CHAPTER 49 Impaction Bone Grafting of the Acetabulum
We have used the IBG technique to reconstruct acetabular bony defects since 1979 and frequently have reported on the clinical outcome in patients with primary THA,1 in young patients,2 in patients with congenital dysplasia of the hip (CDH),3 in revision THA,4 and in patients with rheumatoid arthritis.5 In general the clinical outcomes are favorable, even with long-term follow-up. IBG is not an easy and straightforward technique, and success depends on performance of the technique used by the surgeon. The surgeon should understand the basic principles of the technique. An inferior technique will lead to early instability and migration of the acetabular components We believe that a thorough understanding of the technique of containing and impacting morcelized bone grafts will optimize the clinical outcome for the patients.
Optimal cementation techniques and a proven implant are mandatory.
INDICATIONS AND CONTRAINDICATIONS
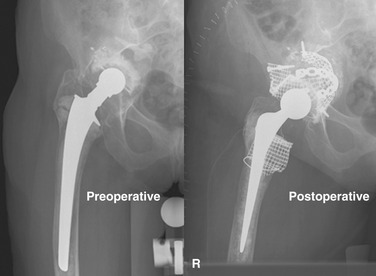
In acetabular revisions with pelvic dissociation it is mandatory to stabilize this pelvic fracture first. Reconstruction of such a dissociation using only flexible wire meshes will fail. Flexible wire meshes do not result in not proper osteosynthesis. The meshes are too thin and flexible, and fixation using small fragment screws is inadequate for the stabilization of the pelvic fracture. Proper pelvic plates and screws must be used to fix and stabilize adequately. Only after the fracture has been fixed can wire meshes be applied to cover the segmental defects and create a cavitary defect that can be filled and impacted with morselized bone chips (Fig. 49-1).
PREOPERATIVE PLANNING
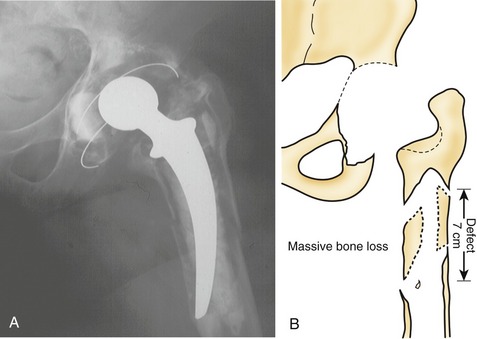
In the planning of revisions it should be realized that bone stock defects and acetabular distortions encountered during surgery are frequently much more severe than the preoperative radiographs suggest. Good-quality plain radiographs in two directions are therefore necessary to evaluate the severity of the anatomic distortion, the location and extent of bone lyses, and, if appropriate, the bone cement distribution. A good rule of thumb is that plain radiographs show only 50% of the reality (Fig. 49-2).