed over a large surface area of mesh. The initial experience with laparoscopic ventral herniorrhaphy reported a 3-cm overlap of mesh, but the current recommendation is at least a 4- to 5-cm margin. The amount of overlap depends on the diameter of the largest hernia defect and the thickness of the patient’s abdominal wall. One large defect deserves at least 5 cm, whereas numerous small defects (i.e., Swiss cheese hernia) may only require 4 cm of additional mesh.
The amount of mesh overlap required for a durable ventral hernia repair is unknown. Based on Pascal’s principle, the intraabdominal pressure is evenly distributed over a large surface area of mesh. The initial experience with laparoscopic ventral herniorrhaphy reported a 3-cm overlap of mesh, but the current recommendation is at least a 4- to 5-cm margin. The amount of overlap depends on the diameter of the largest hernia defect and the thickness of the patient’s abdominal wall. One large defect deserves at least 5 cm, whereas numerous small defects (i.e., Swiss cheese hernia) may only require 4 cm of additional mesh. In a laparoscopic ventral hernia repair, the mesh is placed in an insufflated abdominal cavity. Ideally, there is a slight degree of tension on the mesh at the completion of the repair. The mesh does not lie flush against the underside of the abdominal wall. Rather, it transects the abdominal space, so that when the abdominal cavity is desufflated, the mesh will not occupy the hernia sac (Fig. 2-1).
In a laparoscopic ventral hernia repair, the mesh is placed in an insufflated abdominal cavity. Ideally, there is a slight degree of tension on the mesh at the completion of the repair. The mesh does not lie flush against the underside of the abdominal wall. Rather, it transects the abdominal space, so that when the abdominal cavity is desufflated, the mesh will not occupy the hernia sac (Fig. 2-1). There has been a lot of debate in the literature regarding the approach for ventral herniorrhaphy. Length of stay, postoperative pain, and operative times are essentially similar between the open and laparoscopic techniques in experienced hands. However, the laparoscopic technique consistently demonstrates significant reductions in wound and mesh infections. For this reason alone, the laparoscopic repair of ventral hernias should be the preferred approach when applicable.
There has been a lot of debate in the literature regarding the approach for ventral herniorrhaphy. Length of stay, postoperative pain, and operative times are essentially similar between the open and laparoscopic techniques in experienced hands. However, the laparoscopic technique consistently demonstrates significant reductions in wound and mesh infections. For this reason alone, the laparoscopic repair of ventral hernias should be the preferred approach when applicable.2 Preoperative Considerations
 When considering who is a candidate for a laparoscopic ventral hernia repair, certain patient characteristics must be considered. Contraindications include:
When considering who is a candidate for a laparoscopic ventral hernia repair, certain patient characteristics must be considered. Contraindications include: Surgeon skill, particularly in the area of adhesiolysis, needs to be factored in when making the choice for a laparoscopic ventral hernia repair. Factors that portend a more difficult case requiring experience with the technique include:
Surgeon skill, particularly in the area of adhesiolysis, needs to be factored in when making the choice for a laparoscopic ventral hernia repair. Factors that portend a more difficult case requiring experience with the technique include: The preoperative consultation is critical in the patient undergoing laparoscopic ventral herniorrhaphy. The procedure is painful and not much different from an open repair in terms of postoperative discomfort. The real benefit of the laparoscopic approach is the well-documented reduction in wound- and mesh-related infectious complications. The likelihood of postoperative seroma formation should be discussed. The need for conversion to an open repair and the possibility of an enterotomy should be considered as well. The anticipated options if an enterotomy occurs should be explained to include not repairing the hernia defect at all.
The preoperative consultation is critical in the patient undergoing laparoscopic ventral herniorrhaphy. The procedure is painful and not much different from an open repair in terms of postoperative discomfort. The real benefit of the laparoscopic approach is the well-documented reduction in wound- and mesh-related infectious complications. The likelihood of postoperative seroma formation should be discussed. The need for conversion to an open repair and the possibility of an enterotomy should be considered as well. The anticipated options if an enterotomy occurs should be explained to include not repairing the hernia defect at all. Ventral hernias usually can be identified on physical exam, and no further work up is required. Computed tomography (CT) of the abdominal wall can be helpful in the patient who is morbidly obese, has a recurrent hernia (particularly with intraabdominal mesh), demonstrates a defect in proximity to a bony structure (i.e. suprapubic, subxiphoid, flank defects), or has concern for loss of domain.
Ventral hernias usually can be identified on physical exam, and no further work up is required. Computed tomography (CT) of the abdominal wall can be helpful in the patient who is morbidly obese, has a recurrent hernia (particularly with intraabdominal mesh), demonstrates a defect in proximity to a bony structure (i.e. suprapubic, subxiphoid, flank defects), or has concern for loss of domain. Patients who have previous failed attempts at repair can be difficult. The reasons for recurrence are usually not known, but certainly, efforts should be made not to repeat errors of the past. Every effort to obtain all operative reports that pertain to prior hernia repairs should be made. Before embarking on a recurrent defect, the surgeon should feel extremely confident with adhesiolysis and have a low threshold to convert to open. Patients who have had previous mesh infections that required removal of the prosthesis pose an extremely difficult challenge.
Patients who have previous failed attempts at repair can be difficult. The reasons for recurrence are usually not known, but certainly, efforts should be made not to repeat errors of the past. Every effort to obtain all operative reports that pertain to prior hernia repairs should be made. Before embarking on a recurrent defect, the surgeon should feel extremely confident with adhesiolysis and have a low threshold to convert to open. Patients who have had previous mesh infections that required removal of the prosthesis pose an extremely difficult challenge. The preoperative orders consist of antibiotic and deep venous thrombosis prophylaxis. A first-generation cephalosporin is typically given, and the dose is adjusted for the morbidly obese. Because the ventral hernia patient is frequently obese, will be immobile postoperatively, and will experience increased intraabdominal pressure from pneumoperitoneum, sequential compression devices and subcutaneous heparin are employed preoperatively.
The preoperative orders consist of antibiotic and deep venous thrombosis prophylaxis. A first-generation cephalosporin is typically given, and the dose is adjusted for the morbidly obese. Because the ventral hernia patient is frequently obese, will be immobile postoperatively, and will experience increased intraabdominal pressure from pneumoperitoneum, sequential compression devices and subcutaneous heparin are employed preoperatively.3 Operative Steps
1 Patient Positioning
 For the majority of patients with defects in the midline, supine positioning with the arms tucked works well. The pressure points at the elbow and wrist should be padded (Fig. 2-2). For larger patients, the arm sleds may be required. In patients with defects off the midline or lumbar defects, a bump may be placed under the hip on the side of the hernia, or a true lateral position may be necessary with the aid of a bean bag.
For the majority of patients with defects in the midline, supine positioning with the arms tucked works well. The pressure points at the elbow and wrist should be padded (Fig. 2-2). For larger patients, the arm sleds may be required. In patients with defects off the midline or lumbar defects, a bump may be placed under the hip on the side of the hernia, or a true lateral position may be necessary with the aid of a bean bag. A Foley catheter is placed for bladder decompression and may be used to insufflate the bladder for identification in the repair of suprapubic defects. Gastric decompression is usually reserved for the patient requiring a difficult orotracheal intubation and may be achieved with orogastric tube decompression.
A Foley catheter is placed for bladder decompression and may be used to insufflate the bladder for identification in the repair of suprapubic defects. Gastric decompression is usually reserved for the patient requiring a difficult orotracheal intubation and may be achieved with orogastric tube decompression. An iodine-impregnated adhesive drape is applied to the skin of the prepped and draped patient. This protects the biomaterial from the patient’s skin flora.
An iodine-impregnated adhesive drape is applied to the skin of the prepped and draped patient. This protects the biomaterial from the patient’s skin flora.2 Gaining Abdominal Access
 Abdominal entry can be the most difficult step in the patient who has undergone multiple abdominal operations. Selecting the location for entry can be challenging because many of these patients have had numerous abdominal incisions. The upper quadrant at the tip of the eleventh rib is generally a safe place to gain access even in such cases. The side of entry should avoid previous incisions. For example, in the patient with an open cholecystectomy incision, the left upper quadrant should be chosen.
Abdominal entry can be the most difficult step in the patient who has undergone multiple abdominal operations. Selecting the location for entry can be challenging because many of these patients have had numerous abdominal incisions. The upper quadrant at the tip of the eleventh rib is generally a safe place to gain access even in such cases. The side of entry should avoid previous incisions. For example, in the patient with an open cholecystectomy incision, the left upper quadrant should be chosen. Several safe methods for initial access have been described. A cut-down technique works very well. Through a small incision in the upper quadrant, each layer of the abdominal wall is divided down to the peritoneum. The peritoneum can be sharply entered with a scalpel or bluntly penetrated with the finger to gain safe access to the abdominal cavity. The optical trocar can be used safely in the upper quadrant just below the rib line as well. Some surgeons prefer the Veress needle. The best technique is the one the surgeon is most comfortable and familiar with.
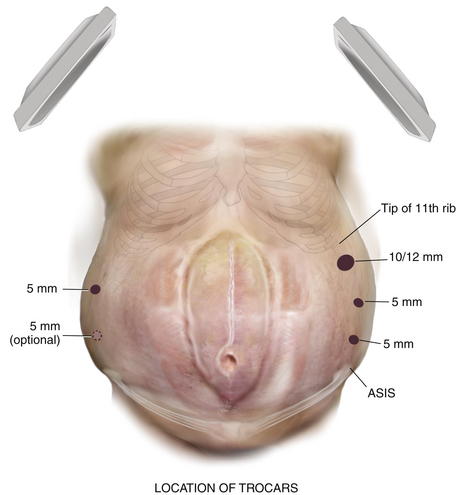
Several safe methods for initial access have been described. A cut-down technique works very well. Through a small incision in the upper quadrant, each layer of the abdominal wall is divided down to the peritoneum. The peritoneum can be sharply entered with a scalpel or bluntly penetrated with the finger to gain safe access to the abdominal cavity. The optical trocar can be used safely in the upper quadrant just below the rib line as well. Some surgeons prefer the Veress needle. The best technique is the one the surgeon is most comfortable and familiar with. Once initial entry into the abdominal cavity is achieved, at least one and preferably two additional trocars are placed laterally on the side of entry. Typically one can be placed above the initial site once pneumoperitoneum has been initiated, and an additional one can be inserted inferiorly with care not to be too close to the iliac crest. Two trocars are placed on the opposite side to provide additional viewing perspective for adhesiolysis and aid in retraction (Fig. 2-3).
Once initial entry into the abdominal cavity is achieved, at least one and preferably two additional trocars are placed laterally on the side of entry. Typically one can be placed above the initial site once pneumoperitoneum has been initiated, and an additional one can be inserted inferiorly with care not to be too close to the iliac crest. Two trocars are placed on the opposite side to provide additional viewing perspective for adhesiolysis and aid in retraction (Fig. 2-3).3 Adhesiolysis
 The Achilles’ heel of the laparoscopic ventral hernia repair is the lysis of adhesions. This step can be the most time consuming and usually determines the length and complexity of the case.
The Achilles’ heel of the laparoscopic ventral hernia repair is the lysis of adhesions. This step can be the most time consuming and usually determines the length and complexity of the case.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree