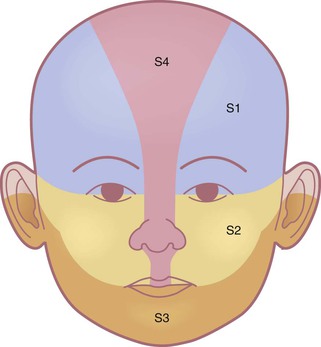
Anita N. Haggstrom, Sarah L. Chamlin Infantile hemangioma (IH) is the most common vascular tumor encountered during early infancy. It is a benign proliferation of endothelial cells that characteristically undergoes a phase of rapid growth followed by slow spontaneous involution. Although large population-based studies are lacking, infantile hemangiomas are estimated to occur in 2.6–5% of infants.1,2 The incidence is highest among Caucasian infants with lower rates in African-American, Hispanic, and Asian infants.3 Females are more commonly affected than males at ratios of 2–3 : 1, with the female-to-male ratio approximately 9 : 1 in patients with segmental hemangiomas associated with PHACE syndrome.4,5 Caucasian race, prematurity and low birthweight are well-established risk factors for the development of IH.3,6 The risk of IH increases by 40% for every 500 g decrease in birthweight.7 A prospective study of over 1000 children with infantile hemangiomas identified additional risk factors, including multiple gestation pregnancies, advanced maternal age, and pregnancies complicated with pre-eclampsia or placenta previa.5,8 Placental abnormalities that impair utero-placental circulation, including retroplacental hematoma, ischemic infarction, dilated vascular communications, vasculitis and chorioamnionitis have been observed to be more common in infants with IH.9 An earlier study reported a threefold increased incidence of hemangiomas in infants born to mothers who undergo chorionic villus sampling, compared with those whose mothers undergo amniocentesis, but subsequent studies have not been conclusive.10 In-vitro fertilization has been suggested as a possible risk factor in one study.2 The majority of hemangiomas arise sporadically; however, a family history can be elicited in some patients, and autosomal dominant transmission has been reported.11 Infantile hemangiomas can be classified based on their location within the skin: superficial, deep, and mixed (superficial and deep). Superficial hemangiomas are the most common type, occurring in approximately 50–60% of cases. Mixed-type IH are estimated to occur in 25–35% of cases, and deep hemangiomas in 15%.12 Superficial hemangiomas are typically bright red with a lobulated surface. These characteristics have led to the use of the term ‘strawberry’ hemangioma. Deep hemangiomas are not commonly noted in the neonatal period, often appearing at 1–3 months of life, or later, as a warm, subcutaneous mass caused by proliferation of the tumor in the deeper portion of the dermis or subcutis. The overlying skin may appear normal or have relatively inconspicuous superficial changes, such as faint blue color, telangiectasias or dilated veins. Mixed-type hemangiomas frequently exhibit a configuration resembling a poached egg, with a well-circumscribed red superficial portion overlying a less well-defined bluish to violaceous deeper component. In addition to characterizing hemangiomas according to their depth and location within the skin, the pattern of involvement is a predictor of prognosis and risk for associated complications.5 Described patterns include ‘focal’, or localized, lesions that appear to arise from a central point, and ‘segmental’ lesions, which typically encompass a larger territory of skin, which in some anatomic sites clearly corresponds to a developmental subunit (Fig. 21.1).13,14 Some lesions are difficult to classify as either focal or segmental and are thus designated ‘indeterminate’. Segmental lesions more often require treatment and are more likely to be associated with complications, including underlying extracutaneous anomalies, including spinal dysraphism, genitourinary anomalies, and PHACE syndrome.14 The patterns of segmental hemangiomas correspond to known embryologic prominences, suggesting a neuroectodermal derivation for their distribution.15 The frontotemporal (S1), maxillary (S2), mandibular (S3), and frontonasal (S4) segments designate commonly observed patterns of facial hemangiomas (Fig. 21.2).15 Infantile hemangiomas have a characteristic clinical course marked by rapid early proliferation, slower late proliferation, a plateau phase, and finally gradual involution. They are either present at birth or appear in the first few weeks of life. Precursor lesions (or so-called ‘premonitory marks’) are seen in as many as 65% of patients and may appear as discrete fine telangiectasias superimposed on a background of pallor, a faint erythematous patch, or a bruise-like area (Fig. 21.3).16 It may be difficult initially to differentiate an erythematous hemangioma precursor from a capillary malformation, but clues include a more ill-defined border, fine telangiectasias, and, if present, skin ulceration. Serial examinations may be necessary to establish the correct diagnosis. Rarely, a hemangioma on the perineum or lip may present in the neonate with ulceration, without an obvious hemangioma, mimicking bacterial or herpetic infection. In these cases, the hemangioma becomes evident over the subsequent days to weeks (see Chapters 10 and 17). In the first few weeks of life, most infantile hemangiomas proliferate rapidly; 80% of superficial hemangioma growth occurs before 3 months of age, with a period of accelerated growth between 5 and 7 weeks of age.16,17 The late proliferative stage is marked by slower growth, but is more variable in its duration, with certain subsets of hemangiomas, including those that are large, segmental, or those with a significant deep component growing much longer, even beyond the age of 1 year.17,18 Most hemangiomas establish the boundaries of their anatomic territory relatively early, growing only in volume thereafter. Superficial hemangiomas initially have a bright red color early in proliferation. Both combined and deep hemangiomas may feel tense, and fluctuations in size and volume may be noted with crying or activity. The earliest signs of involution include a change in color from bright red to a violaceous gray, usually beginning in the center of the hemangioma. The deeper portion also regresses, but this is often not as apparent clinically. Parents may note less fluctuation in hemangioma size during crying and less tumor firmess.6 The warmth of the hemangioma diminishes with time. Some resolve leaving normal or nearly normal skin, whereas others resolve with residua of variable cosmetic significance (Fig. 21.4). Involuted hemangiomas often show residual telangiectasia, pallor or a yellowish color, fibrofatty tissue deposition, and atrophy (Fig. 21.5). Several studies have shown that completion of involution occurs at a rate of approximately 10% per year, with 30% completing involution at 3 years, 50% at 5 years, etc.4,19 Although not specifically mentioned in these studies, it seems that small hemangiomas generally involute sooner than very large, bulky ones. Less commonly, infantile hemangiomas display a more atypical growth pattern characterized by little, if any postnatal growth. These hemangiomas have been variously called infantile hemangiomas with minimal or arrested growth (IH-MAG), abortive hemangiomas, or reticular hemangiomas.20,21 IH-MAG present as telangiectatic patches that have minimal superficial proliferation, often manifested as 1–3 mm red papules at the periphery of the lesion and have a predilection for the lower extremities (Fig. 21.6).22 They may have violaceous to green ectatic vessels underlying the finer telangiectasias. The small proliferative vascular papules involute within the first few years of life but the ectatic vessels can be persistent. The vessels of IH-MAG stain positively for GLUT-1, similar to classic infantile hemangiomas. Ulceration is the most common complication of infantile hemangiomas, occurring in approximately 10–15%, most often during the rapid growth phase. The risk is much higher (approx. 50%) for hemangiomas involving the lip and perineum.23 When the ulceration heals, there is virtually always residual atrophy or scarring. Bleeding may occur, but profuse bleeding is surprisingly rare, occurring mainly with deeply ulcerated hemangiomas or those located on the scalp (Fig. 21.7). Superimposed bacterial infection most commonly with Staphylococcus aureus or Pseudomonas species may develop and may impede healing, but it is uncommon. Recurrent ulceration may complicate hemangiomas located in the perineum. The Kasabach–Merritt phenomenon (KMP) was originally believed to be a complication of large hemangiomas, but studies have proven that KMP is a complication of other vascular tumors, including kaposiform hemangioendothelioma and tufted angioma, rather than infantile hemangiomas (see below). Although the vast majority of hemangiomas are not worrisome and do not necessitate treatment, it is important to recognize the subsets of hemangiomas that are at highest risk for causing permanent disfigurement, impairing vital functions including vision and feeding, and that may be associated with visceral hemangiomatosis or internal anomalies (Box 21.1). The most common reason infants with hemangiomas receive treatment is the potential risk for disfigurement (Fig. 21.8).5 Hemangiomas involving the central face may distort important anatomic landmarks and have a significant impact on future cosmesis. Although exophytic lesions on the medial cheek do not impair vital functions, they are often distressing because of their conspicuous locations and may benefit from more aggressive medical therapies. Distortion of the lip contour can occur even with small hemangiomas because of the disruption of the vermillion border or loss of the curvature of the philtrum. Mixed hemangiomas located on the nasal tip distort the underlying cartilage and leave residual bulk. Surgical repair is often necessary to correct the ‘Cyrano nose’ deformity that can result in splaying of the nasal cartilage. Ulceration involving the columella can lead to destruction of the nasal septum. Hemangiomas on the pinna may ulcerate and become secondarily infected, contributing to structural deformity of the involved ear. Growth of periorbital and lid hemangiomas may cause visual impairment principally by deformation of the cornea, creating refractive errors or less commonly by obstructing the visual axis. If severe or persistent, this can lead to amblyopia. Large and/or segmental hemangiomas in the periocular area have the greatest risk of these complications, but even small lesions may pose a threat to normal visual development, with astigmatism being the most common sight-threatening ocular complication.24,25 Proliferation of retrobulbar lesions may lead to proptosis, strabismus, and visual compromise.26 Large cervicofacial hemangiomas may impair vital functions, distort normal anatomy, or lead to congestive heart failure as they proliferate. These problematic hemangiomas are more common in females than males at a ratio approaching 9 : 1 in some series.27 The term PHACE syndrome refers to the association of posterior fossa brain malformations, hemangiomas, arterial anomalies, coarctation of the aorta and cardiac defects, and eye abnormalities (Box 21.2). The term PHACE(S) is sometimes used when associated sternal anomalies or a supraumbilical raphe are present. Although the exact incidence of PHACE is unknown, it may be more common than Sturge–Weber syndrome.27 In 2009, a multidisciplinary panel of experts published diagnostic criteria for ‘definite’ and ‘possible’ PHACE using specific major and minor criteria.28 A multicenter prospective study of 108 infants with facial hemangiomas measuring 22 cm2 or larger, found that when applying published diagnostic criteria for PHACE, 31% had PHACE and 90% of affected infants had more than one extracutaneous finding. The most common extracutaneous manifestation in PHACE is anomalous cerebrovasculature, with the highest incidence seen in infants with upper face hemangiomas (S1, frontotemporal or S4, frontonasal) (Figs 21.4, 21.9).29 Central nervous system (CNS) anomalies include both structural malformations of the brain and anomalous vasculature of the head and neck, both of which are typically ipsilateral to the cutaneous hemangioma.30 Structural CNS malformations include the Dandy–Walker malformation and other posterior fossa anomalies, such as arachnoid cyst, enlarged fourth ventricle, enlarged cisterna magna, and cerebellar or vermian hypoplasia.31–33 Other CNS anomalies have been reported, including cerebral atrophy, gray matter heterotopia, pituitary abnormalities, and absent corpus callosum. Macrocephaly, ophthalmologic abnormalities, hypotonia, seizures, and psychomotor retardation may be a presenting sign of an underlying structural malformation. Cerebrovascular abnormalities often involve the ipsilateral internal carotid artery and its branches, though other vessels can be involved.30 Dysgenesis of the vessel, including looping, elongation, ectasia, kinking, and focal or fusiform aneurysmal enlargement of the vessel, is most frequently noted.30 Less commonly, vessels can have an anomalous course and/or origin, display narrowing or be completely absent.30 Rarely, patients with intracranial anomalous vessels may demonstrate progressive occlusive arterial changes and cerebral infarction.34 Stroke is a rare complication of PHACE and may be more common in patients with aplasia, hypoplasia or occlusion of a major cerebral artery.35 Other neurologic sequelae of PHACE may include seizures, migraine-like headaches, and developmental delay, including most commonly language and gross motor abilities.36 Cardiac abnormalities, seen in two-thirds of infants with PHACE, usually manifest as unusual forms of aortic arch coarctation, primarily involving long segment narrowing of the transverse aorta often associated with adjacent dilatation or aneurysms.29,37,38 Less frequently, structural anomalies of the heart may be seen, including atrial and ventricular septal defects.28 Less common manifestations include ocular, midline anomalies and hearing loss of the affected ear.39 Ocular findings may include persistent fetal vasculature, retinal vascular anomalies, optic nerve hypoplasia, morning glory deformity, peripapillary staphyloma and coloboma, with other less specific anomalies noted more rarely. Midline defects such as partial or complete sternal agenesis and supraumbilical raphe may also occur.28,40 Endocrine abnormalities, including pituitary dysfunction, thyroid dysfunction, and growth hormone deficiency have been reported in some patients with PHACE. A few infants with PHACE have been noted to have absent or lingual thyroid glands.41–43 Analogous to PHACE syndrome, segmental lumbosacral and perineal hemangiomas can be cutaneous signs of regional anomalies such as underlying structural malformations of the genitourinary, gastrointestinal, neurologic, and skeletal systems (Fig. 21.10).44 The acronyms for this association include LUMBAR, PELVIS, and SACRAL syndromes.44–46 A prospective study of 41 lumbosacral hemangiomas >2.5 cm reported 35% had evidence of spinal dysraphism.47 Tethered spinal cord, spinal lipomas and spinal hemangiomas are the most common underlying abnormalities.48 Imperforate anus, rectoscrotal fistula, renal anomalies, abnormal external genitalia, lipomyelomeningocele, and bony deformities of the sacrum have been reported.44–46 Ulceration is associated with a higher risk of underlying anomalies.47 Multiple hemangiomas occur in approximately 10–25% of infants and are more common in premature infants than in term infants.49 Cutaneous lesions may range in size from a few millimeters to more than several centimeters in diameter. The presence of five or more cutaneous hemangiomas is a known risk factor for extracutaneous hemangiomas, mainly hepatic hemangiomas. Rarely, other organs such as the gastrointestinal tract, lungs, CNS, oral mucosa, and eyes may be affected. Screening ultrasound of the liver is recommended for young infants with five or more cutaneous hemangiomas.50 Serial radiologic evaluation of the liver, especially screening abdominal ultrasound, with further evaluation with CT or MRI, may be necessary to follow progression of visceral lesions. Hepatic hemangiomas (HH) may be solitary or multiple. A classification for hepatic hemangiomas has been proposed, including solitary, multifocal, and diffuse HH.51 Solitary HH in the absence of cutaneous hemangiomas – particularly if detected in utero – are usually GLUT1 negative, regress rapidly, and most likely represent a form of vascular tumor in the liver similar to rapidly involuting congenital hemangioma (RICH) rather than true infantile hemangioma (see below). Multifocal hepatic lesions usually occur in the setting of multiple small skin hemangiomas. They may be completely asymptomatic without the need for treatment, but if they have arteriovenous shunts, they may require liver embolization and/or medical therapy to manage congestive heart failure, as well as hemangioma-specific therapy (such as beta-blockers). Hepatic hemangiomas associated with an arteriovenous, arterioportal shunt or portovenous fistula are associated with greater morbidity.51 Diffuse liver hemangiomas cause massive hepatomegaly, abdominal compartment syndrome, and are associated with hypothyroidism (see below). They have a high rate of mortality and require aggressive medical therapy, and even consideration of liver transplantation. Consumptive hypothyroidism may occur in association with hepatic hemangiomatosis due to the deactivation of thyroxine by a type 3 iodothyronine deiodinase produced by the hemangioma.52–54 This form of hypothyroidism can be detected by the presence of markedly elevated TSH and low T3. T4 levels may be normal or low. Neonatal screening for hypothyroidism is inadequate to assess for this complication, as the most active phase of hemangioma proliferation typically occurs after this period. In some cases, this consumptive form of hypothyroidism may require large doses of thyroid hormone replacement given intravenously. The hypothyroidism typically resolves as the hemangioma regresses, but may have already caused significant morbidity if not detected promptly. Type 3 iodothyronine deiodinase activity has also been found in association with large cutaneous hemangiomas, therefore thyroid function tests should also be considered in patients with large cutaneous hemangiomas.52 Infantile hemangiomas of the airway are most commonly seen in the subglottis and can occur with or without cutaneous hemangiomas. Hemangiomas in the ‘beard distribution’ involving the skin overlying the mandible, chin, and neck, have a high risk of concomitant airway involvement (Fig. 21.11). There is a striking female predilection of 6–7 : 1 for ‘beard’ hemangiomas.55 Though hemangiomas in the mandibular region are most common, other hemangioma patterns that have been associated with airway hemangiomas include unilateral multisegment and hemifacial hemangiomas.56,57 Affected infants typically present within the first few weeks of life with an increasing degree of noisy breathing, stridor, hoarse cry, or other signs of airway obstruction. Having an airway hemangioma together with one or more large facial hemangiomas confers a greater than expected incidence of PHACE – possibly as high as 47%.57 Infantile hemangiomas are believed to represent localized areas of abnormal vascular growth, and several hypotheses have been proposed to explain their pathogenesis. These include endothelial cell defects, a placental origin, extrinsic abnormalities in neighboring cells and exposure to vascular growth stimulators. IH was long thought to be a disease of aberrant angiogenesis, however more recent research supports the idea that it may also represent a disorder of vasculogenesis, that is the formation of new blood vessels de novo, rather than sprouting from pre-existing cells. While some evidence supports many of the proposed hypotheses, no unifying paradigm has emerged: it is likely that the pathogenesis is multifactorial with many mechanisms contributing to their development, proliferation and involution.58–60 Some evidence suggests that hemangioma endothelial cells represent a clonal expansion of cells due to a somatic mutation in genes that play a significant role in vascular growth or vascular regulatory pathways. Mutations in several genes involved in the VEGF signaling pathway (VEGF receptors), Tie-2 and Dusp-5 have been noted supporting this hypothesis, but their exact role in hemangioma pathogenesis is not clear.61–63 Initial analysis of several pedigrees of familial hemangiomas revealed a linkage to chromosome 5q.62 Subsequent analysis of sporadic hemangiomas demonstrated loss of heterozygosity of 5q, further supporting the possibility that somatic mutations play a role in hemangioma formation.64 Infantile hemangiomas share unique immunohistochemical markers with human placenta microvasculature. North and coworkers reported that glucose transporter protein-1 (GLUT-1) is expressed by infantile hemangiomas during all phases of their development (proliferating, involuting, and involuted), distinguishing infantile hemangiomas from vascular malformations and other vascular tumors.65 Other placenta-associated vascular antigens, including merosin, FcγRII and Lewis Y antigen, are also present in hemangiomas and absent in microvessels of normal skin.66 In addition, studies using DNA microarray techniques have revealed that the gene expression profiles of hemangiomas and placenta vascular endothelium are remarkably similar.67 While it is speculated that hemangiomas may arise from embolized placental cells or angioblasts that abnormally differentiate toward a placental phenotype, this is challenged by the finding of negative placental trophoblastic markers in immunochemical analysis of hemangiomas.68 Multiple factors regulate the proliferation and involution of hemangiomas. During proliferation, hemangiomas demonstrate proliferating cell nuclear antigen (PCNA), as well as increased levels of vascular endothelial growth factor (VEGF) and basic fibroblast growth factor (bFGF).69–71 The VEGF signaling pathway is likely one of the more important mechanisms contributing to hemangioma proliferation.72 Angiogenesis mediators, including monocyte chemoattractant protein-1 and the adhesion molecules E-selectin and ICAM-3, are also expressed at high levels.73–76 Proteins involved in extracellular matrix remodeling are expressed during the proliferating phase.59,69,77 Increased levels of urinary matrix metalloproteinase (MMP) proteins are noted in proliferating infantile hemangiomas, suggesting a role in extracellular matrix remodeling, and the expression of lymphatic endothelial hyaluronan receptor-1 (LYVE-1) in proliferating hemangiomas may explain the rapid growth.78,79 Local factors are also believed to play a significant role in hemangioma proliferation. Investigators have noted that hemangioma growth correlates with hyperplasia of the overlying epidermis, with these tissues elaborating angiogenic factors (e.g., VEGF, bFGF). Moreover, these tissues lacked expression of the angiogenesis inhibitor interferon (IFN)-β.80 Indoleamine 2,3-dioxygenase (IDO) enzyme activity may play a role in the transition from proliferation to involution.8,81 During involution, the levels of angiogenic factors found during proliferation decrease, whereas levels of the angiogenesis inhibitor TIMP-1 (tissue inhibitor of metalloproteinase-1) increase.69,75,76 Interferon-regulated genes are upregulated during involution.69,82 Factors that promote apoptosis increase during involution, whereas inhibitors of apoptosis are upregulated during proliferation.83–85 In addition, loss of Dusp-5 function increases apoptosis in human umbilical vein endothelial cells causing speculation for its role in hemangioma involution.72,86 Most infantile hemangiomas can be diagnosed on the basis of history and clinical appearance. The differential diagnosis includes other vascular and nonvascular tumors that are discussed elsewhere. Where history and physical examination are not helpful, further studies such as imaging or even biopsy may be necessary to confirm the diagnosis. Doppler ultrasound and MRI are most helpful in confirming the diagnosis of hemangioma. Doppler studies demonstrate high-flow lesions. T1-weighted MRI sequences demonstrate flow voids as a result of high-flow vessels and enhancement on T2-weighted sequences.87–89 If there is significant diagnostic uncertainty, a biopsy and GLUT-1 staining may be necessary to exclude other soft tissue tumors or vascular malformations. Early in the proliferating stage this tumor consists predominantly of a mass of endothelial cells. Lumina, lined by normal-appearing endothelial cells, become evident somewhat later in the late proliferative phase. PAS stains reveal a thickened basement membrane. Mast cells are increased within proliferating hemangiomas compared to normal tissue. As hemangiomas mature, they show lobules of endothelial channels separated by fibrous septa. Actin-positive smooth muscle cells are deposited around the vessels. Fat cells may be prominent in some involuted hemangiomas. Immunohistochemical analysis with GLUT-1 can be used to confirm the diagnosis of infantile hemangioma. Deep hemangiomas may be particularly difficult to differentiate from other tumors and malformations (Box 21.3 Perhaps the greatest challenge in managing hemangiomas in infancy is the identification of those lesions that need treatment. Because of widely divergent sizes, location(s), and the rapid changes that can occur in early infancy, it may be difficult to predict prognosis at the time of initial evaluation. Frequent assessments during the first few weeks to months of life may be needed, particularly if high-risk features are present. The major goals of management are the prevention and treatment of life-threatening or function-threatening complications of the hemangioma as well as the prevention of permanent disfigurement that may have a long-term social and psychosocial impact on the patient and family (Table 21.1).92 TABLE 21.1 Hemangioma evaluation and management There are a number of treatments employed for infantile hemangiomas, although there is currently no treatment specifically FDA-approved for this indication. There are topical and systemic therapies that target hemangioma proliferation as well as adjunctive therapies that address hemangioma-related complications or the appearance of hemangioma residua after involution. The potential benefits of any form of treatment should be carefully weighed against the associated risks. Several clinical features are important to consider when choosing treatment. It is important to consider not only anatomic location, but also the size, type, and pattern of the hemangioma and whether the hemangioma is actively proliferating. The following sections describe some of the treatment methods that have been employed. This term refers to the active observation and anticipatory guidance that can be given to parents, even if no specific therapy is instituted. Parents may feel significant distress as they await spontaneous involution and may react with disbelief, fear, and mourning. Some feel a degree of social stigmatization and many are accused of child abuse, either jokingly or in earnest. Parent–child interactions may be adversely affected.92 A careful discussion of the natural history of hemangiomas, with photographic examples to demonstrate natural involution, as well as a thorough discussion of therapeutic options, may help allay parental fears. Frequent visits, measurements, and photographs during the proliferating phase are recommended, and as the hemangioma begins to involute, visits can become less frequent. Acknowledgment of the intrusive and unsolicited questions and advice parents may receive can also be helpful.
Infantile Hemangiomas and Other Vascular Tumors
Infantile hemangioma
Clinical subtypes
Natural history
High-risk hemangiomas.
Locations associated with high risk for disfigurement.
Periorbital hemangiomas.
Large cervicofacial hemangiomas and PHACE syndrome.
Lumbosacral hemangiomas and regional anomalies.
Multifocal cutaneous and visceral hemangiomas.
Cutaneous hemangiomas associated with airway hemangiomas.
Pathogenesis
Diagnosis
Histopathology
Differential diagnosis
![]() ).90,91 Infantile myofibromatosis may mimic vascular tumors but is firmer to palpation and has distinct histopathologic features. Infantile fibrosarcoma, a rare tumor that is sometimes congenital, may resemble a deep hemangioma or lymphatic malformation. Rhabdomyosarcoma is the most common sarcoma of early childhood and may present in newborns as a rapidly enlarging red cutaneous mass, usually involving the head and neck, that may be difficult to differentiate from a deep hemangioma. Other benign and malignant tumors that may resemble hemangiomas include adrenal carcinoma, spindle and epithelioid nevi, hemangiopericytoma, dermatofibrosarcoma protuberans, lipoblastoma, neuroblastoma, and nasal glioma. Congenital Langerhans’ cell histiocytosis, multifocal lymphangioendotheliomatosis and disseminated pyogenic granulomas may mimic diffuse neonatal hemangiomatosis. Developmental anomalies such as encephaloceles, dermoid cysts, meningoceles, and teratomas may all be mistaken for deep hemangiomas.
).90,91 Infantile myofibromatosis may mimic vascular tumors but is firmer to palpation and has distinct histopathologic features. Infantile fibrosarcoma, a rare tumor that is sometimes congenital, may resemble a deep hemangioma or lymphatic malformation. Rhabdomyosarcoma is the most common sarcoma of early childhood and may present in newborns as a rapidly enlarging red cutaneous mass, usually involving the head and neck, that may be difficult to differentiate from a deep hemangioma. Other benign and malignant tumors that may resemble hemangiomas include adrenal carcinoma, spindle and epithelioid nevi, hemangiopericytoma, dermatofibrosarcoma protuberans, lipoblastoma, neuroblastoma, and nasal glioma. Congenital Langerhans’ cell histiocytosis, multifocal lymphangioendotheliomatosis and disseminated pyogenic granulomas may mimic diffuse neonatal hemangiomatosis. Developmental anomalies such as encephaloceles, dermoid cysts, meningoceles, and teratomas may all be mistaken for deep hemangiomas.
Management
Hemangioma presentation
Association or complication
Evaluation and treatment
Facial segmental hemangiomas/facial hemangioma >5 cm
PHACE syndrome
MRI/MRA of brain and neck, echocardiogram, ophthalmology evaluation, and consider topical and/or systemic therapy
Periocular hemangioma
Ocular complications
Ophthalmology evaluation and consider topical and/or systemic therapy
Lumbosacral hemangioma
Spinal dysraphism, intraspinal hemangioma, lipoma
MRI of spine or ultrasound spine if neonate, neurosurgical intervention if indicated, consider topical and/or systemic therapy
Perineal segmental hemangioma
Spinal dysraphism and genitourinary anomalies (PELVIS syndrome)
MRI of lumbar spine and pelvis, urological and neurosurgical intervention if indicated, consider topical and/or systemic therapy
Ulceration
Pain, bleeding, scarring
See Box 21.6
Central facial or other hemangiomas distorting normal anatomy
Disfigurement from skin and/or cartilage destruction and deformation
Consider topical and/or systemic therapy
Airway hemangiomas
Respiratory distress
Otolaryngology evaluation and/or MRI of neck, systemic therapy
Multifocal hemangiomas (>5)
Hepatic hemangiomas
Hepatic ultrasound and systemic treatment if symptomatic
Active non-intervention.
Local and topical treatment.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



Infantile Hemangiomas and Other Vascular Tumors
21