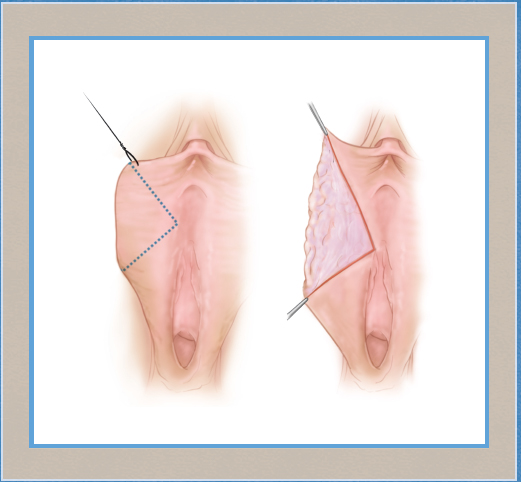
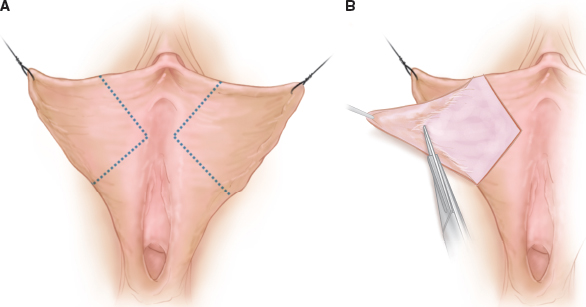
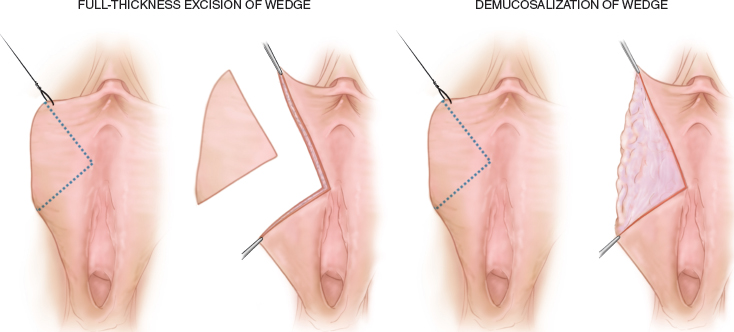
CHAPTER 4 • Labiaplasty by wedge reduction is a safe and effective procedure. • Wedge resection creates a small horizontal scar that is nearly imperceptible once healed. • The removal of excess labia minora with a wedge technique spares critical nerves and preserves arterial supply. • Patients tolerate the procedure well when given local anesthesia; it usually takes less than an hour to perform. • The use of low-temperature plasma radiofrequency cautery may help in wound healing and early recovery. • Complications such as edge notching, dehiscence, and hematoma are rare (see Chapter 10: Complications of Female Cosmetic Genital Surgery). Surgical alteration of the labia minora is the most frequently performed vaginal aesthetic procedure.1 Many published techniques describe decreasing the size of the labia minora. The most common two types are edge trim procedures and wedge resections. In 1998 Alter2 first described the wedge technique as a central wedge removed from the most protuberant portion of the labia minora. The advantages included preservation of the natural edge architecture, a shorter scar, and decreased scar sensitivity. In 2008 Alter3 reviewed his 2-year experience with 407 extended wedge labiaplasties. The technical modification narrowed the clitoral hood and minimized the dog-ear created with the wedge-only technique. The incidence of complications was low, and the patient satisfaction rate was high. Wedge techniques are best suited for patients with radial elongation of the labia and continuous edge pigmentation (Fig. 4-1). Basically, a simple “pie wedge” of full-thickness tissue is resected from the most protuberant portion of the labia minora, and the edges of the submucosa and mucosa are reapproximated. This pie wedge resection reduces the circumference thus reducing protrusion of the minora beyond the labia majora (Fig. 4-2). Fig. 4-2 A, Labia minora wedge resection markings. B, Excision of a wedge defect with preservation of the underlying submucosa. Fig. 4-3 This 49-year-old woman is shown before and 3 months after an extended wedge labiaplasty. Fig. 4-4 This 27-year-old woman has unilateral labia minora hypertrophy (submucosal thickening). Thicker labia from mucosal or submucosal redundancy are suitable for wedge resections (Figs. 4-3 and Figs. 4-4). Edge trimming in such patents is difficult, because debulking submucosa necessitates near amputation of the labia. This results in labial remnants that are quite short and no longer have the natural edge architecture (Fig. 4-5). The wedge procedure allows adjustment of the amount of submucosa resection, facilitating the removal of full-thickness submucosa in patients with very bulky labia. However, in patients with thin or atrophic labia, the submucosa is preserved in the tissue remaining after a wedge resection (Figs. 4-6 and 4-7). Patients with minimal submucosa are also well suited for wedge resection. Fig. 4-5 This 46-year-old woman is shown 10 months after having an edge resection labiaplasty. Fig. 4-6 This 44-year-old woman with thin, atrophic labia minora (minimal submucosa) is shown before and after an L-wedge resection by demucosalization. Fig. 4-7 A full-thickness wedge resection for thick labia versus demucosalization for thin, atrophic labia. Patients with excess AP length in the sagittal plane or a ruffled variant are appropriate candidates for a series of small wedges along the length of the labia (Fig. 4-8). This reduces the length and thus the ruffling and bulkiness to provide a more aesthetic result (Fig. 4-9). A single, more obtuse wedge may suffice; however, tension would be greatest at the point of wedge closure, leaving curled and redundant tissue on either side of the wedge. Very thin, atrophic labia with little submucosa are not amenable to wedge resection, because submucosal sutures tend to tear through, resulting in edge notching and/or fenestrations (Fig. 4-10). Fig. 4-8 This 40-year-old patient has ruffled labia minora excess in the sagittal plane. Fig. 4-9 This 37-year-old patient had redundant labia minora in the sagittal plane. She is shown before and after a wedge labiaplasty. Fig. 4-10 This 32-year-old woman with thin labia minora has fenestrations 8 weeks after a wedge labiaplasty. Funnel-like labia minora that extend radially from a narrow base are a challenging anatomic variation (Fig. 4-11). These may be addressed with a conservative wedge resection or edge resection. In performing a wedge resection, noting the position of the posterior lip is essential. Aggressive wedge resection may result in impingement of the introitus posteriorly and discomfort during intercourse. The web should be released, similar to a small episiotomy, at the time of labiaplasty. This scar tends to be more painful postoperatively because of its location on the perineum. Using a hand mirror, surgeons should point out the posterior labial redundancy preoperatively and describe the additional scarring that will result. Many patients have additional folds of the labia minora superiorly. The fold begins at the confluence of the clitoral frenulum and the labia minora and extends superiorly for a variable distance toward the intervulvar commissure (Fig. 4-12). Patients with a unilateral double fold may not be aware of the fold preoperatively and should be shown the asymmetry during the consultation. Double folds are usually excised in a linear edge resection resulting in a scar in the interlabial groove. The scar tends to heal well, and excising the unilateral fold is typically recommended to prevent asymmetry postoperatively. Fig. 4-12 This 50-year-old woman has a double-fold variant. Patients with large labia minora may have a widened or redundant clitoral hood. Edge trim procedures in these patients may result in a persistence of hood laxity and redundancy and the appearance of a “penis” postoperatively4 (Fig. 4-13). Hunter5 stated that hood redundancy was the most common reason for revision labiaplasty surgery. The extended wedge procedure described by Alter6 addresses the widened clitoral hood through a superior extension of the wedge onto the lateral clitoral hood (Fig. 4-14). The slight tension created by a wedge resection tends to reduce the anterior projection of the clitoral hood, preventing redundancy and the penis appearance.
Labial Reduction: Surgical Wedge Technique
Christine A. Hamori
Key Points
Indications and Contraindications
Indications
Radial Elongation of the Labia Minora


Thickened Labia Minora


Ruffled Variant



Funnel Variant
Double-Fold Variant

Widened Clitoral Hood
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine












