8 Keg to Six Pack: Fat and Cellulite Treatments
Summary
The male demand for cosmetic procedures targeting localized deposits of subcutaneous adipose tissue has grown rapidly over the past decade. Current therapeutic options are less invasive, decreasing downtime and adverse events, while providing a more natural aesthetic appearance. This chapter highlights the numerous available modalities for subcutaneous fat reduction in male patients.
Keywords: noninvasive fat reduction, tumescent liposuction, cryolipolysis, cryoadipolysis, high-intensity focused ultrasound, sodium deoxycholate
8.1 Background
Body contouring procedures are extremely popular, with up to 86% of people surveyed by the American Society for Dermatologic Surgery reporting being bothered by excess weight and 57% of them seeking body sculpting treatments.1 Although men may face less social pressure to seek cosmetic enhancement, they are often motivated by the same desires as women, such as looking as good as possible for their age.2 The male demand for cosmetic procedures targeting subcutaneous adipose tissue has expanded rapidly over the past decade, in part from the growth of less invasive therapeutic options for localized fat reduction with marginal downtime, limited adverse events, and a more natural appearance.3 Between 2012 and 2017, noninvasive body contouring procedures in male patients increased by 60.64%, whereas liposuction decreased by 25.51%.4,5
8.2 Anatomy
Fat distribution is a sexually dimorphic phenomenon, with excess adiposity in men accumulating in the midline (e.g., abdominal and chest), whereas in premenopausal women it collects below the waist (e.g., gluteal, hips, thighs, knees, and calves).6–8 The sex steroid hormone testosterone, analogous to estrogen in premenopausal women, may exert permissive effects on regional fat deposits by regulating the balance between lipid accumulation and mobilization, stimulating the latter in visceral tissue.9,10 Age-related dysregulation of adipocyte lipid metabolism and decreased endogenous testosterone in men in turn leads to progressive abdominal fat deposition viscerally and decreased abdominal fat subcutaneously.11,12 Women also develop central and upper body fat deposits at a later age than men, typically in the postmenopausal period due to a decrease in endogenous estrogen.13 While visceral fat volume in men is 2.6 times that of premenopausal women, it is equivalent to that of postmenopausal women.12
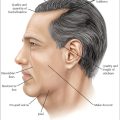
The ideal male abdomen is square shaped with less natural sloping from the midline to lateral aspects and a lower waistline, slightly below the umbilicus, than its female counterpart (Fig. 8.1).14 The male upper body also displays a V-shaped taper from broad shoulders to a narrowed waist. Subcutaneous adipose tissue deposits in the waist and flanks increase waist circumference and decrease this V-shaped tapering.15 Enlargement of the male breast, gynecomastia, either from excess subareolar and lateral pectoral fat—pseudogynecomastia, or subareolar glandular tissue and fat—is cosmetically unpleasant and psychologically distressing.16 On the other hand, fat deposition in the anterior pectoral region, overlying the pectoralis major, can increase chest convexity and give a more masculine appearance.15,17 Excess submental and submandibular fat deposits obscure the strong masculine jawline and leads to a decrease in cervicomental angle.14 Evaluation and marking of any area undergoing treatment should be performed with the patient upright in anatomic position.
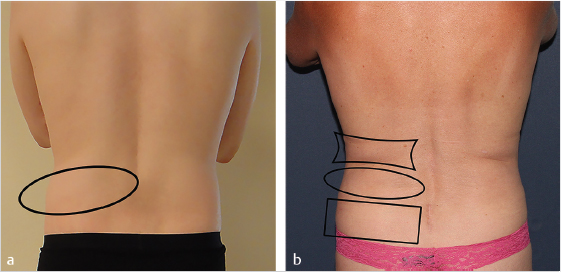
Fig. 8.1 (a) Bilateral male flanks marked by an ellipse. (b) Female hips (rectangle), waist (ellipse), and flanks (polygon). Note the lower waistline in the male patient, with the female waist equivalent to the male flank in anatomic position.
The architecture of the subcutaneous adipose tissue fibrous septa is markedly different between men and women, contributing to the more “firm” or “fibrous” clinical presentation of subcutaneous fat in men.18 Women have a higher percentage of fibrous septa that are perpendicular to the skin surface, while those of men are much more likely to be diagonal or parallel to the skin surface.19
8.3 Approach
Submental, chest, abdominal, and flank subcutaneous adipose tissue deposits are the most common areas of concern for male patients seeking body contouring procedures.20 Available therapeutic options rely on the destruction by cooling, heating, or adipocyte disruption or dissolution, or physical removal by lipoaspiration, of subcutaneous adipocytes.21 While the former techniques lead to subtle results with minimal downtime, the latter is a better option for patients wanting a more dramatic single-treatment result at the expense of a significant period of posttreatment recovery.
Prospective patients with significant visceral fat deposits should be excluded from abdominal body contouring, given that these treatments treat only subcutaneous adipose tissue. Patients with a history of progressive or cyclical weight gain are relatively contraindicated, given their propensity for postprocedure weight gain with suboptimal results. Men with emotional or psychological instability, eating disorders, body dysmorphic disorder, or unrealistic expectations (e.g., seeking immediate results, substantial weight loss, or perfection) are all more likely to be dissatisfied with treatment outcomes and should also be excluded.22
Substantial preexisting laxity of the overlying skin or underlying muscle due to prior rapid weight loss or advanced age may become exaggerated postprocedure. A thorough past medical, surgical, medication, and allergy history must be taken as patients with uncontrolled chronic medical conditions or who are at risk of perioperative bleeding (e.g., due to medically necessary long-term anticoagulation) are best treated with noninvasive body contouring devices. Patients taking medications that inhibit hepatic cytochrome P450 1A2 and 3A4, which interfere with lidocaine metabolism and may lead to toxic elevations in plasma lidocaine concentration, should either be treated noninvasively or stop the implicated medication(s) 1 week prior to tumescent liposuction.23 The most common classes of these medications include antidepressants, antifungals, antivirals, and antibiotics.
8.4 Procedure
8.4.1 Cryoadipolysis
Cryoadipolysis, often incorrectly referred to as cryolipolysis,24 is a procedure cleared by the Food and Drug Administration (FDA) for reducing the appearance of fat bulges in the abdomen, flank, and submental area, among other locations, in nonobese patients. Since adipocytes are preferentially sensitive to cold injury, prolonged cutaneous cooling induces adipocyte apoptosis, triggering a selective, delayed lobular panniculitis and subsequent targeted reduction in superficial subcutaneous fat, without clinical or histologic damage to overlying skin.25,26 Transient pain, erythema, edema, bruising, and numbness are common complaints posttreatment, but alterations in serum lipid levels or liver function tests have not been reported.27,28 Infrequently, intense neuropathic pain may develop several days posttreatment and may respond well to gabapentin or oral analgesics.29 Fortunately, long-term peripheral nerve dysfunction has not been demonstrated.30 Although these concerns have been reported equally among male and female patients, paradoxical adipose hyperplasia—a delayed increase in subcutaneous fat in the treated area that typically begins several months posttreatment—may be more common in men and patients of Hispanic background.31 Hyperplasia or hypertrophy of disorganized adipocytes, perilobular septal thickening/fibrosis, and vascularity are seen on histology. Its etiology remains unclear, but local tissue hypoxia or reduced sympathetic innervation may be inciting metabolic activation of preexisting adipocytes or adipocyte progenitor cells.32
Currently available noninvasive technology utilizes a vacuum to elevate and compress a targeted fold of tissue into a cup-shaped plate for 35 minutes.33 Prior treatment applicators, however, compressed fat within two opposing plates for 45 to 60 minutes at a higher temperature. A 75-minute nonvacuum conformable-surface applicator, with FDA clearance for treatment of thighs, has also been shown to be effective in areas where suction may be limited by anatomy or firmness of tissue, such as the periumbilical abdomen.34 With subjects lying supine, a protective gel pad is draped over the treatment area immediately prior to applicator placement on the abdomen, while the flanks can be targeted with the patient on their side or prone. The applicator may then be secured in place with straps for the entirety of treatment, if needed. Submental cryoadipolysis can also be performed using a smaller applicator and protective liquid gel, with the subject sitting upright and similar straps supporting the device against the submentum.35 At the conclusion of the treatment cycle, the cryoadipolysis applicator is immediately removed, and a manual massage of the treated area is performed. Posttreatment massage has been shown to produce significantly greater reductions in fat thickness due to reperfusion injury.36 Combining cryoadipolysis with radial pulse (shockwave) therapy may also improve results.37
Treatment results are usually modest, with a single application to the flank having been shown to cause a 39.6-mL mean volume loss relative to the contralateral control in a clinical study.38 Double-stacking or overlapping of applicators in the same session may lead to enhanced efficacy without an increase in adverse events.39 A study of two overlapping applicator treatments in the same session for male pseudogynecomastia demonstrated significant improvement in 95% of subjects.16
8.4.2 High-Intensity Focused Ultrasound
High-intensity focused ultrasound (HIFU) uses high-frequency acoustic energy (2 MHz, > 1,000 W/cm2) to rapidly raise adipose temperature above 55 to 58 °C, producing focal coagulative necrosis, while also disrupting adipocyte membranes secondary to mechanical effects (acoustic cavitation).40,41 HIFU devices currently cleared by the FDA are indicated for noninvasive waist circumference reduction and target subcutaneous tissue at a focal depth of 1.3 cm; however, severe periprocedural pain and posttreatment ecchymosis have limited the use of this technology.42
8.4.3 Nonthermal Focused Ultrasound
Nonthermal focused ultrasound (NFU) varies significantly from HIFU by relying solely on adipocyte destruction via low-frequency (200 kHz, 17.5 W/cm2) mechanical disruption.43 NFU is FDA approved for noninvasive reduction of abdominal circumference at a depth of 1.5 cm. This nonthermal approach means dramatically less procedural pain and no downtime posttreatment, but requires multiple sequential treatment sessions for optimal, albeit subtle, results.14 Localized posttreatment adverse events, including pain, erythema, and purpura, are transient and typically minimal.44
8.4.4 High-Intensity Focused Electromagnetic Field Therapy
High-intensity focused electromagnetic (HIFEM) technology has recently been shown to produce muscle fiber hypertrophy and hyperplasia, as well as induce local adipocyte apoptosis, leading to subcutaneous fat metabolism and a local increase in free fatty acids.45–47 A flat applicator is fixed to the abdomen with a belt and each treatment is performed for 30 minutes, with the intensity slowly increased from 0% (ideally to 100%) based on patient tolerance. Four treatments over a 2-week period have been shown to reduce abdominal fat thickness by 19 and 23.3% after 1 and 3 months, respectively.48 Other clinical trials have confirmed reductions in subcutaneous tissue thickness of 18.6% by magnetic resonance imaging (MRI) 2 months after four sessions49 and 17.5% by computed tomography (CT) 1 month after eight sessions, the latter also noting a 14.8% hypertrophy of the rectus abdominis muscle.50 One-year follow-up of subjects treated with HIFEM has demonstrated statistically significant long-term improvement in fat reduction (–14.63%), muscle thickness (19.05%), and diastasis recti reduction (–10.46%).51
8.4.5 Radiofrequency
Radiofrequency (RF) devices create an oscillating electrical field that generates heat from movement and collision of water molecules.52 Since fat has a high electrical impedance and low thermal conductivity relative to overlying dermal tissue, an electrical field directed perpendicular to the skin surface and skin–subcutaneous interface is highly selective for subcutaneous tissue, leading to chromophore-independent thermal damage.53 Purported mechanisms of fat reduction following RF include thermal stimulation of adipocyte metabolism via lipase-mediated enzymatic degradation of triglycerides and adipocyte apoptosis and rupture.54,55
Monopolar, or unipolar, and multipolar mechanisms of RF delivery are currently available for fat reduction, with the latter utilizing high-frequency electromagnetic radiation instead of an electric current to produce heat.56 Trials of monopolar/unipolar RF (with a single electrode) or multipolar RF (three or more electrodes) for fat reduction in male patients, however, are lacking. Nevertheless, volumetric heating of subcutaneous tissue up to 20 mm in depth can be achieved, with optimal results requiring multiple weekly treatment sessions. Newer devices have built-in impedance and temperature monitoring to improve efficacy, safety, and operator dependency.
High-frequency, multipolar field RF has also been shown to produce significant abdominal fat reduction using an operator-independent device. An open-label trial showed a mean circumferential reduction of 4.93 cm in 35 patients after four weekly treatments, although 3 patients did not respond to therapy.57 The body mass index (BMI) was effectively unchanged during the study period, and the best results were associated with subjects who had a higher initial BMI. Approximately 90% of subjects reported no pain with treatment.
Adverse events with RF devices most commonly include treatment-related pain and transient erythema. Posttreatment edema, purpura, postinflammatory hyperpigmentation, subcutaneous erythematous papules, blisters, and superficial burns—although relatively rare—are possible.56
8.4.6 Low-Level Laser Therapy
Although low-level laser therapy (LLLT) has been suggested to disrupt adipocyte cell membranes,58 in vivo59,60 and in vitro21 studies have failed to corroborate this claim. Other purported effects on adipocyte apoptosis via complement activation or lipid metabolism via upregulated mitochondrial cytochrome C oxidase activity remain unvalidated.61 The fact that the majority of photons from 635- or 850-nm LLLT light fail to penetrate into subcutaneous tissue does little to boost claims of subdermal efficacy.21,62 Studies demonstrating improvement in abdominal circumference are compromised by lack of clinical controls, absent weight monitoring, short-term follow-up, or concomitant use of metabolic supplements.63,64,65,66
Nevertheless, LLLT devices are currently FDA approved for circumference reduction of the waist. Treatments are performed two to three times per week, requiring numerous sessions. Devices with light-emitting diode (LED) panels at a preset distance from the skin typically have nearly absent side effect profiles. A study of an LLLT device with LED panels directly approximating the skin in a controlled split-abdomen study showed no significant improvement in ultrasound-measured subcutaneous tissue thickness, but did report two cases of cutaneous ulceration.67
8.4.7 Infrared Diode Laser
A contact-cooled 1,060-nm diode laser device has been shown to produce controlled adipocyte injury by maintaining subcutaneous hyperthermia (42–47 °C), leading to a mean reduction of 18% in caliper-measured targeted fat thickness and 24% reduction in volume by MRI.68 Treatment is performed with up to four rectangular applicators simultaneously for 25 minutes. Studies have shown significant improvement in subcutaneous fat deposits of the abdomen and flanks after a single treatment.69,70 Posttreatment adverse events include tenderness, induration, and erythema.71
8.4.8 Injection Adipolysis
Sodium deoxycholate, or deoxycholic acid (DC), is an animal-derived secondary bile salt and biologic detergent that degrades adipocyte cell membranes.72 Subcutaneous injection of DC produces concentration-dependent local adipolysis and mixed septal and lobular subcutaneous panniculitis composed of inflammatory cells recruited to clear cellular debris and free lipids.73 Fat lobule atrophy and septal thickening/fibrosis are the end result, with the inflammatory cascade characteristically resolving within 1 month postinjection.72,73 Data subanalysis from the two phase 3 pivotal trials in the United States and Canada (Reduced Frequency Immune [REFINE]-1 and -2) demonstrates that 77% of men treated with DC (ATX-101) achieved a clinically significant reduction in submental fat; 79% of men were also satisfied with the posttreatment appearance of their face/chin.74
The submental area is marked, taking care to avoid injecting into the immediate submandibular area, where there is risk of temporary demyelination of the marginal mandibular nerve. Injection points are performed approximately 1 cm apart using a 1-mL syringe and 30-gauge needle, with 0.2 mL of product injected at each point with the needle perpendicular to the skin surface. Using a greater amount of product (three to four vials, 6–8 mL) in the first session may lead to better results early on and encourage patients to complete the treatment series.74 It is expected that less product will therefore be needed with subsequent monthly treatments. Transient injection site pain, edema, numbness, ecchymosis, erythema, and induration/fibrosis are commonly observed postprocedure. Alopecia has been reported from submental injections, but often resolves spontaneously following the end of therapy within several months.75 Intra-arterial DC injection with resulting sludge embolus formation and tissue necrosis is another rare potential complication.76
The effects, and side effect profile, of DC can, however, be tempered with the addition of phosphatidylcholine (PC). PC acts as a physiologic buffer, serving as a vehicle for DC diffusion beyond the injection site via liposome formation, and mitigating the rate of immediate loss of cell viability. Whereas injection of DC leads to immediate cell membrane lysis, the onset of lysis with PC/DC is delayed until 2 weeks postinjection.77 Retrospective studies have confirmed the efficacy and safety of PC/DC in targeting focal areas of abdominal subcutaneous fat after multiple sessions.78
8.4.9 Tumescent Liposuction
Despite the increasing popularity of noninvasive body sculpting devices and injectables, traditional tumescent liposuction remains the gold standard for subcutaneous lipoplasty with unmatched single-session results.79 Predicated on Klein’s tumescent technique, this procedure uses microcannulas to contour subcutaneous adipose tissue comfortably under local anesthesia alone, with minimal postoperative downtime and nominal risk to underlying structures or overlying skin.80,81
Direct percutaneous large-volume infiltration of dilute lidocaine with epinephrine in buffered physiologic saline produces complete, prolonged local anesthesia and hemostasis of cutaneous and subcutaneous tissues, eliminating the need for general anesthesia (Table 8.1).80 The physical compressive effects of interstitial tumescent fluid on subcutaneous capillaries and the vasoconstriction produced by epinephrine combine to slow the systemic absorption of lidocaine, preventing third spacing and virtually eliminating blood loss with lipoaspiration.82 Tumescent lidocaine dosages of 45 mg/kg are exceptionally safe, yielding peak plasma concentrations below levels associated with mild toxicity, regardless of the speed of infiltration.83
Table 8.1 Tumescent anesthetic formulation
Ingredients | Dose (volume) |
0.9% sodium chloride | 1 L |
1% lidocaine hydrochloride | 500 mg (50 mL) for 0.05% 1,000 mg (100 mL) for 0.1% |
1:1,000 epinephrine | 0.65 mg (0.65 mL) for 1:1,500,000 1.0 mg (1.0 mL) for 1:1,000,000 |
8.4% sodium bicarbonate | 10 mEq (10 mL) |
Note: The recommended concentration of lidocaine and epinephrine required per liter for effective tumescent anesthesia varies by body area. The upper and medial abdomen, and chest typically require higher concentrations (1,000–1,250 mg/L lidocaine, 1.0 mg/L epinephrine) than the waist/flanks (750–1,000 mg/L, 0.65–1.0 mg/L) and the lateral abdomen (500–750 mg/L, 0.65 mg/L). | |
The planned treatment areas are first marked with a blue surgical pen, creating a topographic map. Intradermal blebs of anesthetic solution (6-mL syringe, 30-gauge needle,) are injected, through which tumescent fluid infiltration is then started. A variable-rate peristaltic pump is used to rapidly infiltrate subcutaneous tissue by means of a 21-gauge (neck) or 18- to 20-gauge (body) spinal needle. Microcannula entry sites, known as adits, may be either 2-mm incisions (no. 11 blade) or 1.5- to 2-mm-diameter round openings (biopsy punch) placed in the periphery, often in natural skin folds.
Longitudinal movement of a microcannula (12–14 gauge) in a pistonlike in-and-out motion will cause small fat fragments sucked into its aperture(s) to be rasped away from their fibrous stroma and immediately aspirated, creating tunnels within the subcutaneous layer.84 “Pretunneling” with a microcannula not under suction or an Nd:YAG (neodymium:yttrium aluminum garnet) or diode laser device (920–1440 nm) helps break up fibrous subcutaneous connective tissue, which allows for greater and more rapid fat removal. Avoiding large cannulas (or larger microcannulas without pretunneling) also mitigates the risk of subcutaneous irregularities. Removal of repeated small volumes from multiple adits in an overlapping, fanning pattern also optimizes outcomes, especially in more fibrous areas like the abdomen and flanks. A uniform pinch test in the treated area denotes the end of treatment.
Absorbent pads are applied over open entry sites to collect drainage, and the patient is dressed in compression garments to promote drainage, speeding the resolution of subcutaneous edema and induration.85 A high degree of uniform compression should be maintained until 24 hours after drainage has ceased.86 Surgical area pain and tenderness are expected and controlled with a short course of low-dose narcotics followed by over-the-counter oral analgesics. Ecchymosis is generally mild and dependent in nature, often migrating inferiorly. Suctioning of deep fat near the mandibular ramus is avoided in order to decrease the risk of marginal mandibular nerve injury. Adits heal by secondary intention, with perilesional erythema and mild ecchymosis expected in the short term. Bleeding or hematoma formation is only a factor following liposuction of the male breast, albeit rare with high-grade compression.86
Postoperative photos are not taken until 3 to 4 months posttreatment. Whereas liposuctioned areas will resist weight gain, fatty deposits may subsequently accumulate viscerally or in other areas of the body.87
8.5 Before and After Examples
8.5.1 Case 1: Tumescent Liposuction of the Male Chest
The patient is a 38-year-old Caucasian male with pronounced fat deposits of the chest due to weight gain over the last several years, consistent with pseudogynecomastia (Fig. 8.2a). Laser-assisted tumescent liposuction was performed, using 0.1% lidocaine with 1:1,000,000 epinephrine tumescent solution. Approximately 750 mL of subcutaneous fat was aspirated bilaterally with a 12-gauge cannula. A 600–μm laser fiber emitting 1,440-nm (15 W, 50 Hz) energy was utilized prior to suctioning to help emulsify fat. Marked reduction in chest fat deposits is evident at the 3-month follow-up (Fig. 8.2b; the image has been altered to hide the patient’s upper chest tattoo).
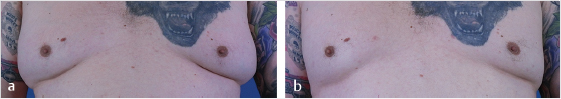
Fig. 8.2 (a) Before and (b) 3 months following laser-assisted tumescent liposuction of pseudogynecomastia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree